Menstrual Disorders
advertisement

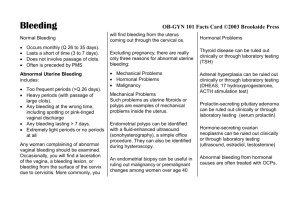
Menstrual Disorders Geetha Kamath, M.D. Dept. of Medicine West Virginia University Definition Normal menstrual cycle involves hypothalamuspituitary-ovary and uterus and is 28 days Vaginal bleeding is abnormal (Abnormal Uterine Bleeding--AUB) when: Volume is excessive or Occurs at times other than expected, including during pregnancy or menopause Known as dysfunctional uterine bleeding (DUB) when organic causes are excluded AUB Duration >7 days or Flow >80ml/cycle or Occurs more frequently than 21 days or Occurs more than 90 days apart or Intermenstrual or postcoital bleeding Terminology Menorrhagia: excessive flow Menometrorrhagia: excessive volume Oligomenorrhea: scanty flow Dysmenorrhea: painful menstrual cycles Causes of Menstrual Disorders Structural Pregnancy associated Hormonal and endocrine Hematologic and coagulation disorders Other Causes--structural Endometrial polyps Endometrial hyperplasia Endometritis Fibroids Intrauterine devices Uterine arterio-venous malformation (AVM) Uterine sarcoma Pregnancy related Implantational bleeding Ectopic pregnancy Spontaneous abortion [incomplete, missed, septic, threatened] Therapeutic abortion Gestational trophoblastic disease Hormonal and Endocrine causes Anovulatory (including polycystic ovary syndrome) Ovarian cyst Estrogen-producing ovarian tumor Perimenopause Hormonal contraceptives Hormone Replacement Therapy Hypothyroidism Hematologic Von Willebrand’s disease (most common inherited bleeding disorder with frequency 1/800-1000) Hemophilia Thrombocytopenia Hematologic malignancies (leukemia) Liver disease Other DUB (dysfunctional uterine bleeding): non-organic causes, either ovulatory or anovulatory Fallopian tube cancer Trauma Foreign body Cervical bleeding--mets, cervicitis, cervical cancer Vaginitis--atrophic, cancer of vagina Endometrial cancer (10% of post-menopausal bleeding) Evaluation of Abnormal Uterine Bleeding (AUB) Acute History suggestive of: Pregnancy and related complications Recent and Heavy bleeding Pelvic pain Medications contributing to above Chronic History: Long standing abnormal menstrual history Symptoms of anemia, hypothyroidism, perimenopause Personal or family history of excessive bleeding AUB Examination Assess vitals/hemodynamic stability Look for features of anemia (pallor, tachycardia, syncope) Look for features of hypothyroidism Look for metabolic syndrome (obesity, hirsutism, acne) Pelvic exam for structural abnormalities: fibroids, pregnancy, active bleeding—uterine vs. cervical bleeding AUB Lab Studies Serum HCG to rule out pregnancy CBC and iron studies to assess severity of anemia TSH for thyroid disorders Coagulation studies (PT, PTT, platelet count, VWF) (primarily for adolescents) Transvaginal ultrasound to look for fibroids and other masses/lesions Endometrial biopsy to rule out endometrial cancer in perimenopausal and chronic anovulatory cycles (primarily for women >35 years with AUB and postmenopausal women) Sonohysterography is useful in diagnosis of anatomical lesions which might even be missed with transvaginal ultrasound Treatment of Chronic Menorrhagia for Most Causes (including DUB) Combined hormonal contraceptives (cyclical or continuous) DMPA (depot medroxyprogesterone) IUD (Intrauterine devices) Treatment options continued After excluding coagulopathy, pregnancy, or malignancy: Progestins Estrogens including oral contraceptives Cyclic NSAIDS Dilatation and curettage (surgical) Endometrial ablation (surgical) Hysteroscopic endometrial resection (surgical) Treatment for Fibroids Surgical: Hysterectomy/myomectomy, uterine artery ablation Medical: Suppression of gonadotropins (danazol and leuprolide) Treatment: progestins Inhibits endometrial growth by inhibiting synthesis of estrogen receptors, promotes conversion of estradiol to estrone, inhibits LH Organized slough to basalis layer Stimulates arachidonic acid production Progestins preferred for those women with anovulatory AUB Progestational Agents Cyclic medroxyprogesterone 2.5-10mg daily for 10-14 days Continuous medroxyprogesterone 2.5-5mg daily DMPA 150 mg IM every 3 months Levonorgestrel IUD (5 years) Estrogens Conjugated estrogens given IV every 6 hours effective in controlling heavy bleeding followed by oral estrogen For less severe bleeding, oral conjugated estrogens 1.25 mg, 2 tabs qid--until bleeding stops NSAIDS Cyclooxygenase pathway is blocked Arachidonic acid conversion from prostaglandins to thromboxane and prostacyclin (which promotes bleeding by causing vasodilation and platelet aggregation) is blocked Clinical Highlights Most common cause of AUB in reproductive age is pregnancy related--so initial evaluation must include pregnancy test. Pregnancy must be ruled out before initiating invasive testes or medical therapy Clinical Highlights Endometrial biopsy is recommended for post menopausal women Or Younger women with history of chronic anovulation >35 years of age Clinical Highlights Uterine cancer and endometrial hyperplasia must be ruled out before medical therapy is initiated in postmenopausal/perimenopausal bleeding NSAIDS may reduce menstrual flow by 20-60% in women with chronic menorrhagia Coagulopathy workup must be initiated in menorrhagia in adolescents References ACOG Practice Bulletin #14, 2000 American Journal Obstetrics and Gynecol 2005;193:1361 Clinical Obstetrics & Gynecology 50(2):324-353, June 2007 Comprehensive Gynecology, 4th edition Harrison’s Principles of Internal Medicine, 14th edition Karlsson, et al, 1995