UNIVERSITY OF TENNESSEE MEMPHIS, TENNESSEE Department of Internal Medicine
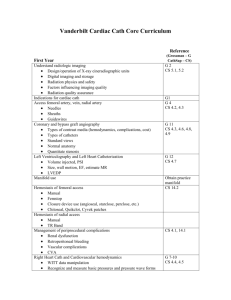
advertisement

UNIVERSITY OF TENNESSEE MEMPHIS, TENNESSEE Department of Internal Medicine Division of Cardiovascular Medicine UT Bowld Hospital CARDIAC CATHETERIZATION LABORATORY Brad S. Burlew, M.D., Director AN INTRODUCTORY MANUAL July 2002 Welcome to the University of Tennessee, Bowld Hospital Cardiac Catheterization Laboratory. It is in this laboratory where you will be taught the fundamentals of hemodynamic assessment, coronary angiography, ventriculography, endomyocardial biopsy, coronary angioplasty, stenting, atherectomy, and occasional other procedures. You will be exposed to patients with ischemic heart disease, acquired valvular disease, congenital anomalies, cardiomyopathies, and pericardial diseases. You will likely also become involved in the placement of temporary pacemakers. Because all of these procedures present very real risks to the patient under study, it is imperative that the fellow fully understands: 1) the indications for the proposed procedure 2) the mechanistic details of the proposed procedure 3) the risk associated with each portion of the proposed procedure 4) which patients, by virtue of their specific diseases have a high risk of complications 5) what should be done to minimize these risks 6) to what extent each patient needs in-patient follow up In view of the above, it should be clear that the performance of a cardiac catheterization involves much more than the procedure itself. As the cath lab fellow, then, you will participate in: A) the initial assessment of the patient, B) clinical stabilization of the patient, if necessary, C) explaining the procedure to the patient and obtaining consent for the procedure, D) performing the procedure, E) post-procedure care, F) data evaluation and reporting G) presentation at angiography conferences. The purpose of this manual is to initially guide you and provide a framework as you learn how to meet these responsibilities. This manual is not at all meant to be comprehensive, but to complement those excellent texts which are already available (see Appendix D). PATIENT RECRUITMENT Patients are referred to the catheterization laboratory from a number of sources, including: 1) Private inpatients and outpatients of UT cardiologists 2) Patients from ER 3) Patients from the Bowld and the Regional Medical Center cardiology services 4) Patients from the Bowld and the Regional Medical Center via a) consult service b) outpatient cardiology clinic It is worthwhile at this point to mention that there is a very strong correlation between the number of cases referred and the perceived enthusiasm of the cath lab fellow. It will pay off in terms of cases referred to you if you communicate often with the senior residents on the floors and with the cardiology fellows responsible for the Cardiology inpatent service and the Consult service. Cath Lab Manual - UT Bowld 1 INDICATIONS for procedure include: (see also Appendix D, Ross et al.): Right heart catheterization; Ventricular dysfunction Valvular heart disease Congenital heart disease To assess pulmonary vascular status, i. e. pulmonary hypertension Left ventriculogram; To assess global function (EF) To assess regional wall motion Mitral Regurgitation Ventricular septal defect Coronary angiography; To assess coronary architecture in patients with: positive non invasive tests stable angina unstable angina new onset angina acute MI and complications poor prognostic indicators post infarction valvular heart disease in older patients prior to surgery cardiomyopathies refractory dysrhythmias To assess graft patency post CABG Asymptomatic patients with: sudden death silent ischemia To assess coronary architecture in congenital anomalies Aortic angiography; Aortic dissection or aneurysm Aortic valvular insufficiency To locate ostia of venous coronary bypass grafts Aortic coarctation Congenital anomalies of aorta Percutaneous Transluminal Coronary Angioplasty (PTCA), stent or Coronary Atherectomy; Hemodynamically significant CAD or disease of venous (or LIMA) coronary bypass graft Endomyocardial Biopsy; Pre transplant evaluation and post-transplant monitoring of heart allograft recipients. Patients presenting with heart failure Patients presenting with arrhythmias Patients presenting with restrictive disease Constrictive pericarditis vs. restrictive cardiomyopathy Cath Lab Manual - UT Bowld 2 RISKS: During the performance of the history and physical, the fellow should also explain to the patient the risk of the procedure as described above, and should obtain written consent for the procedure. The risk of a study is cumulative and depends on the risk of each individual component procedure performed. As a general comment, the risk of "Death or a Major Complication" can be fairly stated as <2% overall. (% risk) COMPLICATION DEATH MYOCARDIAL INFARCTION CVA ARRHYTHMIA & CONDUCTION DISTURBANCE VT V Fib RBBB RBBB c pre-existing LBBB (asystole) 3° AV Block Asystole CARDIAC PERFORATION (especially older females) PERFORATION OF GREAT VESSELS COMPLICATION AT ACCESS SITE Hematoma Surgical exploration/repair Thrombosis (higher in women & ASVC) INFECTION, PHLEBITIS Sones <0.3 0.09-2.6 0.07-.23 Judkins R Heart <0.3 0 0.09-2.6 0 0.07-.23 0 0.1 0.4 0.1 0.4 0.4 0.06 0.4 0.06 0.2 0.2 up to 28 rare 5.4-9.6 <4 ± Biopsy <<0.01 0 0 3 1.3 rare nil 0 0 ≈5 nil 0.2 0.2 0.4 0 0.2 0 >10 0.6-3.6 <1 rare 0 <0.5 rare 0 <0.5 rare rare rare Another complication associated with catheterization is pulmonary edema, which can be a consequence of a new MI, or other factors complicating severe LV dysfunction including the stress of angiographic contrast material and prolonged recumbency. Uncommonly (<<.5% in this laboratory), severe Protamine reactions mimicking anaphylaxis can occur immediately after administration of Protamine sulfate to reverse the effects of heparin. Those at increased risk include patients allergic to fish and diabetics receiving NPH insulin. Dye exposure can induce renal failure, though this is not as common as in the past with the older dyes such as Renografin 76 and Hypaque 76. Predictors of this complication include diabetes, dehydration, azotemia (Cr>2), and myeloma. There are various protocols utilizing volume expansion and diuresis with mannitol drips or furosemide which were designed to protect against acute renal failure. A recent study demonstrated that simple hydration is more effective than diuresis in protecting against dyeinduced nephropathy( see appendix D ). Dye exposure is also occasionally associated with an anaphylactoid (i.e., not IgE-mediated) reaction which cannot be predicted other than by prior occurrence, and even then, a reaction on re-exposure is not certain. Commonly used prophylactic measures are described on the following page. Cath Lab Manual - UT Bowld 3 PATIENT EVALUATION and PREPARATION Once the patient is referred for study, the cath fellow is to obtain the history, perform a physical examination, and review all pertinent data (including prior angiograms, operative reports, etc.) so as to clearly understand the indication for the proposed study and to help plan the procedure. All prior CABG or LIMA procedures must be posted in the lab. The patient should then be presented to the staff invasive cardiologist and the appropriate study proposed. The patient is then scheduled with the cath lab (call 4484195 or write the name and room number on the board) and pre op orders written (see Appendix A). These orders should be written as early in the day as possible, and should include CBC, Prothrombin Time, electrolytes, and EKG. Should abnormalities be detected