Cardiac Transplantation Board Review Brian W. Zagol, M.D. Department of Cardiology
advertisement

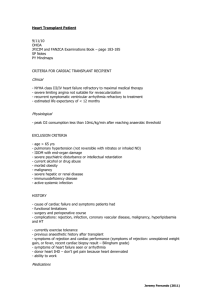
Cardiac Transplantation Board Review Brian W. Zagol, M.D. Department of Cardiology University of Tennessee Introduction • More than 4000 patients in the United States are registered with the United Organ Sharing Network (UNOS) for cardiac transplantation. • There are only about 2500 heart donors yearly. • Scarcity of donors is complicated by the use of single organs, heart injury with common braindeath injuries, difficulty with ex-vivo preservation, heart disease among donors, and the complexity of the operation. Class I Indications for Cardiac Transplantation • Cardiogenic shock requiring mechanical assistance. • Refractory heart failure with continuous inotropic infusion. • NYHA functional class 3 and 4 with a poor 12 month prognosis. • Progressive symptoms with maximal therapy. • Severe symptomatic hypertrophic or restrictive cardiomyopathy. • Medically refractory angina with unsuitable anatomy for revascularization. • Life-threatening ventricular arrhythmias despite aggressive medical and device interventions. • Cardiac tumors with low likelihood of metastasis. • Hypoplastic left heart and complex congenital heart disease. Indications of Cardiac Transplantation • Patients should receive maximal medical therapy before being considered for transplantation. They should also be considered for alternative surgical therapies including CABG, valve repair / replacement, cardiac septalplasty, etc. • VO2 has been used as a reproducible way to evaluate potential transplant candidates and their long term risk. Generally a peak VO2 >14ml/kg/min has been considered “too well” for transplant as transplantation has not been shown to improve survival over conventional medical therapy. Peak VO2 10 to 14 ml/kg/min had some survival benefit, and peak VO2 <10 had the greatest survival benefit. Contraindications to Cardiac Transplantation Evaluation of Cardiac Transplantation Recipient • Right and Left Heart Catheterization. • Cardiopulmonary testing. • Labs including BMP, CBC, LFT, UA, coags, TSH, UDS, ETOH level, HIV, Hepatitis panel, PPD, CMV IgG, RPR / VDRL, PRA (panel of reactive antibodies), ABO and Rh blood type, lipids. • CXR, PFT’s including DLCO, EKG. • Substance abuse history and evidence of abstinence for at least 6 months and enrollment in formal rehabilitation. • Mental health evaluation including substance abuse hx and social support. • Financial support. • Weight no more than 140% of ideal body weight. Status Listing • Once accepted as a transplant candidate, a patient is entered on the list and given a status based upon severity of illness. • If status changes, time accrual starts over. Status I heart recipients are given preference over status I heart / lung recipients who are given preference over status II heart recipients. • Zones are established to give local priority to recipients within 500 to 1000 mile radius centered on donor site. Status Listings • Status I. – Cardiac Assistance • • • • Total artificial heart Ventricular assist devices Intraaotic balloon pump Ventilator – Inotrope dependent for maintaining cardiac output and in hospital intensive care unit – Younger than 6 months • Status II. Patients not status I according to criteria • Status VII. Patients improved and not in immediate need of transplantation or with new complication making transplantation contraindicated. Cardiac Donor • Brain death is necessary for any cadaveric organ donation. This is defined as absent cerebral function and brainstem reflexes with apnea during hypercapnea in the absence of any central nervous system depression. • There should be no hypothermia, hypotension, metabolic abnormalities, or drug intoxication. • If brain death is uncertain, confirmation tests using EEG, cerebral flow imaging, or cerebral angiography are indicated. Cardiac Donor – Exclusion Criteria • • • • • • • • • • • Age older than 55 years. Serologic results (+) for HIV, Hepatitis B or C. Systemic Infection. Malignant tumors with metastatic potential (except primary brain tumors) Systemic comorbidity (diabetes mellitus, collagen vascular disease) Cardiac disease or trauma Coronary artery disease Allograft ischemic time estimated to be > than 4-5 hours LVH or LV dysfunction on echocardiography Death of carbon monoxide poisoning IV drug abuse. Care of Donor Before Transplantation • Contact local organ procurement organization (OPO). • Obtain patient’s height and weight. • Collect CBC, CMP, ABO / Rh testing, HIV, Hepatitis panel, and CMV Ab. • EKG. • Echocardiogram. (Fellow should be paid for this, especially if after hours) • Consider cardiac catheterization if man over 40-45 or woman over 45-50. • Insert arterial line and right heart catheter. Care