1 ______________ _________________ things:
advertisement

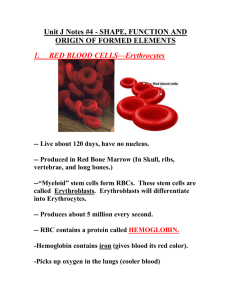
1 Chapter 17 Class Notes Spring 2011 Blood is fluid _________________________________ composed of __________________ that is a nonliving fluid __________________, and ______________ _________________ that include these 3 things: What is the Hematocrit, and what is its normal range for both males and females? Please list 6 Features of Blood (slide # 5): Describe 3 Functions of the Blood (Slides 6-8): (Slide 9) ___________ of Blood Plasma is water. Plasma Proteins are mostly produced by the ______________ and ________ of Plasma proteins are Albumin. (Slide 9) What are 3 Functions of Albumin? _____________ of Plasma Proteins are Globulins. What are 2 types of Globulins and their Function? 4% of Blood Plasma Proteins are _____________________ that forms fibrin threads in a blood clot. (Slide 11) In addition to water and plasma proteins, what are 5 more things carried by Blood Plasma? (Slide 12) Please describe 1 Feature of the three Formed Elements of Blood. Most formed elements survive in the bloodstream for ________________________, and most blood cells originate in the _____________________________ and do not ______________________. (Slide 14) Red blood cells (RBCs) are __________________ discs, ____________________, and have essentially _________ organelles. RBCs are filled with ________________________ for oxygen or ____________________ gas transport. RBCs contain the plasma membrane protein ______________ that provides flexibility for RBCs to change shape as necessary. RBCs are the major factor contributing to blood _________________________________. 2 (Slides 16-17) Please list 3 reasons why the RBC is a “superb example of complementarity of structure and function:” (Slide 18) RBCs are dedicated to __________________________________________________. (Slide 19) Hemoglobin (Hb) Structure: The protein ______________ consists of two _______ and two __________ chains, and the ______________________________ is bonded to each globin chain. An _____________ atom in the center of each heme pigment can bind to _________ oxygen gas (O2) molecule, so each Hemoglobin molecule can transport ______________ O2 molecules. Please Label the major components of Hemoglobin below (Slide 21) O2 loading of hemoglobin in the lungs produces __________________________ (ruby red). O2 unloading in the tissues produces _________________________or reduced hemoglobin (dark red) (Slide 22) CO2 loading in the tissues produces ______________________________________ (carries 20% of CO2 in the blood). Please name 3 places that Hematopoiesis occurs: (Slide 24) What are hematopoietic stem cells called? 3 (Slide 25) In RBC development, a hemocytoblast is transformed into a _________________________, and ______________________ develop into early __________________________. (Slide 26-27) What are the 3 phases that transform the early erythroblast into an erythrocyte? (Slide 29) Too few RBCs leads to tissue ________________, and too many RBCs increases blood ___________________. (Slide 31) ____________________________ hormone is the direct stimulus for erythropoiesis. It is released by the ___________________ in response to ______________ in certain kidney cells. What are 3 causes of hypoxia? (Slide 33) What are 2 effects of EPO? (Slide 33) What hormone enhances production of EPO and what is the result? Please Label the 5 steps of the Erythropoietin mechanism for regulating Erythropoiesis below: (Slide 40) An important dietary requirement for Erythropoeisis is _____________ that is stored in _______________________ (65%), and in the liver, spleen, and bone marrow. Free Iron ions (Fe 2+, Fe 3+) are toxic, so in the cell they are stored as protein-iron complexes, such as _________________ and __________________________. 4 (Slide 41) ___________________________ and _______________________ are necessary for DNA synthesis for cell division during Erythropoiesis. The life span of RBCs is _______________ days. ________________________ engulf dying red blood cells (RBCs) in the _________________. (Slide 43) During the destruction of RBCs, ______________ and globin are separated, while _____________ is salvaged and stored for reuse. Heme is degraded to the yellow pigment called _________________, the ______________ secretes Bilirubin (in bile) into the intestines. The degraded pigment leaves the body in feces as _________________. Globin is metabolized into ___________________________. (Slide 49) Please list 3 important features of Anemia: (Slide 49) Please list 4 symptoms of Anemia: (Slides 50-51) One cause of Anemia is insufficient Erythrocytes. Please name 3 types of Anemia and their Causes that are associated with this condition: (Slides 52-53) What are 2 types of Anemia and their Causes that are associated with Low Hemoglobin Content? (Slides 54-55) What are 2 inheritable types of Anemia associated with Abnormal Hemoglobin? (Slide 55) Sickle cell anemia is caused by the change in coding for a _______________ amino acid in the hemoglobin gene. What is Polycythemia and its two causes? (Slide 59) ________________________ are the only formed elements of blood that are complete cells, with nuclei and the usual organelles. They make up ________% of total blood volume and are crucial to our _____________ against disease. Leukocytes help protect the body against damage by these 5 things: Leukocytes can leave capillaries via a process called ______________________. What is the normal leukocyte response to bacterial or viral invasion called? 