which may increase the risk of dye exposure, such as hypokalemia, uremia, diabetes, myeloma, dehydration and the like, the patient should be stabilized and prophylaxis initiated. Depending on the likelihood of complications, especially ARF or anaphylactoid dye reaction, appropriate orders and consults (to nephrology) should be written as necessary. The currently accepted protocol for prophylaxis against transient dye-induced renal failure is as follows: Solution: .45 % NaCl Infusion: 1 mg/kg/hr Duration: start 12 hours before and continue for 12 hours after catheterization. Prophylaxis against anaphylactoid dye reaction can be accomplished as follows: Prednisone 50 mg p. o. 12 hr & 6 hr prior to and on call to scheduled cath, Diphenhydramine 50 mg p. o. on call, and Ephedrine 25 mg p. o. on call (except in patients with uncontrolled hypertension or unstable angina). special comments - Angioplasty, atherectomy, stenting, etc. Indications for angioplasty include, but are not limited to patients who are acceptable surgical candidates, and who have limited number of lesions suitable for dilation. Aside from the structural considerations which you will be taught, physiologic consequences of the lesion such as symptomatic angina or a positive treadmill test (± thallium) must be considered. It will be necessary to make arrangements for an ICU bed for patients scheduled for these procedures. Depending on the risk of the procedure, surgical back-up may need to be arranged. This involves contacting the Thoracic Surgery nurse who will then schedule OR time and arrange anesthesia coverage. It is imperative, when possible, to begin antiplatelet therapy BEFORE all elective angioplasties. Typical orders for the interventional patient are included in Appendix A. Cath Lab Manual - UT Bowld 4 special comments (continued) - Same-day cath The "same day cath" is designed for patients who are ambulatory and stable, and utilizes small diameter catheters (5F, 6F) for angiography and ventriculography. The advantage of these smaller catheters is that there is a smaller arterial puncture, a diminished likelihood of hemorrhage and less leg immobility time required. Consequently the patient can expect to be sent home on the day of the test. For this to work, we must have the data available before the patient comes to the cath lab. This can be accomplished by writing the orders (including all lab studies, EKG's, IV's and preps) and submitting these orders THE NIGHT BEFORE to Pre Admission Testing. If the patient is scheduled as a 2nd or 3rd case, it is possible have the labs drawn and run on the morning of the study. After the case is completed, the patient can be observed for 6 hours and if all is well, can be sent home that night. If the patient has a complication after returning home, he should return by ambulance (especially if hemorrhaging) to the Bowld ARA. See Appendix D for a recent study of complications of this technique (Kern et al.). CATHETERIZATION - the study It is in the laboratory where you will learn the most, not so much because your cerebellum merely needs practice to refine your motor skills (which is the most common misconception), but because it is in the laboratory where you must think and think fast! You will discover that you will be called upon to assimilate your clinical expertise, your knowledge of patholophysiology and pharmacology, your knowledge of anatomic subtleties, and your ability to conceptualize in three dimensions. For instance, you will frequently be presented with unexpected congenital anomalies requiring immediate recognition (in this laboratory there are often unanticipated ASD's, coronary anomolies) with proper and complete data acquisition. It is inadequate to merely document an ASD; we need to document which type of ASD is present and which associated anomalies coexist. Even the "routine" (and use that word cautiously) left heart cath will often have hidden traps including access problems, tortuous or aneurysmal vessels, congenitally displaced (and hard to find) coronaries and other unpredictable misadventures in patients who are often marginally stable. Each staff cardiologist will have evolved his/her own individual approach to these various problems; there are many "right" approaches. You are now in the position of being able to observe, question, and sample the techniques of others, and based on how you think, gradually develop your own "style" as a catheteer. Regardless of whom the staff is, the following issues will need to be addressed: 1) Vascular access - the Seldinger technique is very much the standard for nearly all Judkins cases and some Sones. You will quickly master it. On occasion, though, you will assist in the more classic Sones arterial cut down. 2) Right heart cath - aside from the Swan-Ganz catheter with which you are already familiar, you will probably be introduced to the Cournand catheter, the Grollman, the Eppendorf, the transvenous bioptome, temporary pacers, and possibly a transseptal catheterization. Cardiac outputs can be obtained via the thermodilution technique, the Fick technique, the left ventricular angiogram, and indicator dilution techniques (now of only historical interest). Cath Lab Manual - UT Bowld 5 3) Left heart cath - Because of the catastrophic nature of the embolic (clot or air) complications of left heart catheterization, you will need to develop immaculate habits when handling catheters, wires, and injection manifolds. You will initially be introduced to the Judkins catheters for cannulating the coronaries and, depending on your abilities, will be exposed to less easily handled (and more dangerous) catheters such as the Amplatz series and the multipurpose. You will also learn the art of "setting up" the radiologic views so as to obtain the most data with the least amount of dye. 4) After the patient is removed from the laboratory, he continues to require careful attention. At this time, rashes suggesting dangerous reactions to dye or Protamine may be seen, symptoms of incipient pulmonary edema may appear. Of course, if catheters are removed, hemostasis must be achieved; if they are not removed, they must be secured with sutures and dressed. It is important for you to develop expertise in achieving hemostasis by deploying hemostatic devices or holding groins. Do not misinterpret mastery of this responsibility as being beneath you; when your technicians cannot control bleeding, they will come to you. 5) Most importantly, as you concentrate on mastering the manipulation of all of the above mentioned catheters while maximizing data acquisition and minimizing dye and radiation exposure, you can never lose sight of the fact that your patient on the table is extremely vulnerable: watch every heartbeat while catheters are in the heart, watch constantly for signs of impending complications. At the risk of sounding redundant: "THERE IS NO SUCH THING AS A ROUTINE CASE" POST-PROCEDURE CARE In the catheterized patient, follow-up care is usually directed towards management of the vascular access site and towards the management of complications of the procedure, if any. Bleeding represents by far the most common complication of the procedure; it also represents one of the most potentially dangerous. Means of monitoring for and preventing this complication include frequent pulse checks and vital signs, leg immobilization, and follow-up hematocrits. Volume status and renal function must also to be monitored overnight. Even these assessments may prove inadequate for detecting the rare (fortunately) retroperitoneal hemorrhage. The access site is managed according to the technique employed. In the patient who was studied from the