The Story of the Blue and the Blue
advertisement

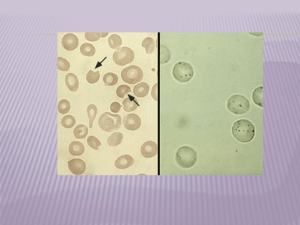
The Story of The Blue and The Blue The Story of the Blue and the Blue Morbidity and Mortality Conference Shadwan Alsafwah, MD Cardiology fellow The University of Tennessee at Memphis Case 44 Y/O M with hx of cocaine and ETOH abuse presented to the ED with few weeks history of right foot pain with foul smelling discharge, fevers at home, and feeling ill PMH: HTN IDDM with CRI and BLE neuropathy Gastric CA PUD PSH: Billirouth II surgery in 2004 Ray amputation of left 3rd toe SH: Cocaine and ETOH abuse, with recent binge smokes 2-3 cig/day since age 14 Case Meds: Was not taking any of his meds: HCTZ Felodipine Insulin Omeprazole Allergies: NKDA FH: Positive for DM and HTN ROS: Other than the R foot pain and fever, was negative Case Physical Exam: 204/106, 15, 105, 100.3, 97% on RA Head: NC, AT ENT: dry mucous membranes Neck: No JVD Chest: CTAB CVS: tachycardic, RRR, accentuated A2, no murmurs, no gallops Abdomen: midline scar, soft, NT, ND, NABS Ext: R foot: inflamed 2-5 toes, eschar on planter surface of the great toe, (+) subcutaneous gas Case Labs: WBC 35,500 Hem 9 HCT 27.3 (at baseline) Plt 573000 MCV 70 Na 118 K 4.4 CL 80 HCO3 22.7 BUN 69 Cr 4.9 (baseline 2.4) Glucose 585 Lactate 1.4 Urine: (+) ketones tox screen: (+) cocaine Right foot X-ray: (+) gas in the soft tissue of the 2nd and 3rd toes Case Admitted to SICU to Surgery Service with Medicine on consult and was started on: IVF Insulin drip Broad spectrum Abx (Pip/Tazo and Vanc) BP control (labetolol, felodipine) Had transmetatarsal amputation the same day His blood cultures grew: MRSA and Beta hemolytic Strep POD#5: started to have temp spikes U/A, CXR were negative Repeat blood cultures and urine cultures were negative (on Abx) Case 2D echo requested to R/O endocarditis, showed: Normal LVSF, EF 70% Normal chamber sizes Mild concentric LVH Possible diastolic dysfunction Mild-mod TR, mild MR, mild AI, mild PI Mild pulmonary HTN (peak systolic PAP 40 mmHg) Mild nodular thickening of the anterior tricuspid leaflet seen on the apical 4-chamber view, suspicious but not definite for vegetation TEE may be indicated if clinical suspicion is strong Case TEE was scheduled The patient was kept NPO post midnight His PE on the morning of the TEE exam: 157/91, 103, 15, Temp 100.7, Sat 97% on RA Neck: no JVD Chest: CTAB CVS: RRR, No murmurs Abdomen: soft, NT, ND, NABS Ext: S/P R TMT amp. Labs: WBC 11.300 Hemog 8.4 HCT 25.8 PLT 518 Na 133 K 3.7 CL 100 HCO3 25.7, BUN 36 Cr 2.8 Glucose 122 Coags WNL Case Prep for TEE included: Lidocaine hydrocholoride 2% viscous 20 ml x 2 Benzocaine 20% spray (Hurricaine) x2 O2 2L/min NC Conscious sedation included: Meperidine (Demerol) 25 mg IVP Midazolam (Versed) 2 mg IVP The patient experienced discomfort and nausea when the TEE probe introduction was attempted, so 2 more sprays of Benzocaine were administered The TEE probe was eventually advanced, and the study started Case After 10 minutes, the patient became cyanotic, O2 Sat by pulse oximetry dropped down to 89% O2 increased to 6L NC. However the pt became tachypnic, more cyanotic and pulse ox dropped further to 85% PE: cyanotic, tachypnic Vitals: 165/95, 25, 120s, Sat 85% on 6LNC ENT: no stridor Lungs: CTAB CVS: tachycardic, RRR Neuro: sedated/obtunded Monitor: sinus tachycardia What Happened!!! Narcotic/benzodiazepine induced respiratory depression! Brochospasm/aspiration! Esophageal rupture! Something else!!! Case The procedure was terminated Flumazenil (romazicon) 0.2 mg IVP x2 Naloxone (narcan) 1 mg IVP were given 100% NRM administered, but the patient remained cyanotic, obtunded with pulse oximetry still 85%!!! Anesthesia and respiratory care were called for emergent intubation CXR ordered stat ABGS blood drawn and sent was noted dark brown in color, so it was repeated even before waiting for the results: 7.49/31.2/363.1/25/100% Case Methemoglobinemia was suspected IV methylene blue at 1 mg/kg IVP was given in the echo lab Pt. responded well with quick reversal of his MS changes, cyanosis, and hypoxemia Was transferred to ICU for close observation Blood was sent out for Methemoglobin level which came back later: Methemoglobin level 31% (reference range: 0.4-1.5%) The patient did well overnight and the next morning repeat Methemoglobin level was 0.9% Outline Safety of TEE Historical background Physiologic background