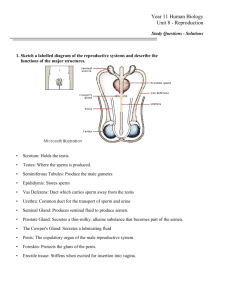
Reproductive Systems
advertisement

Reproductive Systems The reproductive system includes the following components: Gonads, or reproductive organs that produce gametes and hormones. Ducts that receive and transport the gametes. Accessory glands and organs that secrete fluids into the ducts of the reproductive system or into other excretory ducts. Perineal structures that are collectively known as the external genitalia. In both males and females, the ducts are connected to chambers and passageways that open to the exterior of the body. The structures involved constitute the reproductive tract. Penis, Penis, Penis Penis, Penis, Penis Spermatozoa are produced by the process of spermatogenesis. First, stem cells called divide by mitosis to produce two daughter cells. one of which remains at that location as a spermatogonium while the other differentiates into a primary spermatocyte. Primary spermatocytes are the cells that begin meiosis, a specialized form of cell division involved only in the production of gametes (spermatozoa in males, ova in females). Primary spermatocytes give rise to secondary spermatocytes that differentiate into spermatids—that subsequently differentiate into spermatozoa. For each primary spermatocyte that enters meiosis, 4 spermatids are produced. Meiosis produces gametes that contain half the number of chromosomes found in somatic cells. For each cell entering meiosis, the testes produce four spermatozoa, whereas the ovaries produce a single ovum. The entire process takes approximately 9 weeks. Mitochondrial activity provides the ATP required to move the tail. The tail is the only flagellum in the human body. A flagellum, a whiplike organelle, moves a cell from one place to another. The flagellum of a spermatozoon has a complex, corkscrew motion. A mature spermatozoon lacks an endoplasmic reticulum, a Golgi apparatus, and many other intracellular structures. The loss of these organelles reduces the cell’s size and mass; it is essentially a mobile carrier for the enclosed chromosomes, and extra weight would slow it down. Because the cell lacks glycogen or other energy reserves, it must absorb nutrients (primarily fructose) from the surrounding fluid. Spermatogenesis begins at puberty and continues until Vagina, vagina, vagina Vagina, vagina, vagina A woman’s reproductive system produces sex hormones and functional gametes, and it must also be able to protect and support a developing embryo and nourish a newborn infant. The principal organs of the female reproductive system are the ovaries, the uterine tubes, the uterus, the vagina, and the components of the external genitalia. The ovaries, uterine tubes, and uterus are enclosed within an extensive mesentery known as the broad ligament. The uterine tubes run along the superior border of the broad ligament and open into the pelvic cavity lateral to the ovaries. The mesovarium, supports and stabilizes the position of each ovary. The ovaries perform three main functions: (1) production of immature female gametes, or oocytes (2) secretion of female sex hormones, including estrogens and progestins (3) secretion of inhibin, involved in the feedback control of pituitary FSH production. Ovum production, or oogenesis, begins before a woman’s birth, accelerates at puberty, and ends at menopause. Between puberty and menopause, oogenesis occurs on a monthly basis as part of the ovarian cycle. Ovaries Oogenesis begins during embryonic development, and primary oocyte production is completed before birth. Each month after puberty, the ovarian cycle produces one or more secondary oocytes from the pre-existing population of primary oocytes. The number of viable and responsive primary oocytes declines markedly over time, until ovarian cycles end at age 45–55. The ovaries have roughly 2 million primordial follicles at birth, each containing a primary oocyte. By the time of puberty, the number has dropped to about 400,000. Uterus The uterus provides mechanical protection, nutritional support, and waste removal for the developing embryo (weeks 1–8) and fetus (week 9 through delivery). In addition, contractions in the muscular wall of the uterus are important in ejecting the fetus at birth. The wall has a thick, outer, muscular myometrium and a thin, inner, glandular endometrium, The uterus is a small, pear-shaped organ The uterine body is the largest portion of the uterus. The fundus is the rounded portion of the body superior to the attachment of the uterine tubes. The cervix is the inferior portion of the uterus that extends from the isthmus to the vagina. The tubular cervix projects about 1.25 cm (0.5 in.) into the vagina. Uterine Cycle We can divide the uterine cycle into three phases: (1) menses: degeneration of the endometrium, Eventually, the weakened arterial walls rupture, and blood pours into the connective tissues of the functional zone. The sloughing off of tissue is gradual, and at each site repairs begin almost at once. Nevertheless, before menses has ended, the entire functional zone has been lost. The process of endometrial sloughing, called menstruation, generally lasts from one to seven days. Over this period roughly 35 to 50 ml of blood are lost. The process can be relatively painless. The phases occur in response to hormones associated with the regulation of the ovarian cycle. Uterine Cycle (2) the proliferative phase: In the days after menses, the epithelial cells of the uterine glands multiply and spread across the endometrial surface, restoring the integrity of the uterine epithelium. Further growth and vascularization result in the complete restoration of the functional zone (3) the secretory phase: the endometrial glands enlarge, accelerating their rates of secretion, and the arteries that supply the uterine