Unit 12 Adverse Complications of Blood Transfusion Terry Kotrla, MS, MT(ASCP)BB
advertisement

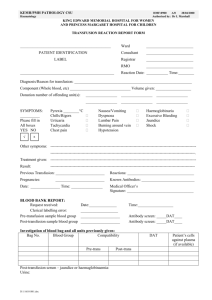
Unit 12 Adverse Complications of Blood Transfusion Terry Kotrla, MS, MT(ASCP)BB Introduction Transfusion of blood and blood components safe and effective way to correct hematologic deficits. Complications during transfusion may occur, called “transfusion reactions” and include broad range of events and problems. Some reactions preventable, some are not. Risk of transfusion must be weighed against benefits. Two categories: Acute or immediate reactions Delayed reactions Clinical Evaluation of Transfusion Reaction Time between reaction and investigation must be as short as possible. Two pronged evaluation Clinical evaluation of patient Laboratory investigation and testing Responsibility of initiation rests with transfusionist. Procedure for Transfusion Blood product picked up from transfusion service. Two licensed personnel check forms against blood product label and patient armband. Take vital signs. Start transfusion. If possible stay with patient first 15 minutes. Retake vital signs to ensure no change. If the same continue transfusion which must be completed within 4 hours, shorter time is preferable, usually 2 hours. Check on patient periodically. Take vital signs upon completion of transfusion What to Watch for During Transfusion Fever Chills Abdominal, chest, flank or back pain Hyper- or hypotension Nausea/vomiting Skin manifestations: urticaria, rash, flushing, pruritus and localized edema. Respiratory distress: wheezing, coughing and dyspnea Jaundice or hemoglobinuria Abnormal bleeding or generalized bleeding (DIC) Oliguria or anuria Pain or burning at infusion site. Shock Actions for Complications Any sign or symptom must be considered potentially life-threatening. Fever and chills may simply be a benign reaction or an indication of acute hemolysis. Two areas of action for the transfusionist: Patient focused steps Component focused steps Patient Focused Steps Stop the transfusion immediately to limit the amount of blood infused and notify a responsible physician. Keep the IV line open with infusion of normal saline. At the patient's bedside perform clerical recheck between the patient and component: check all labels, forms and patient identification to determine if the patient received the intended component. Notify patient’s physician immediately. Component Focused Steps Contact transfusion service immediately. Return discontinued bag of blood, the administration set without the IV needle, attached IV solutions and all the related forms and labels. Send required blood samples, carefully drawn to avoid mechanical hemolysis, to the transfusion service as soon as possible. Send other blood samples for evaluation of acute hemolysis as directed by the transfusion service director or patient's physician. Laboratory Investigation Handle STAT each and EVERY time!! Clerical check identification of patient blood sample, labels, paperwork and donor blood. Repeat ABO testing on the post-transfusion sample. Visual check comparing the patient's pretransfusion and posttransfusion specimen for color of serum or plasma. Perform a DAT on the post-transfusion specimen. If all are negative or normal, nothing further needs to be done. Additional Laboratory Tests for AHTR If DAT positive or hemolysis present in post-transfusion sample additional testing must be performed. Repeat ABO/D on patient pre- and post-transfusion samples as well as donor. Repeat antibody screen on pre- and post-transfusion samples. Repeat crossmatch on pre- and post-transfusion samples THROUGH AHG. If tests on pre-transfusion sample do not match post- transfusion sample notify blood bank supervisor or medical director AND patient’s physician. Investigation for Non-Immune Hemolysis Consider bacterial contamination of the donor unit if: The cells or plasma have brownish or purple discoloration. There are clots or abnormal masses in the liquid blood or segments closest to primary bag appear hemolyzed. The