of Donor Before Transplantation • Donors with beating hearts are often volume depleted because of therapy directed at reducing cerebral edema. • As soon as consent for organ transplantation is obtained (usually by OPO), normal saline should be started or sparingly blood. • A goal CVP should be 5 to 10 and PCWP of 10 to 16. • Arterial systolic BP should be maintained at least 100mmHg. If CVP and PCWP are adequate and hypotension persists dopamine and / or dobutamine should be initiated. Care of Donor Before Transplantation • Diabetes Insipidus should be suspected if urine output is >300cc/hr or if hypernatremia begins to develop. Vasopressin and hypotonic solutions can be used in this setting. • Electrolytes should be measured and corrected hourly until organ procurement. Hypertension as a result of sympathetic discharge can be managed with IV NTG. • Hyperpyrexia or hypothermia should be addressed with surveillance cultures, empiric broad-spectrum antibiotics, cooling / warming blankets. Care of Donor Before Transplantation • Metabolic acidosis from loss of adrenal and thyroid hormone secretion of brain death can depress myocardial contractility and cause vasodilatation. Acidosis should be corrected. • Ventricular dysfunction sometimes responds to levothyroxine 4 micrograms/kg/hr and methylprednisolone 100mg IV qhr and can be tried in this situation. Some recommend empiric treatment with these agents. Care of Donor Before Transplantation • Echo should be performed as soon as possible on the donor heart for assessment of LV function. If unexpected dysfunction is found in a young person, LVEDD and wall thickness should be measured. If dimensions are normal then corticosteroid and thyroid replacement should begin and any acidosis should be corrected. • Particular attention should be paid to wall motion abnormalities (especially in individuals with more advanced age), aortic stenosis, and significant mitral valve abnormalities. Care of Donor Before Transplantation • Coronary angiography should be performed on men older than 45 and women older than 50. • Precise definition of coronary anatomy is not the goal! Quick exclusion of severe lesions is! • The sheath should be sutured in place for ICU monitoring and blood sampling. Removal may also be complicated by coagulopathy. • Risk to potential donor kidneys necessitates limiting contrast exposure. Use non-ionic contrast and <25cc’s if possible. No LVgram unless absolutely necessary. Matching Donor and Recipient • Because ischemic time during cardiac transplantation is crucial, donor recipient matching is based primarily not on HLA typing but on the severity of illness, ABO blood type (match or compatible), response to PRA, donor weight to recipient ratio (must be 75% to 125%), geographic location relative to donor, and length of time at current status. • The PRA is a rapid measurement of preformed reactive anti-HLA antibodies in the transplant recipient. In general PRA < 10 to 20% then no cross-match is necessary. If PRA is > 20% then a T and B-cell crossmatch should be performed. • Patients with elevated PRA will need plasmapheresis, immunoglobulins, or immunosuppresive agents to lower PRA. Surgical Transplantation Techniques • Orthotopic implantation is the most common – it involves complete explantation of the native heart. – Biatrial anastomosis: Most common because the ischemic time is shorter. Complications include atrial dysfunction due to size mismatch of atrial remnants and arrhythmia (sinus node dysfunction, bradyarrhythmias, and AV conduction disturbances) that necessitate PPM implantation in 10-20% of patients. – Bicaval anastomosis: Decreases incidence of arrhythmias, the need for a pacemaker, and risk for mitral or tricuspid regurgitation. However narrowing of the SVC and IVC make biopsy surveillance difficult and ischemic times can be prolonged. Surgical Transplantation Techniques • Heterotopic implantation is an alternative technique in which the donor heart functions in parallel with the recipient’s heart. – It accounts of less than 0.3% of heart transplants. – This procedure can be considered if the donor heart is small enough to fit into the mediastinum without physical restriction of function. – Hypertopic transplantation is beneficial if the patient : • Has pulmonary hypertension that would exclude orthotopic transplantation. • Has heart failure that is potentially reversible (myocarditis) allowing future removal of the transplant. – The negative aspects of this approach include: • A difficult operation. • No anginal relief. • Need for anticoagulation (the native heart can cease to function and thrombose). • Contraindicated if the native heart has significant tricuspid or mitral regurgitation. Physiologic concerns of Transplant • Biatrial connection means less atrial