Pathophysiology Methemoglobinemia types Benzocaine formulation Risk factors Clinical presentation Diagnosis Treatment Conclusion Daniel et al. Safety of Transesophageal Echocardiography. Circulation 1991;83:817-821 Khandheria et al. Mayo Clin Proc 1994; 69:856-863 Historical Background & Incidence The first case of benzocaine induced methemoglobinemia was documented by Bernstein in 1950 Up to 1994 fewer than 100 cases has been reported in literature Between Nov 1997 through March 2002, 132 cases of benzocaine induced methemoglobinemia was reported to FDA : 107 serious (81.1%) 2 deaths (1.5%) In the pulmonary literature topical anesthetics (benzocaine and lidocaine) induced methemoglobinemia occurred in an incidence of 1/7000 bronchoscopies Physiologic Background Hemoglobin contains 4 heme groups with each containing an iron in it’s ferrous state (Fe2+) Physiologic Background It is this ferrous state (Fe 2+) that allows O2 to be transported and delivered to the tissues. With 4 heme groups having an iron in the ferrous state, one O2 molecule may be carried on each heme. Methemoglobin is an altered state of hemoglobin in which the ferrous (Fe2+) irons of heme are oxidized to the ferric (Fe3+) state Pathophysiology The ferric hemes of methemoglobin are unable to bind and carry oxygen, resulting in functional anemia In addition, the oxygen affinity of any accompanying ferrous hemes in the hemoglobin tetramere is increased As a result, the oxygen dissociation curve is left shifted, and oxygen delivery to the tissues is impaired Methemoglobin Pathophysiology RBC are continuously subjected to oxidative stressors that result in the formation of methemoglobin spontaneously in normal individuals at a rate of 0.5-3% of the available hemoglobin per day Reduction of methemoglobin maintains a steady state level of methemoglobin of about 1% of total hemoglobin Pathophysiology The most physiologically important pathway for reducing methemoglobin back to hemoglobin is the NADH-dependent reaction catalyzed by methemoglobin reductase enzyme [cytochrome b5 reductase (b5R)], this accounts for 95% of the reducing activity Less important alternative pathway in Methemoglobin reduction is by an enzyme utilizing NADPH pathway Glutathione and ascorbic acid are slow-acting pathways that play minor roles in the direct reduction of methemoglobin Methemoglobinemia Types Methemoglobinemia occurs when an imbalance due to either increased methemoglobin production or decreased methemoglobin reduction is present Inherited: 1. Cytochrome b5 reductase deficiency: type I: limited to RBC type II: All cells (most die in infancy) 2. Hemoglobin M disease: mutation in either alpha or beta globin molecule Acquired: More common, result from increased methemoglobin formation by various exogenous (most of the time pharmacologic) agents more than the rate of its reduction. The Fugate Family “The Blue People of Troublesome Creek” Agents implicated in Acquired Methemoglobinemia Agents implicated in Acquired Methemoblobinemia Amyl nitrite Aniline derivatives Butyl nitrite Bismuth subnitrite Dapsone Lidocaine Benzocaine Menthol Naphthalene Phenytoin NTG Nitrophenol Nipride Nitrites Nitrates Phenacetin Phenols Pyridium Quinones Silver nitrate Sulfonamides Benzocaine Formulations Benzocaine is available in spray form, throat lozenges, and liquid and gel preparations The spray form is prepared as 14% to 20% The average expulsion rate is 200 mg/sec The average dose that can produce methemoglobinemia is>300 mg in adults The package insert: “spray for ½ second, may repeat as needed” Risk Factors Excessive dose Concurrent use of multiple oxidizing agents Mucosal damage or inflammation are contributing factors Absorption is particularly rapid from the tracheobronchial tree, as it is technically equivalent to IV administration Differences in the metabolism of benzocaine may explain the variability of benzocaine-induced methemoglobinemia High Risk Populations Patients with methemoglobin reductase deficiency or G6PD deficiency Pediatric population and especially neonates: due to low levels of functional NADP methemoglobin reductase Elderly: NADP becomes less efficient Impaired hepatic or renal function Low Oxygen transport states: anemia, acidosis, low cardiac output state, pulmonary disease Clinical Presentation Onset of symptom is usually within 20 to 60 minutes of drug administration The symptoms and