plasma is opaque or muddy. There is a peculiar odor. If any of these are notated set up cultures at 4 C, 20-24 C and 35-37 C and perform a gram stain on the unit. Investigation for Non-Immune Hemolysis Examine the supernatant plasma from the donor blood container for presence of free hemoglobin. Examine the blood remaining in the administration tubing for presence of free hemoglobin. Consider the possibility that the patient or donor has an intrinsic RBC defect such as G-6-PD deficiency or PNH. Consider the possibility of mechanical hemolysis. Consider osmotic hemolysis due to inadvertent entry into the circulation of hypotonic fluids Laboratory Evaluation – Hemolysis Proven Examine post-transfusion urine specimens for the presence of free hemoglobin. Test post-transfusion serum samples for unconjugated bilirubin, carefully recording the timing of sample collection. Peak levels occur at 5-7 hours and disappear within 24 hours. Measure serum haptoglobin in pre- and post-transfusion specimens. Hemolysis Suspected But Tests Uninformative Perform antibody detection tests with more sensitive methods. Perform DAT and IAT daily or more frequently. Measure H&H at frequent intervals to document rise or decrease. Type cells of recipient and donor to find antigens present on donor but absent on recipient. If hemoglobinopathy present perform hemoglobin electrophoresis to verify presence of normal hemoglobin. Acute Hemolytic Transfusion Reaction Triggered by antigen-antibody reaction which activates complement, coagulation systems and endocrine response. Catastrophic clinical events may occur Shock DIC Acute renal failre Life threatening AHTRs almost always due to ABO mismatch. Other blood group incompatibilities may cause hemolysis usually not as severe as ABO. Acute Hemolytic Transfusion Reaction Diagnosis Most common initial sign is FEVER. Reaction may occur with as little as 10-15 mL of incompatible blood. Onset symptoms may be mild: vague uneasiness, abdominal, chest, flank or back pain. First sign patient observes is red or dark urine with or without back pain. Severity directly related to amount of blood transfused. Anesthetized bleeding at surgical site, hypotension or presence of hemoglobinuria. STOP TRANSFUSION, keep IV line open. Therapy for AHTR Goal to treat hypotension and promote renal blood flow. Hemoglobin toxic to kidneys, give fluids to maintain urine output, diuretics to promote urine formation. DIC may occur. Consult with appropriate medical specialist to ensure appropriate treatment. Prevention of AHTRs Impossible Hemolysis may occur even if crossmatch compatible – anamnestic response. Human error Wrong sample from wrong patient. Tech mixed up samples. Blood transfused to wrong patient. SOPs MUST BE FOLLOWED BY EVERYONE. Fatalities must be reported to FDA within 24 hours. Other Immediate Complications Febrile non-hemolytic Transfusion related sepsis Allergic reactions Transfusion associated circulatory overload (TACO) Transfusion related acute lung injury (TRALI) Massive transfusion Febrile non-hemolytic Rise in temperature of 1C or 2F in association with transfusion and no other identifiable cause. Caused by antibodies to transfused lymphs, grans or platelets. Usually occur in repeatedly transfused or pregnant patients. Usually benign BUT may be first sign of AHTR. STOP TRANSFUSION and initiate work up Prevention – pre-storage leukoreduction has decreased incident. Pre-medicate with antipyretics NOT aspirin. Transfusion Related Sepsis Signs/symptoms which occur during or shortly after transfusion. Fever, particularly 101F Shaking chills Hypotension STOP TRANSFUSION IMMEDIATELY – START WORK UP May progress to shock, hemoglobinuria, DIC and renal failure. Platelets most frequently implicated Life threatening sepsis due to platelet transfusion 1 in 100,000 Immediate fatal outcome due to platelet transfusion 1 in 500,000 Transfusion Related Sepsis Bacteria may enter component containers or contaminate port of bag during donor phlebotomy or component preparation. Most common infectious