contribution to stroke volume. • Resting heart rate is faster (95 to 110 bpm) and acceleration of heart rate is slower during exercise because of denervation. • Diurnal changes in blood pressure are abolished. • Diastolic dysfunction is very common because the myocardium is stiff from some degree of rejection and possibly from denervation. Postoperative Complications • Surgical – Aortic pseudoaneurism or rupture at cannulation site – Hemorrhagic pericardial effusion due to bleeding or coagulopathy • Medical – Severe tricuspid regurgitation – RV failure • Pulmonary artery compression • Pulmonary hypertension – LV failure • Ischemia • Operative Injury • Acute rejection Postoperative Complications • Rhythm disturbances • Asystole • Complete heart block. • Sinus node dysfunction with bradyarrhythmias (25% permanent but most resolve within 1-2 weeks). • Atrial fibrillation. • Ventricular tachycardia. • Coagulopathy induced by cardiopulmonary bypass • Respiratory failure • Cardiogenic pulmonary edema. • Noncardiogenic pulmonary edema. • Infection. • Renal or hepatic insufficiency • Drugs. • CHF. Treatment of Postoperative Complications • Treatment is directed at maintaining organ perfusion, oxygenation, acid-base balance, avoiding RV failure, and managing arrhythmias. • If needed drugs to maintain perfusion include dopamine, milrinone, NTG, Nitroprusside, isoproterenonol. • Managing RV failure is difficult. • Improve hypoxemia, acidosis, uremia, and electrolyte imbalance. • Keep transpulmonary gradient <10mmHg and PVR < 6 woods units • If vasodilators, volume reduction with diuretics and ultrafiltration, and inotropic agents fail to improve RV function, then RVAD can be considered. Treatment of Postoperative Complications • Arrhythmias – may signify acute rejection. – Bradyarrhythmias • • • • Isoproterenol 0.01 to 0.02 micrograms/kg/min. AV sequetial pacing. Most resolve in 1 to 2 weeks. AV disturbances in the early postoperative period may indicate incomplete myocardial preservation, pulmonary hypertension, acute rejection, or cardiac edema. – Tachyarrhythmias • Amiodarone, Lidocaine, B-blockers, etc. Postoperative Management • Initiation of medications, particularly immunosuppressive agents begins on the day of the operation. – Cyclosporin started IV on day of the surgery and usually continued until day 3 at which time converted to po. Usual IV dose is 0.5 mg/kg at 2 mg/min qd – Azathioprine 2 mg/kg IV qd until day 3 and then converted to po. – Solumedrol 125mg IV q8h until tolerating po and then Prednisone 0.6 mg/kg/day. – +/- Muromonab-CD3 (OKT3) started on postop day 1 at 5mg IV qd. Postoperative Management • Pneumocystis carinii prophylaxis is started within the first week after transplant. • If patient or donor is CMV positive then ganciclovir is started on postop day 2. • Endomyocardial biopsy is performed on postop day 4 and steroids can begin to be tapered if there is no rejection greater than grade 2b. • Anticoagulation is started if heterotopic transplantation has been performed. • Amylase and lipase are measured on day 3 to detect pancreatitis. • ECG’s are obtained qday. Long-term Management • Endomycardial biopsy is performed once a week for the first month and then less frequently depending on the presence or absence of rejection (usual regimen is qweek x 4 weeks, qmonth x 3 months, q3months in 1st year, q4months in 2nd year, 1 to 2 times per year subsequently). • If the donor was CMV positive a Hickman or peripherally inserted central catheter is placed for IV gangciclovir (5mg/kg IV bid x 14 days then 6mg/kg IV qd x 14 days. If the recipient was CMV negative then oral acyclovir is admisitered orally. If the recipient is CMV seropositive then the antiviral agent can be discontinued. If seroconversion occurs during treatment (and check at 1, 2, 3, and 6 month intervals), then ganciclovir is initiated for at least an additional 2 week period. Long-term Management • Cyclosporine levels are checked periodically by individual center protocols. • Echocardiography is useful periodically and as an adjunct to endomyocardial biopsy. • Cardiac catheterization is performed annually for early detection of allograft vasculopathy. • There is probably no need for routine exercise or nuclear stress testing. Immunosuppressive Agents • Azathioprine: purine analogue that works by nonspecific suppression of T and B-cell lymphocyte proliferation. • Dosage is 1 to 2 mg/kg per day. • Side effects are bone marrow suppression (dose related), increased incidence of skin cancer (use sunscreen), cutaneous fungal infections, and rarely liver toxicity and pancreatitis. • Drug interactions: allopurinol (decrease dose by 75%) and TMP/Sulfa (worsens thrombocytopenia). Immunosuppressive Agents • Cyclosporin: inhibits T-cell lymphokine production. Highly lipophilic. • Dosage