wall elongate and spiral through the tissues of the functional zone. This activity occurs under the combined stimulatory effects of progestins and estrogens. The secretory phase begins at the time of ovulation and persists as long as the corpus luteum remains intact A new cycle then begins with the onset of menses and the disintegration of the functional zone. The secretory phase generally lasts 14 days. As a result, you can identify the date of ovulation by counting backward 14 days from the first day of menses. Uterine Cycle Menopause The uterine cycle begins at puberty. The first cycle, known as menarche, typically occurs at age 11–12. The cycles continue until menopause, the termination of the uterine cycle, at age 45– 55. Regular appearance of uterine cycles is interrupted only by circumstances such as illness, stress, starvation, or pregnancy. If menarche does not appear by age 16, or if the normal uterine cycle of an adult woman becomes interrupted for six months or more, the condition of amenorrhea exists. Primary amenorrhea is the failure to initiate menses. Transient secondary amenorrhea can be caused by severe physical or emotional stresses. Chlamydia—ChlamydiaRates by Sex, United States, 1990–2010 Rate (per 100,000 population) 750 Men Women Total 625 500 375 250 125 0 1990 1992 1994 1996 1998 2000 2002 2004 2006 Year NOTE: As of January 2000, all 50 states and the District of Columbia have regulations that require the reporting of chlamydia cases. 2008 2010 Gonorrhea—Rates, United States, 1941–2010 Rate (per 100,000 population) 500 400 300 200 100 0 1941 1946 1951 1956 1961 1966 1971 1976 Year 1981 1986 1991 1996 2001 2006 Syphilis—Reported Cases by Stage of Infection, United States, 1941–2010 Cases (in thousands) 600 Primary and Secondary Early Latent Total Syphilis 500 400 300 200 100 0 1941 1946 1951 1956 1961 1966 1971 1976 Year 1981 1986 1991 1996 2001 2006 Chancroid—Reported Cases, United States, 1981–2010 Cases (in thousands) 5 4 3 2 1 0 1981 1983 1985 1987 1989 1991 1993 1995 Year 1997 1999 2001 2003 2005 2007 2009 Human Papillomavirus—Prevalence of High-risk and Low-risk Types Among Females Aged 14–59 Years, National Health and Nutrition Examination Survey, 2003–2006 Prevalence, % 60 Low-risk HPV* High-risk HPV* 50 40 30 20 10 0 14–19 20–24 25–29 30–39 40–49 Age * HPV = human papillomavirus. NOTE: Error bars indicate 95% confidence intervals. Both high-risk and low-risk HPV types were detected in some females. SOURCE: Hariri S, Unger ER, Sternberg M, Dunne EF, Swan D, Patel S, et al. Prevalence of genital HPV among females in the United States, the National Health and Nutrition Examination Survey, 2003–2006. J Infect Dis. 2011;204(4):566-73 50–59 Genital Warts—Initial Visits to Physicians’ Offices, United States, 1966–2010 Visits (in thousands) 500 400 300 200 100 0 1966 1969 1972 1975 1978 1981 1984 1987 1990 1993 1996 1999 Year NOTE: The relative standard errors for genital warts estimates of more than 100,000 range from 18% to 30%. SOURCE: IMS Health, Integrated Promotional Services™. IMS Health Report, 1966–2010. 2002 2005 2008 Genital Herpes—Initial Visits to Physicians’ Offices, United States, 1966–2010 Visits (in thousands) 400 350 300 250 200 150 100 50 0 1966 1969 1972 1975 1978 1981 1984 1987 1990 1993 1996 1999 2002 Year NOTE: The relative standard errors for genital herpes estimates of more than 100,000 range from 18% to 30%. SOURCE: IMS Health, Integrated Promotional Services™. IMS Health Report, 1966–2010. 2005 2008 AIDS More than one million people are living with HIV in the U.S. One in five living with HIV is unaware of their infection. Top ten states ranked by rate (per 100,000) of reported STD cases: United States, 2009 Rank Primary and secondary syphilis Chlamydia Gonorrhea 1 Louisiana (16.8) Mississippi (802.7) Mississippi (246.4) 2 Georgia (9.8) Alaska (752.7) Louisiana (204.0) 3 Arkansas (9.6) Louisiana (626.4) South Carolina (185.7) 4 Alabama (8.9) South Carolina (595.0) Alabama (160.8) 5 Mississippi (8.1) `Alabama (556.2) Arkansas (156.2) 6 Texas (6.8) Delaware (540.4) Illinois (154.7) 7 Tennessee (6.5) Arkansas (502.7) North Carolina (150.4) 8 North Carolina (6.3) New Mexico (478.4) Michigan (147.0) 9 New York (6.1) Tennessee (478.1) Alaska (144.3) 10 Illinois (5.8) New York (472.4) Georgia (141.3) Most activities don't spread STDs! You cannot get an STD from everyday, nonsexual activities, such as: • giving blood • sitting next to an infected person • sitting on toilet seats • sharing eating utensils• touching doorknobs • using swimming pools How can you avoid STDs (monogamy) has sex with you only If you are not in a monogamous relationship, be sure to: • Use barrier methods like latex condoms. Latex condoms are your best protection from STDs during intercourse. But remember, even condoms are not 100% effective. • Limit the number of partners you have. The more partners you have, the greater the risk of being exposed to an STD. Remember, you can't tell if someone has an STD just by looking at them. • Have regular physical exams. Ask you physician to test for STDs if you think you've been exposed. Regular tests help find STDs early, when treatment can be most effective. Don't inject drugs. Sharing needles or syringes can expose you to infected blood Waht other types of birth control help protect against STDs? Only latex condoms are considered effective protection against STDs. Birth control pills, diaphragms, sponges, and other contraceptives do not prevent STDs. A lot of men carry condoms in their wallets. Is this a good idea No. Exposure to body heat, sunlight, and extreme cold can all damage condoms and make them more likely to break. Once I've had an STD, can I get it again? Yes. Sex without a condom can result in getting an STD, no matter what STD you've already had.