hazard of transfusion. Transfusion Related Sepsis Components from same donation may be contaminated. Platelets most commonly implicated. Transfusion Related Sepsis Each unit must be inspected prior to issue. Quarantine if: Purple color, clots in bag hemolysis, especially sprigs closest to primary bag. Allergic Reactions Urticaria Commonly encountered Characterized by local erythema, hives and itching, usually without fever or other complications. If localized urticaria is the only manifestation, it is usually not necessary to discontinue the transfusion. Etiology unknown Pre-treat with antihistamines. Allergic Reactions Anaphylactic Shock Occurs after the infusion of only a few milliliters of blood or plasma and the absence of fever. Onset characterized by: coughing, broncho spasm, respiratory distress, vascular instability, nausea, abdominal cramps, vomiting, diarrhea, shock and loss of consciousness. Reactions may occur in IgA deficient patients who have developed anti-IgA antibodies after immunization by previous transfusion or pregnancy. STOP TRANSFUSION IMMEDIATELY–START WORK UP Sensitized IgA-deficient patients must be transfused with blood and blood components that lack IgA. Transfusion Associated Circulatory Overload (TACO) Hypervolemia must be considered if dyspnea, severe headache, peripheral edema or other signs of congestive heart failure occur during or soon after transfusion. Rapid increases in blood volume poorly tolerated by patients with compromised cardiac or pulmonary status. Symptoms: coughing, cyanosis, orthopnea, difficulty breathing. STOP TRANSFUSION IMMEDIATELY–START WORK UP For susceptible patients give small volumes SLOWLY. Transfusion Related Acute Lung Injury (TRALI) Number 1 cause of transfusion related deaths. Chest x-ray acute pulmonary edema, acute respiratory insufficiency but no evidence of heart failure. Symptoms of RDS after infusion of volumes to small to produce hypervolemia. May be accompanied by chills, fever, cyanosis and hypotension. Occurs within 6 hours of transfusion, most within 1-2 hours after transfusion. One study 100% of patients require O2, 72% of those require mechanical ventilation as well. Transfusion Related Acute Lung Injury (TRALI) All plasma products have been implicated. Reaction between DONOR leukocyte antibodies and recipient as well as biologically active lipids. WBCs aggregate, trapped in lungs, release cytokines which damage and cause fluid to enter alveoli spaces. STOP TRANSFUSION IMMEDIATELY–START WORK UP Treatment IV steroids and respiratory support. PREVENTION: Do not make plasma products from female donors. Complications of Massive Transfusion Citrate toxicity Hemostatic abnormalities Hyperkalemia Hypocalcemia Air embolism Hypothermia Transfusion-Related Fatalities by Complication, FY2005 through FY2009 TRALI HTR Non-ABO HTR (ABO) Microbial Infection TACO Anaphy Other FY05 29 16 6 8 1 0 2 FY06 35 9 3 7 8 1 0 FY07 34 2 3 6 5 2 0 FY08 16 7 10 7 3 3 0 FY09 13 8 4 5 12 1 1 Delayed Hemolytic Transfusion Reaction (DTR) Two types Due to primary response Due to secondary response DTR Primary Immune Response This is the immunizing event, takes weeks to months. As antibody titer increases in titer and avidity reacts with antigen positive donor cells present. Degree of hemolysis depends on Quantity of antibody present Quantity of antigen positive donor cells present. Usually unsuspected clinically but may suspect based on: Unexplained fall in hemoglobin Positive DAT Appearance of new alloantibody DTR Secondary Immune Response Previously immunized individual. Alloantibodies may fall to undetectable levels. Kidd antibodies most common. Pre-transfusion testing reveals no unexpected antibodies. Within 3-7 days after transfusion anamnestic response Large number of antigen positive red cells present. Rapid increase in antibody titer Symptoms: fever, unexplained fall in hemoglobin, jaundice. RARELY hemoglobinuria and renal failure. Detection of DTR Transfusion service may diagnose if another crossmatch is ordered. Current sample may have positive