is 8 to 10mg/kg/day in 2 divided doses. IV doses are 1/3 of oral doses in a continuous infusion. • Drug levels are frequently measured for dosage and toxicity, but levels are not highly predictive of actual immunosuppressive effect. Drug levels are reflected for 5 to 10 days because of a long half life. • Side effects: nephrotoxicity caused by afferent arteriolar constriction and manifested by oliguria. Loop diuretics may exacerbate this side effect. Dosage adjustments should only be made if creatinine level is >3.0mg/dL (some renal insufficiency is expected). Other side effects include hypertension, hypertrichosis, tremor, hyperkalemia, hyperlipidemia, and hyperuricemia. • Multiple drug interactions. Immunosuppressive Agents • Corticosteroids: immunosuppressives of uncertain mechanism. Used for maintenance of immunosuppression and to manage acute rejections. • High doses used initially tapered over the 1st 6 months to 5 to 15mg/d prednisone. • Side effects include mood and sleep disturbances, acne, weight gain, obesity, hypertension, osteopenia, and hyperglycemia. Immunosuppressive Agents • Mycophenolate mofetil: selectively inhibits lymphocyte proliferation. • Dosage is 2g/d po. • Side effects include GI disturbances. Does not cause significant bone marrow suppression. • FK-506 (tacrolimus): Lymphophilic macrolide that inhibits lymphokine production similar to cyclosporine. • More toxic than cyclosporine. • Side effects include nephrotoxicity and neuotoxicity. Immunosuppressive Agents • Antilymphocyte globulin: Horse polyclonal antibody designed to inhibit T cells by binding to surface antigens. • It is generally used at the time of transplantation for induction therapy or during acute rejections. • Dosage is 10 to 15 mg/kg qd through a central venous catheter. • Goal is to keep T lymphocyte count ~200cells/microL. • Side effects include fevers, chills, urticaria, serum sickness, and thrombocytopenia. Immunosuppressive Agents • Muromonab-CD3 (OKT3): a murine monoclonal antibody to the CD3 complex on the T-cell lymphocyte designed for selective T-cell depletion. • • • • Usual dose is 5mg/d IV bolus over 10 to 14 days. CD3 cells are monitored with goal <25cells/mL. Used in patients with renal insufficiency. Side effects include cytokine release syndrome (fever, chills, nausea, vomiting, mylagia, diarrhea, weakness, bronchospasm, and hypotension), pulmonary edema. • Rapamycin: Similar mechanism of action of FK-506 except that it antagonizes the proliferation of nonimmune cells such as endothelial cells, fibroblasts, and smooth muscle cells. • Not routinely used at present. • May have a roal in prevention of immunologically mediated coronary allograft vasculopathy. Basic Drug Regimen • Immunosuppressives • Antibiotic prophylaxis • PCP: TMP/Sulfa or Dapsone or Pentamidine aerosols. • CMV infection: Ganglyclovir, acyclovir. • Fungal infections: Nystatin. • Antihypertensives • Diuretics as needed • Potassium and Magnesium replacement (cyclosporin leads to wasting of thes electrolytes. • Lipid-lowering agents. (Avoid allograft vasculopathy). • Glucose lowering agents (DM and steroids) • Anticoagulation if transplant heterotopic. • Cyclosporin dose lowering meds (Diltiazem / Verapamil / Theophyilline) Complications - Rejection • Avoidance with preoperative therapy with cyclosporin, corticosteroids, and azathioprine. • If rejection is suspected then workup should include: measurement of cyclosporine level CKMB level, echocardiography for LV function, and endomyocardial biopsy. • Signs and symptoms of rejection only manifest in the late stages and usually as CHF (rarely arrhythmias). Due to close surveillance, most rejection is picked up in asymptomatic patients. Complications - Rejection • Hyperacute Rejection: Caused by preforemd antibodies against the donor in the recipient. It occurs within minutes to hours and is uniformly fatal. PRA screening is the best method in avoiding hyperacute rejection. • Acute Cellular Rejection: Most common form and occurs at least once in about 50% of cardiac transplant recipients. Half of all episodes occur within the first 2 to 3 months. It is rarely observed beyond 12 months unless immunosuppression has been decreased. Complications - Rejection • Vascular (humoral) Rejection: not well defined. – Characterized by immunoglobulin and complement in the microvasculature with little cellular infiltrate. – It is associated with positive cross match, sensitization to OKT3, female sex, and younger recipient age. – It is more difficult to treat than acute cellular rejection, is associated with hemodynamic instability, and carries a worse prognosis. Staging of Acute Rejection • If acute rejection is found, histologic review of endomyocardial biopsy is performed to determine the grade of rejection. • Grade 0 — no