Assessment and Management of Patients with Endocrine Disorders Dr Ibraheem Bashayreh 29/11/2010

1
Assessment and Management of
Patients with Endocrine Disorders
Dr Ibraheem Bashayreh
29/11/2010
2
Location of the major endocrine glands.
29/11/2010
3
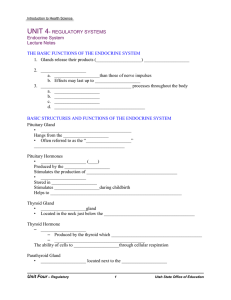
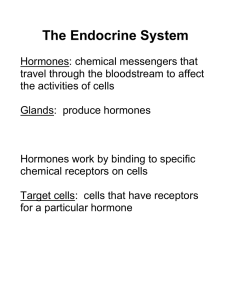
Definition of Hormones
Chemical messengers of the body
Act on specific target cells
Regulated by negative feedback
Too much hormone, then hormone release reduced
Too little hormone, then hormone release increased
29/11/2010
4
Glands of the Endocrine
System
Hypothalamus
Posterior Pituitary
Anterior Pituitary
Thyroid
Parathyroids
Adrenals
Pancreatic islets
Ovaries and testes
29/11/2010
5
Hypothalamus
Sits between the cerebrum and brainstem
Houses the pituitary gland and hypothalamus
Regulates:
Temperature
Fluid volume
Growth
Pain and pleasure response
Hunger and thirst
29/11/2010
6
Hypothalamus Hormones
Releasing and inhibiting hormones
Corticotropin-releasing hormone
Thyrotropin-releasing hormone
Growth hormone-releasing hormone
Gonadotropin-releasing hormone
Somatostatin-=-inhibits GH and TSH
29/11/2010
7
Pituitary Gland
Sits beneath the hypothalamus
Termed the “master gland”
Divided into:
Anterior Pituitary Gland
Posterior Pituitary Gland
29/11/2010
8
Anterior Pituitary Gland
Promotes growth
Stimulates the secretion of six hormones
Controls pigmentation of the skin
29/11/2010
9
Anterior Pituitary Gland
Hormones
Growth Hormone--
Adrenocorticotropic hormone
Thyroid stimulating hormone
Follicle stimulating hormone—ovary in female, sperm in males
Luteinizing hormone—corpus luteum in females, secretion of testosterone in males
Prolactin—prepares female breasts for lactation
29/11/2010
10
Actions of the major hormones of the anterior pituitary.
29/11/2010
11
Posterior Pituitary Gland
Stimulates the secretion of two hormones
Promotes water retention
29/11/2010
12
Posterior Pituitary Hormones
Antidiuretic Hormone
Oxytocin—contraction of uterus, milk ejection from breasts
29/11/2010
Adrenal Cortex
Mineralocorticoid—aldosterone. Affects sodium absorption, loss of potassium by kidney
Glucocorticoids—cortisol. Affects metabolism, regulates blood sugar levels, affects growth, antiinflammatory action, decreases effects of stress
13
Adrenal androgens—dehydroepiandrosterone and androstenedione. Converted to testosterone in the periphery.
29/11/2010
14
Adrenal Medulla
Epinephrine and norepinephrine serve as neurotransmitters for sympathetic system
29/11/2010
15
Thyroid Gland
Butterfly shaped
Sits on either side of the trachea
Has two lobes connected with an isthmus
Functions in the presence of iodine
Stimulates the secretion of three hormones
Involved with metabolic rate management and serum calcium levels
29/11/2010
16
Thyroid
Follicular cells—excretion of triiodothyronine (T3) and thyroxine (T4)—Increase BMR, increase bone and calcium turnover, increase response to catecholamines, need for fetal G&D
Thyroid C cells—calcitonin. Lowers blood calcium and phosphate levels
BMR: Basal Metabolic Rate
29/11/2010
17
Parathyroid Glands
Embedded within the posterior lobes of the thyroid gland
Secretion of one hormone
Maintenance of serum calcium levels
29/11/2010
18
Parathyroid
Parathyroid hormone—regulates serum calcium
29/11/2010
19
Pancreas
Located behind the stomach between the spleen and duodenum
Has two major functions
Digestive enzymes
Releases two hormones: insulin and glucagon
29/11/2010
20
Insulin
Pancreatic Hormones
Glucagon
—stimulates glycogenolysis and glyconeogenesis
Somatostatin
—decreases intestinal absorption of glucose
29/11/2010
21
Insulin
Produced by the Beta cells in the islets of
Langerhans
Regulates blood glucose levels
Mechanisms
Eases the active transport of glucose into muscle and fat cells
Facilitates fat formation
Inhibits the breakdown and movement of stored fat
Helps with protein synthesis
29/11/2010
22
Action of insulin and glucagon on blood glucose levels. (A) High blood glucose is lowered by insulin release.
