Urinary Tract Infections MLAB 2434 –Microbiology Keri Brophy-Martinez
advertisement

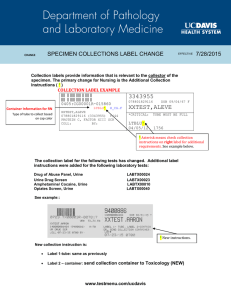
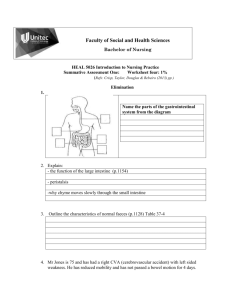
Urinary Tract Infections MLAB 2434 –Microbiology Keri Brophy-Martinez Definitions UTI = Urinary Tract Infection Spectrum of diseases caused by microbial invasion of the genitourinary tract Upper UT includes renal parenchyma (pyelonephritis) and ureters (ureteritis) Symptoms include: fever, flank pain & tenderness Lower UT includes bladder (cystitis), urethra (urethritis), and, in males, the prostrate (prostatitis) Symptoms include: pain on urination, increased frequency, urgency, suprapubic tenderness Bacteriuria = presence of bacteria in urine; may be symptomatic or asymptomatic Anatomy of the Urinary Tract Urinary System Resistant to colonization and infection Characteristics of urine Hyperosmolarity Low pH Very dilute urine fails to grow most bacteria Men have prostatic fluid that is inhibitory Flow has a washing effect Risk Factors: Age Infants Boys have higher incidence rates due to uncircumcision Pre-school age Girls infected more than boys Most renal damage due to UTI at this age School-age children Girls more prone to develop UTI upon sexual activity Risk Factors: Age Adults to 65 Low incidence unless genital-urinary abnormalities Risk Factors: Age Over age 65 UTIs increase dramatically in both genders Atypical presentation • Fever, delirium, failure to thrive Males • Prostate changes & increased catherization • Neuromuscular changes Females • Fecal soiling & increased catherization • Neuromuscular changes • Bladder prolapse Risk Factors: Other Institutionalized care Increase in UTIs • Instrumentation/catherization • Genital-urinary tract abnormalities Pregnancy Renal transplant Risk Factors: Other Urinary conditions High ammonia concentration Lowered pH Decreased blood flow in renal medulla Results in: • Reduced chemotaxis of WBCs • Reduced bactericidal activity of WBCs Clinical Signs and Symptoms Infants and children < 2 years age Children > 2 years Nonspecific symptoms: failure to thrive, vomiting, lethargy, fever Likely to have localized symptoms: Dysuria, frequency, abdominal or flank pain Adults with lower UT infections Dysuria, frequency, urgency, and sometimes suprapubic tenderness Clinical Signs and Symptoms (cont’d) Adults with Upper UTIs Especially those acute pyelonephritis, include LUTI symptoms along with flank pain and tenderness and fever AGN (Acute Glomerulonephritis) Results from immune response to S. pyogenes (Group A) infections, either respiratory or pyodermal • Edema around eyes • Hematuria • RBC and WBC casts Pathogenesis of UTIs Three access routes • Ascending (most significant) • Usually seen in females since ureter is shorter • Descending • Also referred to as Hematogenous/Blood-borne • Occurs as a result of bacteremia • Less than 5% of UTI’s • Lymphatic • Increased pressure on bladder causes a redirect of lymph fluid to kidney • Infection dependent on size of the bacteria, strength of the bacteria present, and how strong the body's defense mechanisms are at the time. • Very rare Flora of Normal Voided Urine Staphylococcus epidermidis Predominant Streptococci Alpha Nonhemolytic Lactobillus species Diphtheroids Yeast Microbial Agents of UTIs Specimen Collection Need to collect specimen to prevent normal vaginal, perianal, and urethral flora Mid-stream clean catch – if self collected, patient needs GOOD instructions Catheterized- sample must come from port NOT bag Suprapubic aspiration ( only for anaerobic culture) Specimen Collection (cont’d) Additives – even with additive, time from collection to processing should not exceed 24 hours Grey top culture tubes( sodium borate) keep sample integrity for up to 48 hours Transport If not processed or preserved, urine should be cultured within 2 hours If refrigerated, urine can be held for 24 hours Preculture Screening Manual screening: Routine Urinalysis Chemical screening • Leukocyte Esterase and Nitrate on urine dipstick Urine microscopic • 5 to 10 WBC/hpf is upper limit of normal • Presence of bacteria Automated methods – expensive, except in large volume labs Gram stains generally not performed on urines Causes for Rejection Inadequate method of collection or transport Labeling incomplete name, source, acc # etc. Insufficient volume Fecal contamination 24 hour urines, pooled urines, and Foley catheter tips must be rejected for culture Setup of Urine Culture Setup 1 Selective agar: MacConkey 1 Nonselective agar: Blood OR Bi-Plate Urine Culture Procedure Inoculation using either a 0.001ml(x1000) OR a 0.01 ml (x100) loop onto selective/nonselective media, such as BAP and MAC Dip calibrated loop into well-mixed urine. Quickly make a single streak down the middle of the BAP with the loop containing urine Streak back and forth across the plate perpendicular to the original inoculum, this creates a “lawn” With the same calibrated loop, do the same with the MAC plate Incubate at 35oC for 24-48 hours Urine Streaking Technique Interpretation of Urine Cultures Is there growth? If no growth: • At 24 hours: • Preliminary report: no growth at 24 hours • Reincubate plates • At 48 hours: • Final report: no growth at 48 hours • Discard plates Interpretation of Urine Cultures If there is growth, what media has it grown on? BAP only: rules out the enteric GNR’s, colonies may be GPC, GPR, GNDC BAP and MAC: most likely an enteric GNR or Pseudomonas. If multiple colony types, a gram stain must be done. Interpretation of Urine Cultures How many colony types are growing? Specimen with ≥ three organisms is probably contamination and should not be identified unless specifically requested by physician One or two pathogens ≥ 100,000 CFU/ml should be identified and sensitivities done One or two pathogens ≥ 100 CFU/ml should be identified only if clinical situation warrants or specimen is catheterized or suprapubic aspiration Determining the CFU Count the numbers of colonies of the plate Multiply that number by the dilution factor of the loop Test YOUR Understanding A clean catch urine is collected from a pregnant patient with symptoms of urinary tract infection. The urine is inoculated onto blood and MacConkey agar with a 0.001 loop. After 24 hour incubation, 72 colonies grew on the blood plate. What is the colony count? Interpretation of Urine Cultures Things to consider in UTI’s Colony count of pure or predominant organism Measurement of pyuria Presence or absence of symptoms References Engelkirk, P., & Duben-Engelkirk, J. (2008). Laboratory Diagnosis of Infectious Diseases: Essentials of Diagnostic Microbiology . Baltimore, MD: Lippincott Williams and Wilkins. https://catalog.hardydiagnostics.com/cp_prod/CatNav.aspx?oid=7405&prodo id=J116 Mahon, C. R., Lehman, D. C., & Manuselis, G. (2011). Textbook of Diagnostic Microbiology (4th ed.). Maryland Heights, MO: Saunders.