signs of methemoglobinemia correlate to the amount of abnormal hemoglobin present Usually, 5 g/dL (>30% of total hemoglobin) of reduced hemoglobin (deoxyhemoglobin) produces clinical cyanosis; but only 1.5 g/dL (>10%) of methemoglobin produces noticeable cyanosis due to the combined: 1. Decrease in O2 carrying capacity 2. shift in oxyhemoglobin dissociation curve to the left Methemoglobin Symptoms and Signs 15-20% Asymptomatic cyanosis 20-45% Headache, dyspnea, weakness, dizziness, lethargy, syncope 45-60% 60-70% >70% Decrease level of consciousness, metabolic acidosis, tachypnea Seizures, cardiac arrhythmias, homodynamic instability and shock Fatal Diagnosis Diagnostic suspicion of methemoglobinemia is based on clinical findings: generalized cyanosis out of proportion to respiratory status and normal PaO2, and doesn’t improve with administration of O2 Arterial blood drawn for blood sampling is chocolate brown, blue, or black and fail to change color when exposed to air (unlike deoxyhemoglobin) or when a drop is dried on filter paper The “oxygen saturation gap” Cooximetry is the diagnostic test of choice The cyanosis is generalized, and doesn’t improve with 100% oxygen The cyanosis has been referred to as “chocolate cyanosis” The Oxygen Saturation Gap Refers to the difference between the high O2 sat calculated from routine ABG analysis and the low O2 sat measured by pulse oximetry Methemoglobinemia should be suspected when O2 Sat (ABG) >O2 Sat (pulse OX) The Routine ABG in Methemoglobinemia The PaO2 usually is normal or inappropriately high In routine ABG analysis O2 saturation is calculated from PaO2 and pH, this leads to falsely “normal” calculated O2 sat on the ABG analysis Hence, the routine ABG by itself has no role in the diagnosis of methemoglobinemia Pulse Oximetry It usually yields information based on the ratio of light absorbance of oxyhemoglobin (940 nm) and reduced hemoglobin (660 nm) Methemoglobin absorbs light equally at both wavelengths (940 and 660), with pulse oximetry displaying a O2 Sat of 85% Hence; the higher the methemoglobin concentration, the closer the O2 Sat to 85%, regardless of patient status Multiple Wavelength Spectrophotometry (Cooximetry) Is the diagnostic test of choice for methemoglobinemia It is based upon analysis of methemoglobin absorption spectra which has peak absorbance at 631 nm A fresh specimen should always be obtained as the methemoglobin levels increase with storage Hyperlipidemia interfere with the light absorption and can cause falsely elevated methemoglobin Treatment Discontinue the offending agent Most of the cases resolve within 24-36 hours after the clearing of the residual Benzocaine General supportive measures (O2, close observation) are appropriate when methemoglobin level are <30% Treatment In more severe cases (methemoglobin>30%) methylene blue in the dose of 1to 2 mg/kg of 1% solution slow IV push over 5 minutes is the preferred treatment. Cyanosis resolve within 15-30 minutes Marked reduction in the methemoglobin concentration usually by 50% is seen within 30 to 60 minutes Methylene blue acts as a reducing agent via the NADPH methemoglobin reductase pathway It converts ferric iron back to ferrous state, restoring the O2 carrying capacity of hemoglobin Treatment Administration can be repeated in 1 hour if symptoms do not resolve Methylene blue by itself has oxidizing properties at higher doses, with toxic effects appearing in doses >7 mg/kg (dyspnea, chest pain, tremors, hemolysis) Hyperbaric O2 and exchange transfusion may be used in: 1. Patients with G6PD deficiency who do not respond to methylene blue 2. Severe cases (Methemoglobin level>70%) Conclusions Benzocaine-induced methemoglobinemia is a rare but potentially fatal reaction that is imminently treatable if the diagnosis is not delayed With the wide spread use of TEE, cardiologists need to be able to identify and treat this serious side effect Identifying high-risk patients, and the judicious use of topical benzocaine is crucial in prevention Conclusions The diagnosis is mainly clinical: with a chocolate-color cyanosis unresponsive to O2 therapy, with a sudden drop of pulse oximeter reading to 85% The saturation gap should alert the physician, and the diagnosis should be confirmed by cooxymetry Methylene blue should be readily available in areas where topical anesthetics are frequently used End The Story of the Blue and the Blue