groin using the Judkins technique, the dressing is removed during early AM rounds, the site inspected, and a note written documenting the presence of distal pulses or hematomas (including size and location), the color and function of the distal extremity, and the appearance, if any, of any new neurologic dysfunction. If the patient underwent a brachial arterial cut down, arrangements for removal of the sutures in 10 -14 days should be made. At that time, a second note documenting the presence or absence of complications must be written in the patient's record. Cath Lab Manual - UT Bowld 6 DATA PREPARATION CARDIAC OUTPUT Cardiac output has been assessed using a number of techniques over the years including indicator dilution, thermodilution, direct visualization with calculated volumes (LV angiography), and oxygen consumption. Indicator dilution technique is presently rarely used. It is performed by injecting a visible dye into the venous blood as a bolus and continuously recording the concentration of the dye flowing past a sampling site in a peripheral artery. It has the advantage of being able to differentiate between R to L shunts, L to R shunts, and valvular regurgitation. Thermodilution is a variation on the indicator dilution technique, using iced saline as the indicator dye, and measuring the thermal response in the blood flowing past a sampling site in a pulmonary artery. Consequently, blood flow through the right heart is measured. This is currently the most commonly used technique. Unfortunately, it cannot differentiate between the various shunts as indicator dyes can. The accuracy of this method is diminished in the settings of tricuspid insufficiency and pulmonic regurgitation. In this laboratory, the left ventricular cardiac output is calculated using images stored in the laboratory computer or by using the Vanguard cine projector. Outlines of the ventricular cavity are drawn in systole and diastole, volumes are calculated, and based on heart rate, cardiac output is determined. Of course, in the normal state, the right heart, left heart, and total forward systemic flows are all identical Total forward systemic circulation can be calculated based on the Fick equation. If the patient's oxygen consumption, mixed venous oxygen content, and arterial oxygen content can be determined, the total systemic forward flow can be calculated. The best way to accomplish this is to actually measure the oxygen consumption by having the patient breathe air in a metabolic hood (Waters MRM2) and to sample mixed venous and central aortic oxygen saturations. An approximation can be made by looking up the oxygen consumption index (OCI) based on age, gender, and HR, and calculating rather than measuring the oxygen consumption (see pg. 8). --Equations used to calculate cardiac output by the Fick equation.-VO2 = oxygen consumption: measured or determined from assumed OCI (pg. 8) Oxygen content = 1.39 x [Hb] x SO2 + .0031 x PO2 where [Hb] is the concentration of hemoglobin of the sample (g/dl) SO2 is the saturation of the hemoglobin sample (≤1.0) PO2 is the partial pressure of O2 in the blood (torr) CaO2 = arterial oxygen content = 1.39 x [Hb] x SaO2 + .0031 x PaO2. CvO2 = central venous oxygen content = 1.39 x [Hb] x SvO2 + .0031 x PvO2. VO2 Oxygen consumption ml/min Cardiac output = Arteriovenous oxygen difference = Ca -Cv O2 O2 ml/100cc = 1.39x[Hb]x(Sa VO2 O2-SvO2)+.0031x(PaO2-PvO2) Cath Lab Manual - UT Bowld 7 OXYGEN CONSUMPTION INDEX (ml/min)/m2 BY SEX, AGE, AND HEART RATE Heart Rate (beats/min) Age (yr.) 50 60 70 80 90 100 110 120 130 140 150 160 170 141 136 134 132 130 129 127 126 124 122 120 119 149 144 141 139 136 134 132 131 130 127 125 124 122 155 152 148 145 142 140 137 136 135 134 131 129 127 126 159 156 151 148 146 144 142 141 139 137 135 133 131 130 163 160 155 152 149 147 146 144 143 142 139 136 135 133 167 163 159 156 153 151 149 148 147 145 143 141 139 137 171 168 162 159 157 155 153 152 150 149 147 145 143 141 175 171 167 163 160 158 157 155 154 153 150 148 147 145 178 175 171 167 165 162 160 159 157 156 154 152 150 149 182 179 174 171 169 167 165 162 161 160 157 155 186 182 178 175 172 170 169 167 166 165 190 186 181 178 176 174 172 130 125 122 119 116 114 111 109 106 103 100 98 141 134 129 125 122 120 118 116 114 109 106 104 102 150 145 137 133 129 126 123 121 119 118 114 110 107 105 153 149 142 136 133 130 127 125 123 121 118 115 111 109 157 152 146 141 136 133 131 128 127 125 121 118 116 112 161 156 149 144 141 137 134 132 130 128 125 122 119 117 165 159 153 148 144 141 136 133 134 132 128 125 123 121 169 163 156 152 148 145 143 140 137 136 132 129 127 124 172 168 160 155 152 149 146 144 142 140 136 133 130 128 176 171 165 159 155 152 150 148 146 144 140 136 180 175 168 163 159 156 153 151 149 148 183 179 172 167 163 160 157 Males 3 4 6 8 10 12 14 16 18 20 25 30 35 40 130 128 127 125 124 123 120 118 116 115 Females 3 4 6 8 10 12 14 16 18 20 25 30 35 40 118 115 112 109 107 106 102 99 97 94 This table is useful for estimating oxygen consumption (VO2) as follows: 1 2 Obtain body surface area from facing page (using height and weight) Oxygen consumption = OCI x BSA Cath Lab Manual - UT Bowld 8 ANGIOGRAPHY General - During the performance of the procedure, the operator is constantly assessing the degree and location of coronary artery disease. While the case is in progress, the various lesions must each be demonstrated in at least 2 orthogonal (at right angles to one another) views. ORTHOGONAL VIEWS postero-anterior vs. lateral right anterior oblique vs. left anterior oblique right anterior oblique, cranial vs. left anterior oblique, caudal right anterior oblique, caudal vs. left anterior oblique, cranial Special views such as lateral with cranial (axillary) or caudal angulations are often helpful to isolate otherwise difficult to demonstrate lesions (See facing page). It is also often useful to focus down (4" view or "double-mag") and magnify the lesion, especially with severe L main or LAD stenoses. During the actual filming of the angiogram, because the optimal area of focus is in the central portion of the screen, one should start the cine with the proximal portion of the vessel centered, then should "pan" or move the table so that the more distal portions of the vessel are well seen. Panning should be limited as much as possible or avoided altogether. If a lesion is being magnified for special evaluation, it is best to center the lesion first during the cine. Finally, it is preferred to start the injection of dye a brief period of time (such as one heartbeat) after the beginning of the cine. This allows electronic equilibration of the focusing and contrast circuits of the equipment, and also allows assessment of the degree of calcification of the vessels and of the coronary flow dynamics present. After the film has been developed, each artery needs to be defined in terms of specific anatomy and in terms of localization (see facing page) and severity of lesions. Each artery (the left main: LM, the left anterior descending: LAD, the circumflex: Cx, and the right coronary: RCA) needs to be described. The presence or absence of a ramus intermedius and the dominance of the posterior circulation needs to be defined. An artery (RCA Vs Cx) is deemed dominant if it feeds the diaphragmatic portion of the heart via the posterior descending artery (which takes off opposite to the A-V nodal artery). After determining the major anatomy, the lesser vessels need to be assigned; the conus branch (originates from a separate ostium about half the time) and the acute marginal branches feeding the RV free wall are branches of the right, the septal perforators and the diagonal branches