Normal and Abnormal Uterine Bleeding UNC School of Medicine Obstetrics and Gynecology Clerkship
advertisement

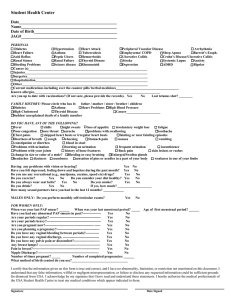
Normal and Abnormal Uterine Bleeding UNC School of Medicine Obstetrics and Gynecology Clerkship Case Based Seminar Series Objectives for Normal and Abnormal Bleeding Define the normal menstrual cycle and describe its endocrinology and physiology Define abnormal uterine bleeding Describe the pathophysiology and identify etiologies of abnormal uterine bleeding Discuss the steps in evaluation of abnormal uterine bleeding Explain medical and surgical management options for patients with abnormal uterine bleeding Counsel patients about management options for abnormal uterine bleeding Normal Menstrual Cycle Normal Menstrual Cycle Basic functional components Hypothalamic-pituitary unit Ovaries Uterus-endometrium Normal Menstrual Cycle Proliferative (Follicular) Phase: Days 1-13 Rise in FSH stimulates maturation of ovarian follicle Follicles secrete estrogen as they mature Estrogen stimulates proliferation of the endometrial lining Endometrium reaches maximum thickness in late follicular phase Level of estrogen peaks on day 12-13, stimulating LH surge on day 14 LH surge stimulates ovulation Normal Menstrual Cycle Secretory (Luteal) Phase: Days 14-28 After ovulation, FSH and LH cause follicle to transform into corpus luteum Corpus luteum produces progesterone which maintains endometrial lining Microvasculature becomes well-differentiated (spiral arterioles) In absence of fertilization the corpus luteum involutes Fall in progesterone triggers menstruation (endometrial sloughing) Normal Menstrual Cycle Normal parameters: Cycle interval: 24 – 35 days Menses: 4 – 7 days Blood loss: 30 – 45 mL Ovulatory bleeding is cyclic and predictable Abnormal Uterine Bleeding: Definition Bleeding that is outside the normal parameters of the menstrual cycle (volume, duration, or interval) Abnormal Uterine Bleeding (AUB): Polymenorrhea: regular cycle interval < 24 days Oligomenorrhea: regular cycle interval > 40 days Menorrhagia: regular blood loss > 80 mL or menses > 7 days Metrorrhagia: irregular bleeding Menometrorrhagia: heavy and irregular bleeding AUB: Etiology Trauma Cervical laceration Foreign body Organic Pregnancy complication Uterine leiomyoma Adenomyosis Endometrial polyp Endometrial hyperplasia Malignancy (cervix, uterus) Dyscrasias Von Willebrand’s Disease Thrombocytopenia Iatrogenic Exogenous estrogen Intrauterine device (IUD) Heparin, Coumadin Systemic Hepatic disease Thyroid disease Hyperprolactinemia Renal failure Other Anovulation (DUB) AUB: Evaluation History Detailed menstrual history (volume, duration, intervals) Symptoms associated with ovulation e.g. breast tenderness, bloating, mood changes Associated symptoms e.g. dysmenorrhea, post-coital bleeding, galactorrhea, hirsutism Weight changes Medical history and medications Pelvic Exam Cervical and vaginal lesions Size, shape of uterus AUB: Evaluation Laboratory Urine pregnancy test CBC with platelets Coagulation studies Thyroid studies (TSH, T4) Prolactin Diagnostic Procedures Pap smear Endometrial biopsy (EMB) Transvaginal ultrasound Hysteroscopy Saline-infusion sonography (SIS) AUB: Management (Medical) Directed at treating the underlying pathology with relief of volume and duration of menses Medical management NSAID’s Combination hormonal contraceptives (e.g. OCP’s, vaginal ring, patch) Levonorgestrel IUD (Mirena) GnRH agonists (e.g. Lupron) Correct medical condition AUB: Management (Surgical) Surgical management Endometrial ablation D&C - IF clinically indicated