MLAB 1415: Hematology Keri Brophy-Martinez Hemolytic Anemia: Nonimmune Defects
advertisement

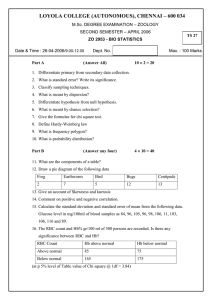
MLAB 1415: Hematology Keri Brophy-Martinez Hemolytic Anemia: Nonimmune Defects Nonimmune Hemolytic Anemia These anemias represent a group of conditions that lead to the shortened survival of red cells by various mechanisms. Causes Antagonists Hemolysis precipitated by either injury to the RBC membrane or to denaturation of hgb Toxins, infectious agents Physical trauma Hemolysis caused by physical injury to RBC Antagonists: Infectious Agents Parasites: Intracellular infections Malaria Carried by mosquito Release of the parasite from the cell causes cell lysis Species of malaria include: Plasmodium vivax P. faciparum - most fatal P. malariae - uncommon P. ovale - uncommon Peripheral smear examination will reveal intracellular parasites Morphology depends on the species Babesiosis Tick-borne Peripheral smear examination will reveal intracellular parasites Resemble tiny rings inside the RBC Antagonists: Infectious Agents Bartonellosis Transmitted by sand fly or direct inoculation by scratch or bite of a mammal Restricted to South America Induces pitting or invagination or RBC membrane Clostridium perfringens Bacteria is OUTside the RBC Exotoxin production affects integrity of host cell membrane Antagonists Venoms Some spiders contain enzymes that lyse the red cell membrane (i.e Brown Recluse) Snake venoms can lysis by: Directly disrupting the RBC membrane Altering RBC membrane to cause complement activation Initiate DIC Physical Injury or Trauma Intravascular and/or extravascular hemolysis Striking abnormal shapes of the circulating blood, such as fragments and helmet cells Physical Injury or Trauma Categories Microangiopathic hemolytic anemia HUS, TTP,DIC, Hypertensive crisis Other physical trauma Burns Macroangiopathic hemolytic anemia Cardiac prosthesis, exercise-induced hemoglobinuria Microangiopathic hemolytic anemias (MAHAs) Fragmentation of the red cells by fibrin strands as they pass through abnormal arterioles. The fibrin strands are the results of intravascular coagulation Damaged RBC cleared by extravascular hemolysis Types of MAHAs Hemolytic uremic syndrome= HUS Thrombotic Thrombocytopenic Purpura= TTP Hypertensive Crisis DIC HUS: Hemolytic Uremic Syndrome Multisystem Disorder Triad of clinical findings Hemolytic anemia with RBC fragments Thrombocytopenia Acute nephropathy Classified based on presence or absence of diarrhea Atypical HUS Found in adults Absence of diarrhea D+ HUS Onset between 6 months- 5 years Majority of cases Presence of diarrhea Pathophysiology of D + HUS 90% of cases associated with Shiga toxin produced by E. coli 0157:H7 Organism enters human GI tract, damages the mucosa and releases toxin Toxin activates the platelets Platelet thrombi trap RBCs and fragment then Platelet thrombi block glomerular vasculature resulting in renal failure D+ HUS Clinical Findings Foul-smelling and bloody diarrhea Onset acute Sudden pallor Abdominal pain Vomiting Jaundice Hematuria Possible acute renal failure TTP: Thrombotic Thrombocytopenic Purpura Platelets and VWF aggregate on the microvascular endothelium As RBC are forced through the aggregates, fragmentation occurs Platelets are removed from the circulation Affects young adults, especially females Systemic infections, autoimmune disorders, and pregnancy are common precipitating factors Lab Features in HUS and TTP Evidence of Hemolysis Decreased H and H Increased reticulocytes/polychromasia Thrombocytopenia Leukocytosis with left shift Schistocytes Evidence of Intravascular Hemolysis Hemoglobinemia Hemoglobinuria Decreased haptoglobin Increased total & unconjugated bilirubin Evidence of Thrombotic Microangiopathy Thrombocytopenia DIC: Disseminated Intravascular Coagulation Bacterial sepsis, neoplasms, immunologic disorders or trauma can precipitate DIC As coagulation is activated, fibrin is deposited in the microvasculature RBC become trapped in the fibrin meshwork and then fragment Due to the clotting process- platelets are consumed Hypertensive Crisis Increase in blood pressure damages endothelial cells Platelets and coagulation factors are activated Fibrin deposits in the vasculature RBCs fragment on the fibrin strands. Peripheral smear shows RBC fragments, low platelet count, mechanism unknown Macroangiopathic Hemolytic Anemias & Burns Cardiac prosthesis (heart valves) RBCs fragment as they pass through prosthetic heart valves Peripheral smear shows RBC fragments, helmet cells and occasional spherocytes March hemoglobinurea/ Exercise-Induced Caused by traumatic destruction of the red cells in strenuous and sustained physical activity such as marching or running Burns Warming RBCs to 49o C induces fragmentation It is thought that the direct effect of the heat on spectrin, causes the red cells to fragment and burst. Spleen clears damaged RBCs within 24 hours of injury Referenes McKenzie, S. B. (2010). Clinical Laboratory Hematology (2nd ed.). Upper Saddle River, NJ: Pearson Education, Inc. Rodak, B. F. (2002). Hematology Clinical Principles and Applications (3rd ed.). St. Louis: Saunders Elsevier.