are from the LAD, and the obtuse marginals originate from the Cx. The posterior descending artery (PDA) originates from the RCA in around 85% of people, from the Cx in about 8%. In the remainder of patients, there is a codominant or balanced system, with the inferior septal perfusion coming from the terminal branch of the RCA and terminal posterolateral branches of the Cx. Once the anatomy is defined, the location and severity of lesions need to be determined. Lesion location is described using the above mentioned terminology. The severity of a lesion is Cath Lab Manual - UT Bowld 9 communicated quantitatively in terms of percent decrease in vessel internal diameter. It is also useful to qualitatively describe distal flow in terms of TIMI Grades (see below). One of the most common errors is for an angiographer to "estimate" the degree of stenosis. DON’T DO THIS. There are plenty of studies demonstrating very poor correlation between estimated and measured stenoses. Don't try, you'll be wrong. In this lab, every lesion is to be measured manually with calipers, or using our computer-assisted quantitative angiography. Definitions of perfusion in the TIMI trial Grade 0 (no perfusion): There is no antegrade flow beyond the point of occlusion. Grade 1 (penetration without perfusion): The contrast material passes beyond the area of obstruction but “hangs up” and fails to opacify the entire coronary bed distal to the obstruction for the duration of the cineangiographic filming sequence. Grade 2 (partial obstruction): The contrast material passes acoss the obstruction and opacifies the coronary bed distal to the obstruction. However, the rate of entry of contrast material into the vessel distal to the obstruction or its rate of clearance from the distal bed (or both) are perceptibly slower than its entry into or clearance from comparable areas not perfused by a previously occluded vessel –– e.g., the opposite coronary artery or the coronary bed proximal to the obstruction. Grade 3 (complete perfusion): Antegrade flow into the bed distal to the obstruction occurs as promptly as antegrade flow into the bed proximal to the obstruction, and clearance of contrast material from the involved bed is as rapid as clearance from an uninvolved bed in the same vessel or the opposite artery. VENTRICULOGRAPHY Cardiac ventriculography, especially left ventriculography, is performed to evaluate global and segmental ventricular function, and to detect abnormalities such as asymmetric hypertrophy and VSD's. It is usually performed in the RAO (and often LAO) projection using a 7 or 8F pigtail catheter. Other catheters used include the multipurpose, the NIH, Eppendorf, Lehman ventriculography, and the Grollman R ventriculography catheters. After setting up the LV gram, the cine is performed while injecting a minimal but effective bolus into the LV over several seconds. Typical flow rates are on the order of 10 - 15 cc/sec for 3 seconds. Pigtails are quite useful because the geometry permits high flow rates without a "fire hosing" effect (where the catheter whips around inside the heart during the injection because of a jet reaction at the hole at the tip of the catheter). Multiple side hole catheters are second best because the dye escaping from the side holes lessens the jet reaction. If the jet is severe enough, it can actually cause dye to burrow into the myocardium and cause "staining" (not acceptable). For this reason, end-hole catheters should be used with lesser rates of injection (8 - 12 cc/sec) after carefully placing the catheter along the long axis of the ventricle, as far away from endocardium as possible. Once performed, the ventriculogram is evaluated on the cine projector by entering the data requested by the computer and following the instructions to trace the end-diastolic and systolic ventriculograms. The laboratory computer can also be used to give you information regarding the global and regional (see facing page) ventricular function. Cath Lab Manual - UT Bowld 10 Hemodynamic Calculations - Oximetry SHUNTS (See chapter on "Shunt detection and Measurement" in Grossman text) The presence and extent of shunting is usually expressed as the ratio of pulmonary to systemic blood flow: Qp/Qs. Normally, pulmonary blood flow(Qp) is very nearly the same as systemic blood flow (Qs), the trivial difference being accounted for by the physiologic shunt (coronary and bronchial blood drains into the left ventricle & atrium or pulmonary veins). As already described in the cardiac output discussion, VO2 Oxygen consumption Cardiac output = Arteriovenous oxygen difference = Ca -Cv O2 O2 This concept is used to determine the flow across the systemic capillary bed: VO2 Qs = Ca -Cv O2 O2 and the pulmonary capillary bed: VO2 Qp = CPV -CPA O2 O2 where: VO2 = oxygen consumption (measured or calculated) CaO2 = systemic arterial O2 content (measured from aorta) CvO2 = mixed venous O2 content (must be measured in chamber immediately proximal to site of shunt - see below†) CPVO2 = pulmonary venous O2 content (measured from pulmonary vein, systemic artery if PaO2≥95%, or assumed to be 98% if PaO2<95% and R to L shunt is demonstrated) CPAO2 = pulmonary arterial O2 content (measured from PA) † LOCATION OF O2 STEP-UP USE CvO2 FROM Pulmonary artery (i.e., PDA) Right Ventricle Right Ventricle (i.e., VSD) Right Atrium Right Atrium (i.e., ASD) CvO2 = CO2 (IVC)+3xCO2(SVC) 4 In the setting of suspected congenital heart disease or acquired septal defects, the "sat run" needs to be fairly extensive to increase the likelihood and precision of localizing the shunt. Samples obtained in such a case should include: Superior Vena Cava- high Inferior Vena Cavahigh Pulmonary Artery-main PA low low selective (R or L) Right Atrium - high Right Ventricle inflow "Wedge" saturation (optional) middle outflow Left Ventricle low Aorta Compared to the complete sat run, the great majority of your cases will be abbreviated. "Screening" sat runs are part of the routine right heart cath when a pathologic shunt is not suspected. In these cases, single samples drawn from the IVC, mid RA, RV and PA are sufficient. Cath Lab Manual - University of Tennessee / Bowld Hospital Page 11 Hemodynamic Calculations - Oximetry By way of example, Fig. 1 (facing page) demonstrates the saturation run measured in a patient with an atrial septal defect. In this example, [Hb] = 12 g/dl CaO2 = systemic arterial O2 content = 1.39 x [Hb] x SO2 + .0031 x PO2 = 1.39 x 12 x .96 + .0031 x 92 (using SaO2 measured from aorta of 96%, PaO2 of 92 mm Hg) = 16.01 + .28 (note the 1.7% contribution (.28/16.01) from the plasma) = 16.3 CO2(IVC)+3xCO2(SVC) CvO2 = mixed venous O2 content = 4 CO2(IVC) = 1.39 x 12 x .73 +.0031x51, (using SO2(IVC) = .73, PO2(IVC) = 51mm Hg) = 12.17 +.15(again note the trivial contribution from the plasma) = 12.32 CO2(SVC) = 1.39 x 12 x .68+.0031x48, (using SO2(SVC) = .68, PO2(SVC) = 48mm Hg) = 11.34 +.15(ditto) = 11.49 CvO2 then, = CO2 (IVC)+3xCO2(SVC) 12.32+3x11.49 = = 11.70 4 4 To demonstrate the relative contribution of the .0031 x PaO2 factor, I will now ignore the trivial contribution from the plasma and calculate the CvO2 using: CvO2 = CO2 (IVC)+3xCO2(SVC) = 4 .73x(1.39x12)+3x.68x(1.39x12) .73+3x.68 = x(1.39x12) 4 4 =.6925x(1.39x12)= 11.55 ( a 1.3% error compared to 11.7). Clinically, the .0031 factor is often ignored in patients with physiologic PO2's, and in this manual, will be henceforth ignored. CPVO2 = pulmonary venous O2 content = 16.01 (measured from systemic artery in this case) CPAO2 = pulmonary arterial O2 content (SPAO2 = 80%) = 1.39 x 12 x .80 = 13.34 VO2 Qp = CPV -CPA O2 O2 VO2 and Qs = Ca -Cv O2 O2 VO2 Qp CPVO2-CPAO2 CaO2-CvO2 = CPV -CPA (VO2 cancels out) Qs = VO2 O2 O2 CaO2-CvO2 Qp/Qs = (16.01 - 11.55)/(16.01 - 13.34) = 4.46/2.67 = 1.67 Cath Lab Manual - University of Tennessee / Bowld Hospital Page 12 Hemodynamic Calculations - Oximetry The next example, Fig. 2 (facing page) demonstrates the saturation run measured in a patient with a large ventricular septal defect. In this example, [Hb] = 14.2 g/dl, and again, the O2 content of the plasma will be ignored. CaO2 = systemic arterial O2 content, (using SaO2 measured from aorta of 96%, PaO2 of 92 mm Hg) = 1.39 x 14.2 x .97 =19.14 CvO2 = mixed venous O2 content measured from the RA (average of samples=66%) = 1.39 x 14.2 x .66 = 13.03 CPVO2 = pulmonary venous O2 content =19.14 (measured from systemic artery) CPAO2 = pulmonary arterial O2 content (SPAO2 = 88%) = 1.39 x 14.2 x .88 = 17.36 VO2 VO2 Qp = CPV -CPA and Qs = Ca -Cv O2 O2 O2 O2 Qp CaO2-CvO2 Qs = CPVO2-CPAO2 (VO2 cancels out as before) Qp/Qs = (19.14- 13.03)/(19.14 - 17.36) = 6.11/1.78 = 3.43 Bi-directional shunts must be assessed in various complex congenital anomalies involving admixture of blood from both sides of the circulation. In the figure to the right, the L R shunt is the difference between the total pulmonary blood flow and the effective pulmonary flow (PBF-EPBF). Likewise, the R L shunt is the difference between the systemic blood flow and the effective pulmonary flow (SBFEPBF). The calculation of the bi-directional shunts can therefore be accomplished with oxygen content measurements: PBF (Qp) EPBF RL EPBF RL L R shunt = PBF-EPBF VO2 VO2 = CPV -CPA - CPV -CV O2 O2 O2 O2 R L shunt = SBF-EPBF VO2 = Ca -Cv O2 O2 VO2 - CPV -CV O2 O2 Cath Lab Manual - University of Tennessee / Bowld Hospital Mixed Venous Return SBF (Qs) Page 13 Hemodynamic Calculations - Gorlin formula VALVE REGURGITATION The quantitation of valvular insufficiency is a relatively straightforward procedure which requires the quantitation of: a) the left ventricular stroke volume or cardiac output as measured by angiography b) the actual forward flow (stroke volume or cardiac output) as determined by thermodilution or Fick. c) The regurgitant fraction = (a - b) / a In a simple example, a patient with severe AI has an otherwise normal heart. On angiography, the stroke volume is calculated as 132 ml. and her pulse is 107. The thermodilution cardiac output is 3.2 L/min. In this case, a = .132 x 107 = 14.1 L/min. The regurgitant fraction = (14.1- 3.2) /14.1 = 10.9/14.1 = 77.3% (not good!) VALVE STENOSIS The quantitation of valvular stenosis requires the application of several measured or derived parameters into the Gorlin equation with the empiric orifice constant corrected for the appropriate valve. These parameters include: 1. The measured SYSTOLIC EJECTION PERIOD 2. The TOTAL SYSTOLIC CARDIAC OUTPUT, which in face of valvular insufficiency is not the thermodilution CO, but the total systolic forward transvalvular flow, often best approximated by the angiographically derived Stroke Volume x Heart Rate. This parameter is even harder to determine in combined Aortic and Mitral regurgitation. 3. The CALCULATED MEAN SYSTOLIC TRANSVALVULAR GRADIENT. Gorlin equation: Valve Area = Flow C x 44.3 P1-P2 Flow = , where: Cardiac output(ml/min) DFP or SEP DFP = Diastolic filling period per minute (Diastolic filling time/beat x HR) SEP = Systolic ejection period per minute (Systolic ejection time/beat x HR) C = empiric orifice constant: for semilunar (aortic, pulmonic) valves, patent ductus, septal defects; C=1 for mitral valve calculations using DFP derived from PA catheter Vs LV; C = 0.85 for mitral valve calculations using DFP derived from arterial pressure tracing; C = 0.7 P1-P2 = CALCULATED MEAN TRANSVALVULAR GRADIENT. This, as described on the next page, is derived by physically measuring with a planimeter the area on the pressure tracing best representing the transvalvular gradient, and dividing by the linear dimension on the tracing which represents the duration of the gradient (DF time or SE time for that heartbeat). Cath Lab Manual - University of Tennessee / Bowld Hospital Page 14 Hemodynamic Calculations - Gorlin formula MEASURED PARAMETERS, using a case of aortic stenosis as an example, are obtained directly from the pressure tracings as follows: 1) Using tracing paper or any paper through which you can easily see underlying print draw near the bottom a horizontal line representing the baseline P=0. Matching this exactly with the baseline of the pressure tracing, trace several cycles of the LV pressure curve as shown below: 2) In a similar fashion, trace the aortic pressure tracing, being careful to exactly match the baseline and the systolic/diastolic periods. If there is a dichrotic notch, it will help you align the tracings properly: Cath Lab Manual - University of Tennessee / Bowld Hospital Page 15 Hemodynamic Calculations - Gorlin formula 3) Using the planimeter, measure the area representing the systolic transvalvular pressure gradient (shaded): The area obtained in this example is 5.125 cm 2, which can be conceptualized as a rectangle with the base representing the systolic ejection period in milliseconds and the height representing the mean systolic transvalvular pressure gradient in mm Hg. It follows then that the way to calculate the mean systolic transvalvular pressure gradient is to measure the shaded area in cm 2 with the planimeter (5.125cm2) and divide by the systolic ejection period measured directly off the pressure tracing in centimeters (2.33 cm). This will yield a linear dimension (2.2 cm height) which, when compared to the scale of the pressure tracing (200 mm Hg calibrated over 10 cm total vertical span, or 20 mm Hg/vertical cm), will convert to the mean systolic transvalvular pressure gradient in mm Hg (44 mm Hg in 5.125 5.125 sq. cm. this example). Likewise, assuming a paper feed speed sq . cm. of 50 mm/sec, each horizontal centimeter (or 10 mm) represents 200 mSec, and the systolic ejection period is 466mSec (2.33 cm x 200 mSec/cm). 4) Calculate the valve area with the Gorlin formula using a. b. c. d. CO = 5.1 L/min (thermodilution) SEP = 466 mSec (from above) x HR (91/min) P1-P2 = 44 mm Hg (from above) C = 1 (this example is a semilunar valve) Valve Area = Flow 120.3 ml/sec = = 0.4094 cm2 (severe) C x 44.3 P1-P2 1 x 44.3 44 mm Hg where Flow = Cardiac output(ml/min) 5100ml/min = .466 sec x 91/min = 120.3 ml/sec DFP or SEP Cath Lab Manual - University of Tennessee / Bowld Hospital Page 16 Hemodynamic Calculations - Gorlin formula The valve area in Mitral Stenosis is similarly calculated, although in this instance, the pressures on both sides of the stenotic valve can be simultaneously recorded using the LV pressure and the PCWP from the Swan Ganz catheter. A sample tracing is seen below: Similarly, the area obtained in this example is 5.53 cm2, which can be conceptualized as another rectangle with the base representing that heartbeat's diastolic filling period in milliseconds and the height representing the mean diastolic transvalvular pressure gradient in mm Hg. Again, the mean diastolic transvalvular pressure gradient is calculated by measuring a traced copy of the shaded area with the planimeter (5.53cm2) and dividing by the diastolic filling period measured directly off the pressure tracing in centimeters (2.7 cm). This will yield a linear dimension (2.05 cm height) which, when Mean gradi ent compared to the scale of the pressure tracing (40 mm Hg calibrated 5.5 35 s q. cm. (mm Hg ) over 10 cm total vertical span, or 4 mm Hg/vertical cm), will convert to the mean diastolic transvalvular pressure gradient in mm Hg (8.2 mm Hg in this example). Likewise, assuming a paper feed speed of 50 Diastolic fi llin g