5 (Slide 62) What are 3 types of Granulocytes, and what are 4 of their major Features? (Slide 63) ____________________________ are the most numerous WBCs, have a __________________ nucleus, and stained cells have a ______________ color. These cells contain hydrolytic enzymes called _________________ and are very _______________________. (Slide 64) __________________________ are red-staining cells with _____________________ nucleus. These cells are modulators of the _____________________ response and digest parasitic _______________ that are too large to be phagocytized. (Slide 65) _______________________ are the rarest WBCs, that have large, purplish-black (basophilic) granules that contain __________________, which is an inflammatory chemical that acts as a vasodilator and attracts other WBCs to inflamed sites. Basophils are functionally similar to ___________ cells that release histamine to cause an inflammation response, and __________________ counter this effect. Please Label the Leukocytes Below, and Note whether the Cell is a Granulocyte or Agranulocyte: (Slide 67) Agranulocytes include ____________________ and ______________________, which ______________ visible cytoplasmic granules and have _________________ or ____________________ nuclei. (Slide 68) ______________________ have large, dark-purple, circular nuclei with a thin rim of blue cytoplasm, are mostly found in lymphoid tissue as few circulate in the __________________. These cells are crucial to _____________________. 6 (Slide 69) What are the 2 major types of Lymphocytes and what are their main function? (Slides 70-71) ___________________ are the largest Leukocytes, with abundant pale-blue cytoplasm, and dark purple-staining, U- or kidney-shaped nuclei. Monocytes ____________ the circulation, ____________ tissues, and differentiate into ____________________ which are actively _____________________ cells. Macrophages are crucial against viruses, intracellular bacterial parasites, and chronic infections, and they activate _______________ to mount an ___________________________. (Slide 73) ___________________________ is the Production of White Blood Cells that is stimulated by chemical messengers from cells of the ________________________ and mature _____________. These chemical messengers include ________________________ and _________________________________. (Slide 74) Hemocytoblasts differentiate into _____________________ and ____________________Stem Cells. Lymphoid Stem Cells are early precursors to _______________________. (Slide 75) Myeloid Stem Cells are early precursors to these 4 blood cell types: (Slide 77) Please name 2 types of serious Leukocyte Disorders and their cause: (Slide 78) Please name 2 types of Leukemia and describe which population they affect: (Slide 79) Please name 3 Features of Leukemia: (Slide 79) Please name 3 possible treatments of Leukemia: (Slides 80-81) Platelets are small cytoplasmic fragments of ______________________. Their formation is regulated by ________________________. Platelets have a blue-staining outer region and purple granules, which contain chemicals involved in ________________ such as serotonin, Ca2+, enzymes, Adenosine Di-Phosphate (ADP), and ____________________________________________ (PDGF). 7 (Slide 82) Platelets Form a temporary __________________________ that helps seal breaks in blood vessels. Circulating platelets are kept inactive and mobile by __________ and __________________ released from endothelial cells of blood vessels. Part 2, Chapter 17, The Blood (Slide 85) What is the purpose of Hemostasis and what are its 3 main Steps? (Slide 86) What is Vascular Spasm, its main Function and what are 3 triggers? (Slides 87-88) Platelet Plug Formation is a ____________________ feedback cycle. At the site of blood vessel injury, platelets stick to exposed collagen fibers with the help of _____________________________, a plasma protein. The platelets then swell, become spiked and sticky, and release these 3 chemical messengers: (Slid 88) How do these 3 messengers help perpetuate the Positive Feedback Mechanism? (Slide 90) Coagulation is a set of reactions in which blood is transformed from a liquid to a_________, and reinforces the platelet plug with _____________________. (Slide 91) Please describe the 3 Steps to Coagulation: (Slides 92-93) Please be familiar with main components of Figures on Page 9. (Slide 94) What are the 2 pathways to Prothrombin Activator? (Slides 94-95) Phase 1 (2 pathways to Prothrombin Activator) is triggered by tissue-damaging events that involves a series of _________________________or ________________________________ that are numbered from _________________________. Each pathway cascades toward activating ___________________________, which complexes with Ca2+, Platelet Factor 3 (PF3), and Factor V to form the ____________________________________. (Slide 96) The intrinsic pathway Uses Clotting Factors already present within the __________________ (intrinsic) that circulate in an _____________________ form until activated by vessel rupture and exposure of underlying tissues. 