evidence of cellular rejection • Grade 1A — focal perivascular or interstitial infiltrate without myocyte injury. • Grade 1B — multifocal or diffuse sparse infiltrate without myocyte injury. • Grade 2 — single focus of dense infiltrate with myocyte injury. • Grade 3A — multifocal dense infiltrates with myocyte injury. • Grade 3B — diffuse, dense infiltrates with myocyte injury. • Grade 4 — diffuse and extensive polymorphous infiltrate with myocyte injury; may have hemorrhage, edema, and microvascular injury. Treatment of Acute Rejection • Grade 1A and Grade 1B: No treatment is necessary. • Grade 2: Probably no treatment is necessary. Short course of steriods (Prednisone 100mg qd x 3 days) is optional. • Grade 3A and Grade 3B: High dose corticosteroids (Solumedrol 1mg/kg IV). If no response then ATGAM (OTK3 also an option, but causes more intense cytokine reaction). • Grade 3 with hemodynamic compromise or Grade 4: High dose corticosteriods plus ATGAM or OTK3. • It is critical that an endomyocardial biopsy be performed to document reversal of rejection after treatment. Otherwise additional agents will need to be added. A biopsy is obtained 1 week after initial biopsy showed rejection and then 1 week after therapy complete. If ATGAM or OTK3 is used biopsy should be obtained at the end of a course of therapy (usually 7 to 14 days) and then again 1 week later off therapy. Complications - Rejection • Allograft vasculopathy (Chronic rejection): Transplant coronary artery disease that is the leading cause of death in patients more than 1 year after transplantation. • Likely a result of a proliferative response to immunologically mediated endothelial injury (chronic humoral rejection). • It differs from native CAD in that it is manifested by concentric stenoses, predominately subendocardial location, lack of calcification, can be rapidly progressive and lack of angina pectoris. • Risk factors include degree of histocompatibility, hypertension, hyperlipidemia, obesity, and CMV infection. Complications – Rejection Allograft Vasculopathy • Treatment is mainly prevention with statins, diltiazem, and antioxidant vitamins. Rapamycin is an agent that has shown promise in preventing this complication. • Treatment with percutaneous interventions and CABG is limited due to its diffuse nature and subendocardial locations. • Retransplantation for this disorder is an option, but retrospective analysis have shown this approach does not improve mortality as patients do significantly worse with a second transplant as compared with the first. Complications - Infection • There are two peak infection periods after transplantation: • The first 30 days postoperatively: nosocomial infections related to indwelling catheters and wound infections. • Two to six months postoperatively: opportunistic immunosuppresive-related infections. • There is considerable overlap, however as fungal infections and toxoplasmosis can be seen during the first month. • It is important to remember that immunosuppressed transplant patients can develop severe infections in unusual locations and remain afebrile. Opportunistic Infections • CMV: most common infection transmitted donor to recipient. • Manifested by fever, malaise, and anorexia. Severe infection can affect the lungs, gastrointestinal tract, and retina. • If donor is CMV positive and the recipient is CMV negative, prophylaxis with IV ganciclovir or foscarnet is given for 6 weeks and followed by longterm oral prophylaxis with acyclovir. • If the recipient is CMV positive a less potent regimen can be used. • Bone marrow toxicity related to treatment can occur and be confused with that due to azathioprine treatment. Opportunistic Infections • Toxoplasma gondii: Primary infection can be serious while reactivation is rarely a serious clinical problem. • Manifested as encephalitis, myocarditis, or pneumonitis. • Treated with pyrimethamine and sulfadiazine. • Pneumocystis carinii: Prophylactic therapy with TMP/Sulfa is highly effective in preventing progressive bilateral interstitial pneumonia caused by this protozoan. • Dapsone (Requires G6PD testing) and pentamidine aerosols (does not protect lung apices) are quite effective for those with sulfa allergies. Opportunistic Infections • Aspergillus organisms: Invasive Aspergillus infection, typically of the lung or upper respiratory tract is extremely difficult to manage. • It is fortunately rare, and usually occurs among patients who are severely immunocompromised from use of antilymphocyte antibodies. • Standard treatment is with IV Amphotericin. Complications - Malignancy • Transplant recipients have a 100-fold increase in the prevalence of malignant tumors as compared with age-matched controls. • Most common tumor is posttransplantation lymphoproliferative disorder (PTLD), a type of non-Hodgkin’s