mm/sec, each horizontal centimeter represents 200 mSec, and the peri od (m Sec) diastolic filling period is 540mSec. Often, unfortunately, the patient with mitral stenosis is in atrial fibrillation; these calculations can performed and the valve area approximated by averaging the results of 10 to 15 consecutive cardiac cycles (a tedious process, at best). Calculate the valve area with the Gorlin formula using a. b. c. d. CO = 4.8 L/min (thermodilution) DFP = 540 mSec (from above) x HR (88/min) P1-P2 = 8.2 mm Hg (from above) C = .85 (this example is a mitral valve with an LV pressure tracing) Valve Area = Flow 101 ml/sec = = 0.9367 cm2 C x 44.3 P1-P2 .85 x 44.3 8.2 mm Hg where Flow = Cardiac output(ml/min) 4800ml/min = .540 sec x 88/min = 101 ml/sec DFP or SEP Cath Lab Manual - University of Tennessee / Bowld Hospital Page 17 Hemodynamic Calculations - Gorlin formula DATA PRESENTATION At the conclusion of every study, the data derived from the study need to be presented promptly to the referring clinicians. This is accomplished in two stages; first in the chart, with a preliminary report being written by the cath fellow or staff before the patient is returned to his room, and second, via the formal final report. Copies of a preliminary report form and a final formal report are included in Appendix B. The preliminary report MUST be on the chart immediately. The formal report is to be submitted to the staff cardiologist for approval within 24 hours. No excuse for failing to meet this responsibility will be acceptable; we are a consultative service with an absolute obligation to our colleagues and their patients. CATH CONFERENCE This is a multidisciplinary educational conference designed to provide a forum wherein the most appropriate management of selected patients can be determined. Participants in this forum include the Cardiologists (staff & fellows), Thoracic Surgeons, Pediatric Cardiologists (as the case dictates), representatives of the appropriate medical service, and any other interested party. Although this is an invasive conference, the non invasive data are presented for purposes of demonstrating the indication for procedures performed and for purposes of clinical correlation. The cath fellow's responsibilities include organizing and presenting the cases as follows: 1) Determine with the staff physicians which cases are to be presented. It is best to keep an ongoing list of appropriate cases so there is no last-minute “scramble” for cases. 2) Determine which of these cases have relevant echocardiograms and relay this information to the Echo Labs. The noninvasive fellows or staff will then prepare to present the echocardiographic data at the conference. 3) Know the patient's history and physical in detail. It is acceptable and reasonable to permit the consult team or the floor resident to present the case, but it is your responsibility to know (or arrange to have available) the pertinent and detailed cardiac H&P. 4) If available, present the CXR for each case. 5) Present the relevant EKG's for each case. 6) Have copies of relevant exercise studies ± thallium. 7) Make copies or transparencies of relevant hemodynamic data which will be presented just prior to the cath films. As you develop more expertise, you will also present the angiograms to the audience. 8) Be prepared to make recommendations based on the data available to you. 9) Assist in the communication of the recommendations of the group to the referring team. Cath Lab Manual - University of Tennessee / Bowld Hospital Page 18 APPENDIX A UT Cardiac Catheterization Laboratory PRE-CATHETERIZATION ORDERS (Circle order number and check all boxes that apply. Uncircled orders will not be transcribed.) 1 Please have consent for cardiac cath and angioplasty (if applicable) on the chart prior to transfer to cath lab. 2. Please obtain transfer authorization for cardiac catheterization BEFORE 06:00 (if the patient is from the Regional Medical Center). Do not delay transport to cath lab for authorization. 3. Laboratory studies - PLEASE HAVE RESULTS ON CHART Basmet CBC with platelet count UA PT, PTT EKG CXR other:__________________________________________________ 4. Height and weight and allergies on the front of the chart. 5. Prep and shave both groins . 6. Begin an IV of _______ to infuse at _______ cc/hr Place in the left arm with an 18 gauge angiocath if possible. 7. NPO after midnight except for medications and sips of water. The patient must receive all oral medications unless they are specifically ordered to be held. 8. Medications: ASA, 325 mg p.o. now and on call to cath lab Plavix 300 mg p. o. now and 75 mg p.o. q AM heparin: __________________________________ Insulin: ___________________________________ _________________________________________ _________________________________________ _________________________________________ 9. On call to the catheterization lab: • make certain the IV is patent, • allow the patient to void or have a bowel movement if needed. • Premedicate with: Benadryl 25 mg p.o. Valium 5 mg p.o. other:__________________________________________________ 10. Please call me for any problems with the above orders - Thank you. Also, the fellow should check and record peripheral pulses and previous cath entry sites. One should administer steroids ± antihistamines for prior long term steroid Rx or contrast allergy. Cath Lab Manual - University of Tennessee / Bowld Hospital -Appendices- a i APPENDIX A UT Cardiac Catheterization Laboratory POST-CATHETERIZATION ORDERS (Circle order number and check all boxes that apply. Uncircled orders will not be transcribed.) 1. Strict bed rest for ____ hours. Keep ____ leg straight. Restrain foot if necessary. 2. • BP and HR every 15 min. times 4, then every hour times 4, then resume precath orders for VS. • Foot pulse checks and dressing checks (hematoma, bleeding, etc.) with VS. • Document all of the above on chart. 3. Remove pressure dressing in A.M. 4. Resume pre-cath diet as tolerated 5. Encourage PO fluids as tolerated. 6. IV: Remove IV when patient tolerates oral fluids and has voided Continue IV at _____ cc/hr. 7. Resume heparin at U / hr IV nitroglycerin at µg / min Medications: Oral pain medication: Resume pre-cath medications heparin: __________________________________ Insulin: ___________________________________ _________________________________________ _________________________________________ _________________________________________ 8. Labs: PTT at ________ HR and in AM Big 7 in AM CBC with platelet count in AM other: 9. EKG now and q A.M. x 2 10. Please review "post cardiac cath leg rules" sheet with patient. 11. Please call cardiology fellow below for: SBP < _____ HR <_____ or >_____ angina nausea or vomiting cold painful pulseless leg problems with the above orders. 12. Notify cardiology fellow by beeper (see below) or call 448-4195 STAT for active bleeding, growing hematoma or severe pain at the dressing site. Cath Lab Manual - University of Tennessee / Bowld Hospital -Appendices- a ii APPENDIX A UT Cardiac Catheterization Laboratory POST PTCA/STENT ORDERS (Circle order number and check all boxes that apply. Uncircled orders will not be transcribed.) PAGE 1 0F 2 Procedure: S/P PTCA with intra-coronary STENT of _______ 1. Strict bed rest. Keep ____ leg straight. Restrain foot with Kerlex if necessary. HOB may be elevated to 30° max. 2. • Continuous cardiac monitoring. • BP and HR every 15 min. times 4, then every hour times 4, then resume precath orders for VS. • Foot pulse checks and dressing checks (hematoma, bleeding, etc.) with VS. • Document all of the above on chart. 3. Resume pre-cath diet as tolerated 4. Encourage PO fluids as tolerated. 