Ventricular Tachyarrhythmias An Electrophysiologic Overview
advertisement

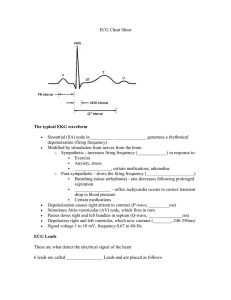
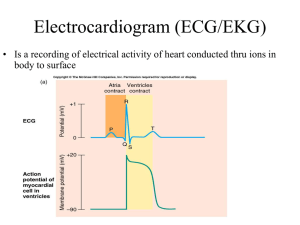
Ventricular Tachyarrhythmias An Electrophysiologic Overview Module Objectives – Ventricular Tachyarrhythmias After completion of this module, the participant should be able to: • Identify the mechanisms for ventricular tachycardias • Differentiate types of ventricular tachycardias using ECG and intracardiac electrogram recordings • Discuss treatment options for ventricular tachycardias Module Outline – Ventricular Tachyarrhythmias I. Description II. Characteristics A. Mechanisms B. Sustained vs. nonsustained C. Premature ventricular contractions Module Outline – Ventricular Tachyarrhythmias III. Classification A. Monomorphic 1. 2. Idiopathic a. Description b. ECG recognition c. Treatment – ablation Bundle branch a. Description b. ECG recognition c. Treatment –ablation Module Outline – Ventricular Tachyarrhythmias III. Classifications - continued 3. Ventricular flutter a. 4. Ventricular fibrillation a. B. ECG recognition ECG recognition Polymorphic 1. Torsades de pointes a. b. c. IV. Summary Description ECG recognition Treatment Ventricular Tachycardia (VT) • Originates in the ventricles • Can be life threatening • Most patients have significant heart disease – Coronary artery disease – A previous myocardial infarction – Cardiomyopathy Mechanisms of VT • Reentrant – Reentry circuit (fast and slow pathway) is confined to the ventricles and/or bundle branches • Automatic – Automatic focus occurs within the ventricles • Triggered activity – Early afterdepolarizations (phase 3) – Delayed afterdepolarizations (phase 4) Reentrant • Reentrant ventricular arrhythmias – Premature ventricular complexes – Idiopathic left ventricular tachycardia – Bundle branch reentry – Ventricular tachycardia and fibrillation when associated with chronic heart disease: • Previous myocardial infarction • Cardiomyopathy Automatic • Automatic ventricular arrhythmias – Premature ventricular complexes – Ischemic ventricular tachycardia – Ventricular tachycardia and fibrillation when associated with acute medical conditions: • Acute myocardial infarction or ischemia • Electrolyte and acid-base disturbances, hypoxemia • Increased sympathetic tone Automaticity Abnormal Acceleration of Phase 4 Fogoros: Electrophysiologic Testing. 3rd ed. Blackwell Scientific 1999; 16. Triggered • Triggered activity ventricular arrhythmias – – Pause-dependent triggered activity • Early afterdepolarization (phase 3) • Polymorphic ventricular tachycardia Catechol-dependent triggered activity • Late afterdepolarizations (phase 4) • Idiopathic right ventricular tachycardia Triggered Fogoros: Electrophysiologic Testing. 3rd ed. Blackwell Scientific 1999; 158. Sustained vs. Nonsustained • Sustained VT – Episodes last at least 30 seconds – Commonly seen in adults with prior: • Myocardial infarction • Chronic coronary artery disease • Dilated cardiomyopathy • Non-sustained VT – Episodes last at least 6 beats but < 30 seconds Premature Ventricular Contraction • PVC – Ectopic beat in the ventricle that can occur singly or in clusters – Caused by electrical irritability • Factors influencing electrical irritability – Ischemia – Electrolyte imbalances – Drug intoxication Classification • Ventricular Tachycardia – – Monomorphic • Idiopathic VT • Bundle branch reentry tachycardia • Ventricular flutter • Ventricular fibrillation Polymorphic • Torsades de pointes (TdP) Monomorphic VTs Monomorphic VT • Heart rate: 100 bpm or greater • Rhythm: Regular • Mechanism – Reentry – Abnormal automaticity – Triggered activity • Recognition – Broad QRS – Stable and uniform beat-to-beat appearance ECG Recognition ECG used with permission of Dr. Brian Olshansky. Intracardiac Recording of VT EGM used with permission of Texas Cardiac Arrhythmia, P.A. Idiopathic Right Ventricular Tachycardia • Right ventricular idiopathic VT – Focus originates within the right ventricular outflow tract – Ventricular function is usually normal – Usually LBBB, inferior axis • Treatment options: – Pharmacologic therapy (beta blockers, verapamil) – RF ablation ECG Recognition Kay NG. Am J Med 1996; 100: 344-356. Case History: Idiopathic VT 39 y.o. female with no prior cardiac history • First episode – 9 hours of palpitations – In ER, found to be in wide-complex tachycardia of LBBB, inferior axis, at 205 bpm – Converted with IV lidocaine; placed on tenormin • Second episode – While on tenormin, patient had onset of palpitations at airport – In ER, converted with IV lidocaine • Patient underwent EP study Case History: Idiopathic VT Case History: Idiopathic VT • At EP study, tachycardia focus was mapped and localized to right ventricular outflow tract • The focus was successfully ablated using radiofrequency energy, with no subsequent inducible or clinical VT Endocardial Activation Mapping • Using an ablation catheter, map the area around and inside of the right ventricular outflow tract • Find the electrograms that precede the onset of the QRS complex during tachycardia • This area identifies the site of earliest activation, and possibly the “site of origin” of the arrhythmia Pace Mapping • Pace mapping helps to localize the “site of origin” after endocardial mapping has been performed • If the heart is paced from this region, the resulting ECG should be identical to the ECG taken during tachycardia • Delivering RF energy to this site usually eliminates ventricular tachycardia Idiopathic VT Ablation in RVOT RAO RAO Idiopathic Left Ventricular Tachycardia • RBBB/LAFB – Involves the Purkinje network • Treatment options: – RF ablation – Pharmacologic therapy (verapamil, beta blockers) ECG Recognition ECG used with permission of Kay NG. Bundle Branch Reentry • Reentry circuit is confined to the left and right bundle branches • Usually LBBB, during sinus rhythm • Presents with: – Syncope – Palpitations – Sudden cardiac death • Treatment: RF ablation of right bundle VT Due to Bundle Branch Reentry Catheter Ablation of Right Bundle Branch V1 I II RA Current Voltage Courtesy of Dr. Warren Jackman Ventricular Flutter • Heart rate: 300 bpm • Rhythm: Regular and uniform • Mechanism: Reentry • Recognition: – No isoelectric interval – No visible T wave – Degenerates to ventricular fibrillation • Treatment: Cardioversion Ventricular Fibrillation • Heart rate: Chaotic, random and asynchronous • Rhythm: Irregular • Mechanism: Multiple wavelets of reentry • Recognition: – No discrete QRS complexes • Treatment: – Defibrillation ECG Recognition • P waves and QRS complexes not present • Heart rhythm highly irregular • Heart rate not defined Polymorphic VT Polymorphic VT • Heart rate: Variable • Rhythm: Irregular • Mechanism: – Reentry – Triggered activity • Recognition: – Wide QRS with phasic variation – Torsades de pointes ECG Recognition EGM used with permission of Texas Cardiac Arrhythmia, P.A. Torsades de Pointes (TdP) • Heart rate: 200 - 250 bpm • Rhythm: Irregular • Recognition: – Long QT interval – Wide QRS – Continuously changing QRS morphology Mechanism • Events leading to TdP are: – Hypokalemia – Prolongation of the action potential duration – Early afterdepolarizations – Critically slow conduction that contributes to reentry ECG Recognition • QRS morphology continuously changes • Complexes alternates from positive to negative Possible Causes • Drugs that lengthen the QT: – Quinidine – Procainamide – Sotalol – Ibutilide • Physical – Ischemia – Electrolyte abnormalities Treatment • Pharmacologic therapy: – Potassium – Magnesium – Isoproterenol – Possibly class Ib drugs (lidocaine) to decrease refractoriness/shorten length of action potential • Overdrive ventricular pacing • Cardioversion Summary • VT ablation is not an FDA-approved indication • RF catheter ablation can be a useful technique in patients with ventricular tachycardia • Success largely depends on the etiology of the arrhythmia • Unstable sustained VT, polymorphic VT and ventricular fibrillation are not ablatable • Improved catheters and imaging techniques may change this in the future