lymphoma believed to be related to EBV. • The incidence is as high as 50% in EBV-negative recipients of EBV-positive hearts. • Treatment involves reduction of immunosuppressive agents, administration of acyclovir, and chemotherapy for widespread disease. • Skin cancer is common with azathioprine use. • Any malignant tumor present before transplantation carries the risk for growth once immunosuppresion is initiated because of the negative effects on the function of T-cells. Complications - Hypertension • As many as 75% of transplant recipients treated with cyclosporine or corticosteroids evential develop hypertension. • Treatment is empiric with a diuretic added to a calcium channel blocker, B-blocker, or Ace inhibitor. • If either diltiazem or verapamil is used, the dosage of cyclosporin should be reduced. Complications - Dyslipidemia • As many as 80% of transplant recipients eventually have lipid abnormalities related to immunosuppression medications. • These dyslipidemias have been linked to accelerated allograft arteriopathy. • These disorders should be treated aggressively with statins and fibrates to hopefully alleviate transplant coronary vasculopathy. Complications – Tricuspid Regurgitation • A rare complication is tricuspid regurgitation caused by biotome-induced trauma to the valve apparatus that rarely requires valve replacement. Hospitalization of Transplanted Patients • If nausea and vomiting prevent administration of oral medications, the regimen should be changed to an IV one i.e. transplant patients should not be without immunosuppressives for even a short period of time!!! • Cyclosporin IV dose is 1/3 of oral dose. • If fever develops then the following should be performed: • Blood, urine and sputum cultures, BMP, CBC • CXR, Echocardiography (for LV function and effusion). • Consider endomyocardial biopsy for rejection. Outcomes • The survival rate according to the United States Scientific Registry for Organ Transplantation reports the 1-year survival rate to be 82% and 3 year survival rate to be 74%. • The most common cause of mortality was cardiac allograft vasculopathy. • The UNOS data suggested some group differences with 3-year survival rate for white persons 75%, Hispanics 71%, and African Americans 68% • Similar survival rates between men and women. • Lowest survival in patients < age 1 and approaching age 65. Outcomes • The typical causes of death in the first year are due to acute rejection and infection. • After the 1st year the primary cause of death is vasculopathy. • In the later stages (after the perioperative period) arrhythmia may be signs of acute rejection or of an allograft vasculopathy. Outcomes • Poor outcomes are associated with the following risk factors: • • • • • • • • • • Age less than 1 year or approaching age 65. Ventilator use at time of transplant. Elevated pulmonary vascular resistance. Underlying pulmonary disease. Diffuse atherosclerotic vascular disease. Small body surface area. The need for inotropic support pre-transplant. Diabetes mellitus. Ischemic time longer than 4 hours of transplanted heart. Sarcoidosis or amyloidosis as reason for transplant (as they may occur in the transplanted heart). Question 1 1. A 38 y/o woman is seen for a second opinion regarding the management of her chronic left ventricular dysfunction and symptomatic heart failure. She first developed symptoms 7 years with DOE. A CXR revealed cardiomegally and a subsequent echo revealed 4 chamber enlargement EF 25% without significant valvular abnormalities. Coronary angiography and endomyocardial biopsy were unrevealing and dx of idiopathic dilated cardiomyopathy was made. On good medical regimen including Digoxin, Lasix, AceI, Coreg, KCl, and metolazone prn. Continues to have class 2 to 3 symptoms and has been hospitalized 3 times in the last year. The patient has been advised by her internist that she should be listed immediately for cardiac transplantation and has been referred to you. She has learned to live with her physical limitation, but wishes to know more about her prognosis with medical therapy. Which diagnostic test is most useful in predicting her likelihood for survival over the next year? A. Cardiac Index by right heart catheterization. B. Left ventricular ejection fraction by radioventriculography. C. Plasma norepinephrine concentration. D. Peak oxygen uptake by cardiopulmonary exercise testing. E. Left ventricular dimension by echocardiography. Answer 1 1. D: Multiple studies have shown that peak O2 uptake determined by maximal CPX testing accurately predicts short-term (<18 month) prognosis in patients with moderate to severe CHF. A peak VO2 < 10 to 12 ml/kg/min is associated with a 1 year survival of only 60% and is a powerful indicator of the need for transplant listing in suitable candidates. Its