DAT. Perform elution Identify antibody Antibody screen May be negative, all antibody produced going onto donor rbcs Will become positive once all donor antigens coated. Reason that sample for compatibility testing be no more than 3 days old at time of testing. ALWAYS CHECK PATIENT HISTORY - Once immune antibody identified must ALWAYS give antigen negative blood even if antibody screen is negative. DTR Antibody Screen DAT Initial Negative NA Next Sample Negative Positive- as antibody produced going on to donor rbcs Next Sample Positive – all antigen sites coated, excess antibody detectable Positive Next Sample Positive Negative – no donor cells left Next Sample Negative Negative Infectious Complications Viral hepatitis Cytomegalovirus Malaria Babesiosis Syphilis Chaga’s Disease Toxoplasmosis West Nile Virus Human Immunodeficiency Virus Many more…. Hepatitis Transmission of Hepatitis A rare – fecal-oral route of transmission. All donors screened for Hepatitis B and C but transmission does occur – not through “window”. Defer donor if only unit given patient contracted hepatitis. Defer donor if implicated in two cases. Identified by “look back” Still have non-A, B, C hepatitis transmission Infectious Disease Transmission Cytomegalovirus (CMV) Immunoincompetent/immunosuppressed. Transmitted by leukocytes. All blood pre-storage leukoreduced. Malaria – no screening test available. Very rare but cases are rising. Travel and immigration. Exclude donors at high risk. Report cases to transfusion service or blood provider Infectious Disease Transmission Babesiosis Caused by Babesia species transmitted by ticks. Organism multiplies in RBCs. Donors permanently deferred. Syphilis Caused by Treponema pallidum Donor must be drawn during brief period of spirochetemia. Treponemes can only survive 72 hours at 4C. Serological test for syphilis (STS) negative in primary syphilis. Positive STS indicates high risk life style activities. Infectious Disease Transmission Chagas’ Disease Trypanosoma cruzi transmitted by reduviid bug. Disease primarily found in Central & south America. Few cases reported in Texas and California. Cause of 30% of adult deaths in brazil. Toxoplasmosis Toxoplasma gondii Unusual complication in immunosuppressed Lyme’s disease Borrelia burgdorferi transmitted by tick bite. May be potential problem, no cases reported. Infectious Disease Transmission West Nile Virus Primary reservoir birds, spread by mosquitos. First documented transfusion cases 2002, 23 cases. NAT test used to screen donors. Three month deferral after illness. Humon Immunodeficiency Virus Attempts to prevent transmission rely on careful donor screening and sensitive tests. No cure Transfusions should never be given unless medically necessary. Other Delayed Adverse Affects Transfusion Associated Graft versus Host Disease (TA-GVHD) Rare but usually fatal disease in immunosuppressed. Donor lymphocytes engraft in recipient, consider recipient “foreign”, mount immune response. Pretransfusion irradiation to prevent disease for Intrauterine transfusions Patients identified as being at risk for TA-GVHD Cellular components donated from relatives. Transfusion of HLA selected products. Other Delayed Adverse Affects Post-Transfusion Purpura Rare event occurring almost exclusively in multi-parous women. Precipitous fall in platelet count with purpura about 1 week after transfusion. Some caused by anti-HPA-1a Antigen has 98.3% prevalence, only 1.7% at risk. Antibody destroys not only transfused HPA-1a positive platelets but patients own HPA-1a negative platelets. Thrombocytopenia severe, platelet transfusions no help. Self-limiting. Exchange plasmapheresis for treatment. Adverse Complications of Transfusions Immunologic Non-Immunologic Infectious Alloimmunization TACO Hepatitis Hemolytic Transfusion Rxn Massive Transfusion: Metabolic Hypothermia Febrile Transfusion Rxn Dilutional Pulmonary Microembolism TRALI HIV, HTLV Allergic Transfusion Rxn Syphilis Posttransfusion Purpura Parasites Immunosuppressive Effects CMV, EBV Bacterial End of Unit 12