5. Medications. Oral pain medication: NTG 1/150 s.l. q 5 min for angina x 3 doses and call physician. Soluble ASA, 325 mg po q 12 hours Plavix 75mg p. o. q AM heparin: __________________________________ Insulin: ___________________________________ _________________________________________ _________________________________________ _________________________________________ 6. IV: Pressurized saline to femoral arterial sheath NS through femoral venous sheath at _____ cc/hr.. Venous sheath may be used for meds. IV nitroglycerin at _______________ µg / min IV heparin at _______________ U / hr _________________________________________ _________________________________________ Maintain PTT between 45 - 80 using HEPARIN PROTOCOL: <35 if STAT PTT is: Heparin is to be: >80 Decreased by 200 U/hr 45-80 not changed (higher end of range preferred) 40-44 Increased by 200 U/hr 35-39 Increased by 200 U/hr, and give 1000 U IV bolus Increased by 200 U/hr, and give 2000 U IV bolus (orders continued on next page) Cath Lab Manual - University of Tennessee / Bowld Hospital -Appendices- a iii APPENDIX A UT Cardiac Catheterization Laboratory POST STENT ORDERS (Circle order number and check all boxes that apply. Uncircled orders will not be transcribed.) (orders continued) 7. EKG now and q A.M. x 2 8. Labs: PAGE 2 0F 2 troponin now and q 8 hr x 2 PTT at _____ HRS and q 6 hrs. Run STAT - use results to titrate IV heparin PT with INR q AM Basmet in AM CBC with platelet count in AM _________________________________________ _________________________________________ 9. Please call cardiology fellow by beeper (see below) for: SBP < _____ HR <_____ or >_____ angina nausea or vomiting cold painful pulseless leg PTT > 100 sec or < 35 sec on two consecutive samples problems with the above orders. 10. Notify cardiology fellow by beeper (see below) or call 448-4195 STAT for: active bleeding, growing hematoma or severe pain at the dressing site. Cath Lab Manual - University of Tennessee / Bowld Hospital -Appendices- a iv APPENDIX A UT Cardiac Catheterization Laboratory POST SHEATH REMOVAL ORDERS (Circle order number and check all boxes that apply. Uncircled orders will not be transcribed.) Sheath removed at __________HRS. 1. Strict bed rest for _______ hours. Keep ____ leg straight. Restrain hand/foot with Kerlex if necessary. 2. Please review "post cardiac cath leg rules" sheet with patient. 3. • BP and HR every 15 min. times 4, then every hour times 4, then resume precath orders for VS. • Foot (wrist for arm case) pulse checks and dressing checks (hematoma, bleeding, etc.) with VS. • Document all of the above on chart. 4. Remove pressure dressing in A.M. 5. Oral pain medication: 6. Labs: PTT at ____ HR and in AM Basmet in AM CBC platelets other: 7. For stent patients: Plavix 75mg p.o. q AM. Resume Heparin infusion one hour after sheath removal at_____U/hr. Draw STAT PTT two hours after heparin is resumed and q 6 hours thereafter. Maintain PTT between 45 - 80 using HEPARIN PROTOCOL: if STAT PTT is: Heparin is to be: >80 Decreased by 200 U/hr 45-80 not changed (higher end of range preferred) 40-44 Increased by 200 U/hr 35-39 Increased by 200 U/hr, and give 1000 U IV bolus <35 Increased by 200 U/hr, and give 2000 U IV bolus Other: ___________________________________________________ 8. Please call cardiology fellow below for: SBP < _______ HR <_______ or >_______ angina nausea or vomiting cold painful pulseless leg PTT > 100 sec or < 35 sec on two consecutive samples problems with the above orders. 9. Notify cardiology fellow by beeper (see below) or call 448-4195 STAT for: active bleeding, growing hematoma or severe pain at the dressing site. Cath Lab Manual - University of Tennessee / Bowld Hospital -Appendices- a v APPENDIX B Forms PRELIMINARY REPORT CARDIAC CATHETERIZATION LABORATORY University of Tennessee, Wm. F. Bowld Hospital Patient Name ................................................................. Date..................... MRN ......................... Clinical Diagnosis: ....................................................................................... Age ........ Sex ......... PROCEDURES: APPROACH: PRESSURES: Right Atrium R heart Ventriculogram Angiogram Aortogram Biopsy PTCA/Stent Right Left Normal Right Ventricle VENTRICULOGRAM: Brachial Femoral Other...................................... Abnormal (see values below) Pul monary Artery Normal Pul monary Wedge Cardi ac Output Left Ventricle Central Aorta Heart Rate Abnormal ................................................................... CORONARY ARTERIES: SUMMARY: COMPLICATIONS: THIS IS A PRELIMINARY REPORT. AN OFFICIAL REPORT, WHICH MAY VARY, WILL FOLLOW. .....................................................................M.D., Pager................................ Dept. of Cardiology (448-4195) Cath Lab Manual - UT Bowld Hospital -Appendices- b i APPENDIX C (sample dictations) SAMPLE DICTATIONS: Organization of the procedure report is fairly easily accomplished using the components listed below. Items in italics are most frequently modified according to the case. i introductory – “The patient was premedicated with 5 mg of Valium and transported to the catheterization laboratory. He was prepped and draped in the usual fashion" ii venous access – “After infiltration of the area with local anesthesia (2% Xylocaine), using the Seldinger technique, the R femoral vein was entered. Over a guide wire, a 7 F venous sheath was placed. iii right heart – “Through the venous sheath, a 7 F thermister tipped Swan-Ganz catheter was advanced to the level of the pulmonary artery with appropriate pressures, oxygen saturations and cardiac outputs recorded. iv arterial access – “Again using the Seldinger technique, the R femoral artery was entered and over a guide wire, a 7 F sheath was placed. v left heart – “Through the arterial sheath, a 7 F pigtail catheter was advanced to the level of the ascending aorta and appropriate pressures and oxygen saturations were recorded. The catheter was then advanced retrograde across the aortic valve without difficulty and ventricular pressures recorded. A left ventriculogram was then performed in the RAO and LAO projections using 45 cc. of Cardiografin. After the ventriculogram was completed, the left ventricular and aortic pullback pressures were recorded. vi aortogram – “Using the pigtail catheter, an aortogram was then performed in the LAO view using 60 cc. of Omnipaque. vii coronary angiography – “Over a guide wire, the pigtail catheter was exchanged for a 7 F 4 cm L Judkins coronary catheter. The left main coronary ostium was cannulated without difficulty and selective angiograms of the left coronary system were obtained in multiple projections. This catheter was similarly exchanged for a 7 F 4 cm R Judkins coronary catheter. The right coronary ostium was cannulated without difficulty and selective angiograms of the right coronary artery were obtained in multiple projections. viii biopsy – “Over a guide wire and after removal of the Swan-Ganz catheter the sheath in the femoral vein was exchanged for a 7 F 125 cm. A-1 Multipurpose catheter with a 98 cm. biopsy guiding sheath and the wire removed. Using hemodynamic and fluoroscopic guidance, the catheter and sheath were advanced antegrade across the tricuspid valve into the right ventricle and the sheath advanced over the catheter, which was then removed.. Through the guiding sheath, after verifying proper position fluoroscopically, 7 F Mansfield transvenous bioptome was used to obtain multiple biopsy specimens from the right ventricular surface of the interventricular septum. ix vascular egress and hemostasis – “The patient received 5,000 units of Heparin at the initiation