MLAB 2401: Clinical Chemistry Keri Brophy-Martinez Pathophysiology of Renal Function
advertisement

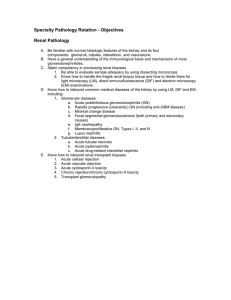
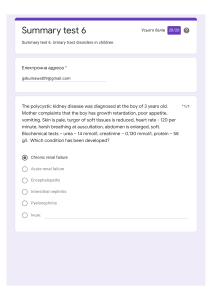
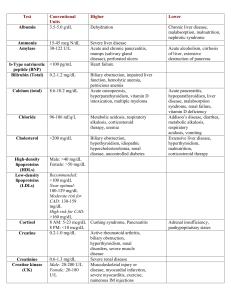
MLAB 2401: Clinical Chemistry Keri Brophy-Martinez Pathophysiology of Renal Function Glomerular Diseases Associated with damage to the glomeruli of the nephron Lead to tubular dysfunction Can be acute or chronic Acute Glomerulonephritis (AGN) Characterized by rapid onset of symptoms that indicate damage to the glomeruli. Population affected includes children and young adults Acute Glomerulonephritis (AGN) Causes of: ◦ AGN often follows a group A streptococcal infection Circulating immune complexes trigger an inflammatory response in the glomerular basement membrane ◦ Toxin/Drug-related exposures ◦ Acute kidney infections ◦ Systemic diseases Acute Glomerulonephritis (AGN) • Symptoms – Hematuria – Proteinuria – Oliguria – Fever – Malaise – Rapid Onset – Edema – Hypertension – Sodium & water retention • Laboratory Findings – Decreased GFR – Increased BUN & creatinine – Hyaline, granular, RBC casts – Increased protein in urine – Blood in urine Chronic Glomerulonephritis (CGN) Associated with the end stage of persistent glomerular damage Irreversible loss of renal tissue Can result in renal failure Symptoms of CGN include: ◦ edema, fatigue, hypertension, metabolic acidosis, proteinuria, decreased urine volume Nephrotic Syndrome Causes of: ◦ Complications of glomerulonephritis ◦ Circulatory disorders affecting kidneys Hallmark ◦ Increased permeability of glomerular basement membrane Allows for proteins & lipids to enter GFR Nephrotic Syndrome Symptoms: ◦ ◦ ◦ ◦ ◦ ◦ Massive proteinuria (>3 g/day) Albuminuria (>1.5 g/day) Pitting edema Hyperlipidemia Hypoalbuminemia Lipiduria: oval fat bodies Urinary Tract Infection • Causes of: – Pyelonephritis (kidneys) • Acute: no permanent damage • Chronic: permanent damage, possible renal failure – Cystitis (bladder) • Lab Findings – Positive nitrite on dipstick – Hematuria – Pyuria – WBC casts Obstructions Causes of: ◦ Renal calculi Calcium oxalate most common ◦ Tumors ◦ Urethral strictures Leads to chronic renal failure Renal Failure Acute ◦ Sudden decline in renal function ◦ GFR < 10 mL/minute ◦ Caused by nephrotoxic agents, necrosis, hemorrhaging Hemolytic transfusions reactions Burns Cardiac failure Antifreeze ingestions Renal Failure: Chronic (CKD) Chronic ◦ Gradual decline in function ◦ Associated with hypertension and diabetes ◦ Risk factors Autoimmune diseases Urinary tract and systemic infections Some medications o Complications from CKD • Anemia • Hyperparathyroidism • Vitamin D deficiency/insufficiency • Mineral and bone disorders Dialysis Method used to rid the body of waste products References 14 Bishop, M., Fody, E., & Schoeff, l. (2010). Clinical Chemistry: Techniques, principles, Correlations. Baltimore: Wolters Kluwer Lippincott Williams & Wilkins. Sunheimer, R., & Graves, L. (2010). Clinical Laboratory Chemistry. Upper Saddle River: Pearson. Vassalotti, MD, J. A., & Kaufman, MD, H. W. (2013, July). New Guidelines to Evaluate and manage Chronic Kidney Disease. MLO, 24-26.