predictive value is only valid when patient reaches his anaerobic threshold ie cardiac limit. Conversely patients whose VO2 exceeds 15 ml/kg/min are likely to experience one year survival rates similar or better than after cardiac transplantation. LVEF loses its independent predictive value when below 25% and in patients with advanced symptomatic CHF. Cardiac index <2.2 l/min/m2 is associated with a poor outcome, but is highly variable depending on patients volume status and afterload medications. Norepinephrine levels >900 picrograms/ml are predictive of poor two year outcome, but are seldom measured outside of clinical trials. LV dilation portends a worse prognosis, but its prognosis in the setting of chronic CHF is unclear. Question 2 2. A 45 y/o male business man presents to your office with a hx of nonischemic, dilated cardiomyopathy. He was dx 5 years earlier when he presented with CHF. In the past 3 months he has become increasingly difficult to treat with 4 hospitalizations in that time period. Today he complains of fatigue and breathlessness when he walks around his house. Meds include Digoxin 0.125mg qd, Aldactone 50mg qd, lisinopril 40mg qd, Lasix 80mg bid, Metolazone 5mg qd, and Coreg 25mg bid. Recent labs include Na 129, K 4.5, BUN 35, Cr 1.2, Digoxin 0.6 ng/ml, and Hgb 12.0. Echo 2 months earlier unchanged from previous with EF 25%. PE is significant for P 85, BP 85/60, Pox 95% RA, JVP 10cm, laterally displaced PMI, S3, 2/6 HSM at apex, cool extremities with pitting edema to knees. CPX reveals VO2 of 12ml/min/kg with peak systolic BP during the test 115mmHg. What would be your next best treatment in this patient’s management? A. Increase Digoxin to 0.25 mg qd B. Increase Aldactone to 100mg qd C. Change patient from furosemide to torsemide D. Refer patient for cardiac transplantation E. Decrease dose of Coreg and titrate to off. Answer 2 2. D. This patient is failing on appropriate regimen for CHF. His recent VO2 max score of less than 14ml/min/kg and inability to achieve BP of 120mmHg are markers for poor prognosis. Given patient’s age and lack of comorbidities, transplantation should strongly be considered. A study from the DIG trial demonstrated an increase mortality from serum digoxin dosing above 0.5 to 0.8 ng/ml range. The potential benefits of higher Aldactone dosing have not be demonstrated. The RALES trial used as dose of 25mg qd titrated to 50mg qd. Changing to torsemide from furosemide may benefit the patient if bowel wall edema is leading to decreased absorption and thus the effectiveness of furosemide, but would not be expected to affect the patients prognosis. The use of B-blockers have been shown to improve mortality and exercise tolerance in patients with cardiomyopathy. Question 3 3. You are called to the ER to see a 30 y/o African American male patient of yours who had a heart transplant for idiopathic dilated cardiomyopathy six years previously. He has come in complaining of a 2 day history of generally feeling unwell with nausea and mild dyspnea at rest. His posttransplant course has previously been uncomplicated and he has returned to work as a computer programmer and been very compliant with medical follow up. His last surveillance heart biopsy 3 months ago showed no rejection, his immunosuppressive regimen has been stable and consists of cyclosporin and mycophenolate mofetil. His other medications include diltiazem, ASA, pravastatin, and TMP/sulfa. His last cath was 2 years ago and normal. On exam he appears apprehensive with NAD, BP 105/60, pulse 110 regular, O2 sat 99%. No signs of CHF and his cardiac exam is only significant for an S3 gallop. CXR is unremarkable. ECG reveals sinus tach with IRBBB unchanged from previous but new repolarization abnormality. A bedside echocardiogram reveals mild generalized LV hypokinesis. Screening labs, including cardiac enzymes is unremarkable. Your leading diagnostic suspicion at this point should be which of the following? A. Early / Subclinical opportunistic pulmonary infection. B. Cardiac allograft rejection. C. Myocardial ischemia. D. Anxiety. E. Recurrent cardiomyopathy. Answer Question 3 3. C. The transplanted heart remains denervated (with rare exceptions) and thus transplant patients are incapable of experiencing the subjective symptom of angina pectoris. The cardiac allograft is prone to develop a very diffuse form of coronary vasculopathy this is independent of the usual coronary risk factors, is increasingly prevalent with time after transplantation, and can be rapidly progressive. A long-term transplant recipient who is on a stable low-dose immunosuppressive regimen is unlikely to develop allograft rejection or opportunistic infection, although both are within the realm of possibility. Patient is relatively hypotensive and to write his symptoms off to