8 (Slide 97) The extrinsic pathway is triggered by exposure to ________________________________, also called Factor III, which comes from tissues ____________________________________________ ______________________________________, so it is called an “extrinsic factor” (to the blood). The Extrinsic Pathway bypasses several steps of the Intrinsic Pathway, thus it is _______________________. (Slide 98) Prothrombin Activator catalyzes the transformation of Prothrombin to the active enzyme ________________________. (Slides 99-100) Thrombin converts soluble ____________________________ into insoluble _________________________. Fibrin strands form the structural basis of a ________________, and fibrin causes plasma to become a gel-like trap for _______________________________. Thrombin (with Ca2+) activates ______________________________ which ____________________ Fibrin, and Strengthens and stabilizes the _______________. (Slide 102) In _____________________________________ actin and myosin in platelets contract within 30–60 minutes. Platelets pull on the fibrin strands, squeezing serum (plasma minus blood proteins) from the clot, and this further ______________________________ the blood ______________. (Slide 103) What 2 Growth Factors associated with the blood clot stimulate tissue repair? (Slide 104) What is Fibrinolysis? Please name 3 things that inhibit the Clotting Factors (slide # 106): What are 4 things that prevent undesirable clotting (slide # 107)? (Slide 108) Thromboembolytic disorders include __________________________________________ and ________________________________ which are abnormalities that ________________________ normal clot formation. (Slide 109) A ________________________________ is a clot that develops and persists in an unbroken blood vessel that may block circulation, leading to ________________________. An _______________________ is a Thrombus (clot) freely floating in the blood stream. _________________________________ emboli trapped in the lungs impair the ability of the body to obtain ________________________. Cerebral emboli can cause _____________________________. (Slides 110-111) What 3 things prevent thromboembolytic conditions? 9 10 (Slide 112) DIC or ____________________________________________________________________ is widespread clotting blocks intact blood vessels. Severe bleeding occurs because residual blood unable to clot, and is most common in pregnancy, septicemia, or ______________________________________________________. (Slide 113) What is thrombocytopenia, its two causes, and how is it treated? (Slide 114) Impaired liver function causes severe bleeding through an inability to ____________________________________________. Causes include _________________________________ (that is needed to synthesize 4 clotting factors), ________________________________________, or _______________________________________________. (Slide 115) What are the 3 types of hereditary Hemophilia and in what Factor is each deficient? Which type is most common? (Slide 118) Red Blood Cell membranes bear 30 types of glycoprotein ______________________ that form a unique pattern to each individual, and are perceived as foreign if transfused blood is ________________________________. Mismatching promotes _______________________________ (clumping) and destruction of RBCs . The antigens are called____________________________________________. (Slide 119) Humans have _______________ varieties of naturally occurring RBC antigens. Presence or absence of each antigen is used to classify blood cells into different blood _____________________. Antigens of the ____________ and ________________ blood groups cause vigorous transfusion reactions. Other blood groups (MNS, Duffy, Kell, and Lewis) are usually weak _______________________. (Slide 120) What are the 4 types of ABO Blood groups? Blood may contain anti-A or anti-B antibodies (agglutinins) that act against transfused RBCs with ______ ___________________ not normally present. Please label 4 blood groups in the Figure on Page 11. (Slide 123) O is the __________________________________. AB is the __________________________________________. O types react to all blood transfusions except type_____________________. AB types cannot ___________________ to anyone except an ___________________ type. 11 (Slide 124) Which Rh Factor is classified as Rh positive (+)? (Slide 125) How many transfusions can an Rh negative individual receive before Rh antibodies that cause agglutination are formed? How many transfusions are needed to cause agglutination? (Slide 126) Describe Erythroblastosis Fetalis: (Slide 127) What is the treatment for pregnant women and when is it recommended who are Rh negative and carrying Rh positive babies? (Slide #128): In a mismatched transfusion, the ____________________ cells are attacked by the ________________________________ plasma agglutinins (antibodies). 12 (Slide 129) In Blood Typing, when Serum containing anti-A or anti-B antibodies is added to the blood sample, _________________________________ will occur between the antibodies in the serum and corresponding A or B antigens in the Blood sample. Positive reactions are indicated by agglutination, or reaction by _______________________ in the Serum that is added to the Blood sample. (Slide 132) Death from _______________________________ may result from low blood volume. Volume must be replaced immediately with: (Slides 134-135) What are 7 types of blood tests?