of the left heart catheterization and 40 mg. of Protamine at the end of the procedure. All catheters and sheaths were removed and hemostasis achieved with manual pressure. There were good right dorsalis pedis and posterior tibial pulses palpable at the end of the procedure. x final - "The patient tolerated the procedure well and left the Catheterization Laboratory in satisfactory condition. There were no apparent complications. Cath Lab Manual - University of Tennessee / Bowld Hospital -Appendices- c i APPENDIX C (sample dictations) SAMPLE DICTATION FOR FEMORAL APPROACH - Aortic and Mitral Valve disease Procedure: Right and left heart catheterization, left ventriculography, aortography and coronary angiography. The patient was premedicated with 5 mg. of Valium and 25 mg. of Benadryl and transported to the catheterization laboratory. He was prepped and draped in the usual fashion. After infiltration of the area with local anesthesia (2% Xylocaine), using the Seldinger technique, the R femoral vein was entered. Over a guide wire, a 7 F venous sheath was placed. Through the venous sheath, a 7 F thermister tipped Swan-Ganz catheter was advanced to the level of the pulmonary artery with appropriate pressures, oxygen saturations and cardiac outputs recorded. Again using the Seldinger technique, the R femoral artery was entered and over a guide wire, a 7 F sheath was placed. Through this sheath, a 7 F A-II Multipurpose catheter was advanced to the level of the ascending aorta and appropriate pressures and oxygen saturations were recorded. The catheter was then advanced retrograde across the stenotic aortic valve and ventricular pressures recorded. Simultaneous LV and wedge pressures were then recorded. A left ventriculogram was subsequently performed in the RAO and LAO projections using 78 cc. of Omnipaque After the ventriculogram was completed, the left ventricular and aortic pullback pressures were recorded. An aortogram was then performed in the LAO view using 60 cc. of Omnipaque. Using the Multipurpose catheter, the left main coronary ostium was cannulated without difficulty and selective angiograms of the left coronary system were obtained in multiple projections. The right coronary ostium was then cannulated without difficulty and selective angiograms of the right coronary artery were obtained in multiple projections. The patient received 5,000 units of Heparin at the initiation of the left heart catheterization and 50 mg. of Protamine at the end of the procedure. All catheters and sheaths were removed and hemostasis achieved with manual pressure. There were good right dorsalis pedis and posterior tibial pulses palpable at the end of the procedure. The patient tolerated the procedure well and left the Catheterization Laboratory in satisfactory condition. ______________________ Cath Lab Manual - University of Tennessee / Bowld Hospital -Appendices- c ii APPENDIX C (sample dictations) SAMPLE DICTATION FOR SONES APPROACH Procedure: L&R heart cath, LV gram, aortogram The patient was premedicated with 5 mg. of Valium and 25 mg. of Benadryl and transported to the catheterization laboratory. His right arm was prepped and draped in the usual fashion. After infiltration of right antecubital region with local anesthesia (2% Xylocaine), the right median antecubital vein and brachial artery were isolated. A thermister tipped Swan-Ganz catheter was introduced through the vein and was advanced to the level of the pulmonary artery with appropriate pressures, oxygen saturations and cardiac outputs recorded. A #7 Sones catheter was then introduced through an arteriotomy in the brachial artery and advanced to the aortic root. Appropriate pressures were recorded after which this catheter was advanced retrograde across the aortic valve into the left ventricular cavity without difficulty. Appropriate pressures were recorded. The left ventricular angiogram was then performed in the RAO projection using 45 cc. of Omnipaque After the ventriculogram was completed, the left ventricular and aortic pullback pressures were recorded. Next an aortic root angiogram was performed in the left anterior oblique projection injecting 50 cc. of dye at 30 ml. per second. Using the Sones catheter, the left main coronary ostium was cannulated without difficulty and selective angiograms of the left coronary system were obtained in multiple projections. The right coronary ostium was then cannulated without difficulty and selective angiograms of the right coronary artery were obtained in multiple projections. Next, withdrawal pressures were obtained from the right side of the heart, the Swan-Ganz catheter was removed and the vein repaired. The Sones catheter was removed and the brachial artery repaired with a single inverted locking suture using OOOO Tevdek. There was a good left radial pulse palpable after repair of the artery. The overlying skin was then sutured with interrupted silk sutures. The patient received 6000 units of Heparin via the brachial artery at the initiation of left heart catheterization. The patient tolerated the procedure well and left the Catheterization Laboratory in satisfactory condition. There were no apparent complications ______________________ SAMPLE DICTATION FOR ENDOMYOCARDIAL BIOPSY (this procedure rarely requires premedication) Procedure: Endomyocardial biopsy Mr. Green was brought to the catheterization laboratory, prepped and draped in the usual fashion. Under local anesthesia, using the Seldinger technique the R femoral vein was cannulated. Over a guide wire, a 7F 125 cm. A 1 Multipurpose catheter with a 98 cm. long venous sheath was advanced to the level of the right atrium and the guide wire removed. Under hemodynamic and fluoroscopic guidance, the catheter was advanced antegrade across the tricuspid valve and the sheath advanced over the catheter, which was then removed. After checking sheath placement, a 7F Mansfield transvenous bioptome was used to obtain multiple biopsy specimens from the right ventricular surface of the interventricular septum. At the end of the procedure, the sheath and bioptome were removed and hemostasis achieved with manual pressure. Mr. Green tolerated the procedure well, leaving the catheterization laboratory in satisfactory condition. There were no apparent complications. Cath Lab Manual - University of Tennessee / Bowld Hospital -Appendices- c iii APPENDIX D - Bibliography Recommended Reading: William Grossman: Cardiac Catheterization and Angiography An excellent established text which focuses on the scientific basis of catheterization. Spencer B King, John S Douglas, Jr.: Coronary Arteriography and Angioplasty. New York, McGraw Hill Book Co. This book examines in depth the Judkins, Sones, and multipurpose techniques. The focus is on atherosclerosis. Carl J. Pepine: Diagnostic and Therapeutic Cardiac Catheterization. Baltimore, Williams and Wilkins, 1989 A book which will serve nicely as a primer for the new cath fellow. Sing San Yang, Lamberto G Bentivoglio, Vladir Maranão, Harry Goldberg: From Cardiac Catheterization to Hemodynamic Parameters, 3rd edition. Philadelphia, FA Davis Company,1988 According to the preface, the "main objective is …… to transform raw data into meaningful hemodynamic parameters to be fused with the clinical data in cardiovascular diagnosis". This book accomplishes that goal admirably. Herbert L. Abrams: Coronary Arteriography - A Practical Approach. Boston, Little, Brown, and Co.,1983 A worthwhile guide for the beginner. Has lots of pictures with an excellent section on coronary congenital anomalies. Selected References are attached in the next section Cath Lab Manual - University of Tennessee / Bowld Hospital -Appendices- d i