Myomectomy – IF leiomyomata and fertility desired Hysteroscopic resection – IF polyp, submucous myoma Hysterectomy (TAH, TVH, or TLH) Dysfunctional Uterine Bleeding: Definition Abnormal uterine bleeding with no attributable underlying illness or pathology Diagnosis of exclusion! Must exclude all other causes of AUB DUB: Etiology Anovulation Polycystic ovary syndrome (PCOS) Obesity Adrenal hyperplasia Luteal phase defect (rare) DUB: PCOS Polycystic ovary syndrome (PCOS) Increased circulating androgens aromatize to estrone (E1) Constant, noncyclic, unopposed level of estrogen stimulates growth and development of the endometrium Estrogen provides feedback to pituitary, resulting in low FSH and high LH Static levels of LH trigger chronic anovulation Without ovulation, progesterone-induced changes do not occur Endometrium outgrows blood supply and sloughs at irregular times in unpredictable amounts (usually frequent and heavy) DUB: Etiology Progesterone Estrogen Estrogen 2 4 6 8 10 12 14 16 18 20 22 24 26 28 Menses DUB/Anovulation Ovulatory Cycle DUB: Evaluation Pelvic Exam Cervical and vaginal lesions Size, shape of uterus Laboratory evaluation Urine pregnancy test CBC with platelets Coagulation studies Thyroid studies (TSH, T4) DHEAS and testosterone, if symptoms of hirsutism Prolactin Procedures Endometrial biopsy (R/O neoplasia) Transvaginal ultrasound (R/O anatomic lesions) DUB: Management (Medical) Massive Intractable Bleeding Conjugated Estrogens 25 mg IV Continued Management after Massive Bleeding Conjugated Estrogens 2.5 mg po daily x 25 days Medroxyprogesterone acetate 10 mg for the last 10 days Allow 5-7 days for withdrawal bleed Administer Mirena IUD DUB: Management (Medical) Management of Moderate Menometrorrhagia 1. Estrogen-Progestin Combination Conjugated Estrogen 1.25 mg po daily x 25 days + Medroxyprogesterone acetate 10 mg po for last 10 days OCP x 21 days, with 7 day withdrawal 2. Cyclic Progestin Medroxyprogesterone acetate 10 mg po daily x 10-15 days ea. month Norethindrone acetate 5 mg po daily x 10-15 days ea. month 5 – 7 days menstrual withdrawal should follow cessation ea. month 3. Mirena IUD DUB: Management (Surgical) Patients who do not respond to medical therapy Patients who do not desire future pregnancies Management: Endometrial ablation Hysterectomy Bottom Line Concepts Abnormal menstruation is one of the most common problems dealt with in the gynecologic clinic. Understanding of the physiology and endocrinology of the menstrual cycle is imperative in a thorough evaluation and management of AUB. It is important to rule out unsuspected pregnancies and endometrial cancer in the evaluation of AUB. Irregular bleeding that is unrelated to anatomic lesions of the uterus is referred to as dysfunctional uterine bleeding (DUB/anovulatory). Before DUB can be diagnosed, anatomic causes including neoplasia should be excluded. The primary goal of treatment of DUB is to ensure regular shedding of the endometrium and consequent regulation of menses. In AUB from other causes it is important to correct underlying pathology and decrease volume and duration of menses. References and Resources APGO Medical Student Educational Objectives, 9th edition, (2009), Educational Topic 45 (p96-97). Beckman & Ling: Obstetrics and Gynecology, 6th edition, (2010), Charles RB Beckmann, Frank W Ling, Barabara M Barzansky, William NP Herbert, Douglas W Laube, Roger P Smith. Chapter 35 (p315-319). Hacker & Moore: Hacker and Moore's Essentials of Obstetrics and Gynecology, 5th edition (2009), Neville F Hacker, Joseph C Gambone, Calvin J Hobel. Chapter 33 (p368-370).