anxiety or an upper respiratory infection would be a great disservice. Question 4 4. A 54 y/o male heart transplant recipient arrives for an unscheduled visit in transplant clinic following 2 weeks of progressive fatigue, anorexia, and worsening SOB. He underwent transplantation 5 years ago for lymphocytic myocarditis and had an early postoperative course complicated by 2 bouts of symptomatic CMV viremia, and 2 episodes of moderate (ISHLT grade 2 rejection at 3 months; and ISHLT grade 3A rejection at 6 months) cellular rejection. Both episodes rapidly resolved after intervenous treatment with methylprednisolone. Subsequent biopsies have been ISHLT grade 0 or 1A. Chronic maintenance therapy has consisted of cyclosporin (3mg/kg qd), azathioprine (1.5mg/kg qd), amlodipine (10mg qd), and simvastatin (20mg qd). He has been entirely well and walking about 1 hour qd until symptoms suddenly appeared. PE revealed mildly Cushingoid appearance / NAD, BP 160/95, P 115 with occasional PVC’s, temp 98.8. Skin showed several AK’s over sun-exposed skin surfaces. Lung exam showed fine crackles at b/l bases. Cardiac exam showed non-displaced PMI, S2 paradoxically split, loud S4, 2/6 HSM at LLSB. JVD 8cm; 1+ peripheral edema. CXR showed mild CMG and 2+ pulmonary vascular redistribution. ECG showed Sinus tach at 114, occasional PVC, biatrial enlargement, LBBB, diffuse repolarization abnormalities, WBC 5600, Plt 210, pO2 80, pCO2 32, pH 7.45. An echo, RHC, and endomyocardial bx is contemplated. The most likely diagnosis is: A. Chronic cellular rejection. B. Acute mitral regurgitation. C. Reactivation of cytomegalovirus pneumonitis. D. Recurrent lymphocytic myocarditis. E. Transplant coronary vasculopathy. Answer Question 4 4. E. Accelerated coronary vasculopathy is the most common cause of symptomatic LV dysfunction in heart transplant recipients who survive beyond the 1st 3 years. The patients clinical presentation is characteristic of post-transplant vasculopathy. The patient probably had a “silent” AMI approximately 2 weeks ago due to an epicardial coronary occlusion. The cardiac allograft typically remains denervated in the majority of transplant recipients so typical anginal pain is typically absent. Heart faliure and sudden cardiac death are the two most common clinical presentation. This frequent complication remains the “Achilles heel” of heart transplantation and is the major cause of mortality in long-term transplant recipients. Angiographic evidence of coronary vasculopathy is evident in at least 50% of patients at 5 years. CMV infection is a significant risk factor for this complication. HMG co-reductase inhibitors have been shown to lower the incidence of transplant vasculopathy. Cellular rejection occurs in over 70% of transplant recipients but is rarely observed beyond 12 months unless immunosuppression has been decreased. CMV can produce an interstitial pneumonitis but reactivation of disease after 7 years in the absence of enhanced immusuppression is unlikely. The lack of fever or leukopenia also argues against this diagnosis. Finally recurrent lymphocytic and giant cell myocarditis in the cardiac allograft has been described, but is exceedingly rare. Question 5 5. You are asked by the family of a 53 y/o Hispanic woman to consult and render a second opinion regarding her care. She has a 5 year hx of CHF and thorough evaluation has led to the diagnosis of idiopathic, dilated cardiomyopathy. She is otherwise in good health. She has been treated with a flexible diuretic regimen, digoxin, Ace I, aldactone, and until current admission, B Blocker. She has been hospitalized 4 times in the past 6 months with exacerbations of her heart failure despite good compliance with medical and dietary regimen. She was readmitted 3 days ago with increasing dyspnea and orthopnea. The B-blocker was stopped and she has improved on IV milrinone. On exam she is resting comfortably. She is able to converse and is oriented and wishes to go home. BP 80/60 and P 98. Mild bibasilar crackles, PMI laterally displaced, 2/6 HSM, and loud S3 gallop. Her extremities are cool and free of edema. S-G catheter reveals RA 8, PAP 40/16/25, wedge 16, CO 2.6, and CI 1.7. At this point you should suggest which of the following? A. Increase the dose of milrinone. B. Restart the B-Blocker at a lower dose. C. Change milrinone to dobutamine. D. Refer for cardiac transplantation. E. Refer for hospice care. Answer Question 5 5. D. The patient clearly fits the definition of “advanced heart failure” and is a candidate for “specialized” therapies. If she were elderly or had major comorbidities, a hospice referral would be appropriate. In this case she is an excellent candidate for cardiac transplantation. There is probably little to be gained in the long-term by minor adjustments in her medications.