Carbohydrate Storage and Disorders By Jennifer Turley and Joan Thompson
advertisement

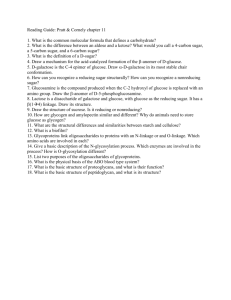
Carbohydrate Storage and Disorders By Jennifer Turley and Joan Thompson © 2016 Cengage Presentation Overview • • • • STORAGE Blood Sugar (glucose) DISORDERS Starch vs. Glycogen • Lactose Intolerance & Glycogen in detail Lactose Mal-digestion Blood sugar regulation • Hypoglycemia • Insulin & Glucagon • Diabetes What is Glucose Used for? • Immediate carbohydrate energy &/or glycogen storage (Liver & Muscle). • Brain, central nervous system (CNS), & red blood cell (RBC) function (liver glycogen). – Requires a minimum of 100-150 grams carbohydrate day (continuous). • Muscle functioning (muscle glycogen). • Fat synthesis (excess energy intake). What is Glycogen? • The storage form of glucose, “animal starch”. • Made from dietary carbohydrate sources. – All carbohydrate is converted to glucose then stored as glycogen or used immediately. Diets should be planned to meet the 45-65% of Calories AMDR & minimally the DRI for carbohydrate (130 gm/day for adults). Whole grain complex carbohydrates are best. Carbohydrate is protein sparing. Where is Glycogen Stored? • The Liver (100 grams; 400 Calories). – Is used for blood sugar (glucose) regulation. • The Muscle (1-4 grams/100 grams of muscle). – The level increases with high carbohydrate diets & exercise. – Is used for the working muscle. How Does the Body Regulate Blood Sugar? • By hormones that are produced in the pancreas. • The hormones effect the liver & muscle cells. – Insulin: decreases blood sugar levels. – Glucagon: increases blood sugar level. Blood Sugar Regulation, Part 1 Blood Sugar Regulation, Part 2 Carbohydrate Related Disorders • Lactose Intolerance & Lactose Mal-digestion • Hypoglycemia • Diabetes Lactose Intolerance, Part 1 Physiology: • Lactase deficiency (completely missing in “intolerance” while low activity/levels in “mal-digestion”) is strongly tied to evolution with several gene mutations identified. • Symptoms: Gas, bloating, cramps, diarrhea. Lactose Intolerance, Part 2 Dairy Products and Lactose Intolerance • Use a product like lactaid • Consume yogurt with live cultures • Consume aged cheese OR • Avoid dairy products Allergy vs. Intolerance • Lactose intolerance & mal-digestion are due to an inability to digest milk sugar (lactose) not an allergic reaction to milk protein (casein). • An allergy elicits an immune reaction & involves antigens & antibodies. – Antibody: Protein structures produced by immune cells that inactivate antigens (allergens). – Antigen (allergen): Foreign protein substances that elicit an immune reaction. • Allergic responses cause the formation of mucous in the respiratory tract, GI distress &/or hives. Antibody and Allergen in an Allergic Immune Response Hypoglycemia: low blood sugar • Reactive: Blood sugar levels drop after eating sugar. – Too much insulin is secreted in response to sugar consumption. Hyperinsulinemia. • Spontaneous: Liver stores of glycogen are depleted, the ability to maintain blood sugar is diminished. – Happens to everyone in between meals or when food has not been consumed. 4-6 hours during the day, 10-12 hours with sleep. • Drug Induced: Low blood sugar from a drug reaction. – Improper insulin or oral hypoglycemic drug use with diabetes. – Anti-inflammatory and thyroid medications are known to cause hypoglycemia. Diabetes : A chronic disease • Is characterized by hyperglycemia (high blood sugar). • Affects >20 million Americans, many unaware. • Increases heart disease, stroke, kidney disease, retinopathy, and neuropathy. • Decreases life expectancy. • Occurs as type 1 or type 2 diabetes. Type 1 Less common • • • • ~5% of cases Juvenile onset Is more difficult to control Insulin administration is essential in the control of blood sugar (Insulin-dependent diabetes) • Is due to a genetic and/or viral factor causing auto immunity directed against the pancreatic beta cells Physiology of Type 1 Diabetes, Part 1 Physiology of Type 1 Diabetes, Part 2 Type 2 Very common • ~95% of cases • Typically adult onset • May be controlled with lifestyle changes & oral hypoglycemic agents • Is caused by insulin resistance (decreased insulin receptor response) • Is predisposed by obesity & genetics. Physiology of Type 2 Diabetes, Part 1 Physiology of Type 2 Diabetes, Part 2 1. Oral Hypoglycemic drugs are used to make the cells respond to the insulin. 2. Blood sugar levels decline. Indications of Diabetes • Fasting glucose level ≥ 126 mg/dl. • 2 hour post prandial (fed) blood glucose level ≥ 200 mg/dl. Hyperglycemia Normal Blood Glucose is 70-99 mg/dl Pre-Diabetes is 100-125 mg/dl Glucose Tolerance Test Measures Carbohydrate Metabolism • • • • Normal diet for 3 days prior to test. Baseline fasting blood sugar level. (Levels ≥126 mg/dl indicate diabetes). Glucose load. 1 gm carbohydrate /Kg body weight or a max of 100 gm for adults. Monitor blood sugar every half hour for six hours. Overweight Contributes to Hyperglycemia type 2 diabetes Case Studies: Dick & Jane Food Composition The Glycemic Response/Index • Simple sugars & foods with a high glycemic index burn up fast & elicit an insulin response. • Complex carbohydrates sustain energy better. What is the Glycemic Response/Index? • The rise in blood sugar in response to food as compared to glucose. • Glucose is assigned 100. • The Glycemic Index of a food can be useful to anyone concerned with blood sugar control. Glycemic Response of Foods • Those with diabetes should eat foods that have a lower glycemic response or slower entrance of glucose into the blood stream. • Foods with high protein, fat, & fiber lower the glycemic response. Glycemic Index of Foods Some Summary Points, Part 1 • Glucose is required by the brain, RBCs & CNS for energy (ATP). • Carbohydrate is the preferred energy source of the body. • All carbohydrate is converted to glucose for energy. • Excess carbohydrate is stored as glycogen. (liver & muscle) • If glycogen stores are full, excess carbohydrate is stored as fat. Some Summary Points, Part 2 • Liver glycogen maintains blood sugar for brain, RBCs & CNS function. • Muscle glycogen maintains the working muscle in high intensity exercise. • The hormones insulin & glucagon regulate blood sugar levels. • Insulin decreases while glucagon increases blood sugar. Some Summary Points, Part 3 • Lactose intolerance occurs when the enzyme lactase is missing. • Milk allergy involves immunity. • Hypoglycemia is low blood sugar. Can be reactive, spontaneous, or drug induced. • Hyperglycemia is a sign of diabetes. Some Summary Points, Part 4 • Diabetes occurs as type 1 & type 2. • Unmanaged diabetes has health implications. • Individuals with diabetes should consider the glycemic response of foods for diet planning. • Selecting low glycemic index foods is useful in controlling blood sugar rises. References for this presentation are the same as those for this topic found in module 3 of the textbook