29/11/2010
23
( continued) Action of insulin and glucagon on blood glucose levels. (B) Low blood glucose is raised by glucagon release.
29/11/2010
24
Glucagon
Produced by the alpha cells in the islets of Langerhans
Glucagon released when blood glucose falls below 70 mg/dL
29/11/2010
25
Glucagon
Prevents blood glucose from decreasing below a certain level
Functions:
Makes new glucose
Converts glycogen into glucose in the liver and muscles
Prevents excess glucose breakdown
Decreases glucose oxidation and increases blood glucose
29/11/2010
26
Kidney
1, 25 dihydroxyvitamin D—stimulates calcium absorption from the intestine
Renin—activates the RAS
Erythropoietin—Increases red blood cell production
RAS: Renin-Angiotensin System
29/11/2010
27
Adrenal Glands
Pyramid-shaped organs that sit on top of the kidneys
Each has two parts:
Outer Cortex
Inner Medulla
29/11/2010
28
Adrenal Cortex
Secretion of two hormones
Glucocorticoids: cortisol
Mineralocortocoids: aldosterone
Involved with blood glucose level, antiinflammatory response, blood volume, and electrolyte maintenance
29/11/2010
29
Adrenal Medulla
Secretion of two hormones
Epinephrine
Norepinephrine
Involved with the stress response
29/11/2010
30
Ovaries
Estrogen
Progesterone—inportant in menstrual cycle,*maintains pregnancy ,
29/11/2010
31
Testes
Androgens, testosterone—secondary sexual characteristics, sperm production
29/11/2010
32
Thymus
Releases thymosin and thymopoietin
Affects maturation of T lymphocetes
29/11/2010
33
Pineal
Melatonin
Affects sleep, fertility and aging
29/11/2010
34
Prostaglandins
Work locally
Released by plasma cells
Affect fertility, blood clotting, body temperature
29/11/2010
35
Past Medical History
Hormone replacement therapy
Surgeries, chemotherapy, radiation
Family history: diabetes mellitus, diabetes insipidus, goiter, obesity, Addison’s disease, infertility
Sexual history: changes, characteristics, menstruation, menopause
29/11/2010
36
Physical Assessment
General appearance
Vital signs, height, weight
Integumentary
Skin color, temperature, texture, moisture
Bruising, lesions, wound healing
Hair and nail texture, hair growth
29/11/2010
37
Physical Assessment
Face
Shape, symmetry
Eyes, visual acuity
Neck
29/11/2010
38
Palpating the thyroid gland from behind the client. (Source: Lester V.
Bergman/Corbis)
29/11/2010
39
Physical Assessment
Extremities
Hand and feet size
Trunk
Muscle strength, deep tendon reflexes
Sensation to hot and cold, vibration
Thorax
Lung and heart sounds
Extremity edema
29/11/2010
40
Older Adults and Endocrine
Function
Relationship unclear
Aging causes fibrosis of thyroid gland
Reduces metabolic rate
Contributes to weight gain
Cortisol level unchanged in aging
29/11/2010
41
Abnormal Findings
Ask the client:
Energy level
Fatigue
Maintenance of ADL
Sensitivity to heat or cold
Weight level
Bowel habits
Level of appetite
Urination, thirst, salt craving
29/11/2010
42
Abnormal Findings (continued)
Ask the client:
Cardiovascular status: blood pressure, heart rate, palpitations, SOB
Vision: changes, tearing, eye edema
Neurologic: numbness/tingling lips or extremities, nervousness, hand tremors, mood changes, memory changes, sleep patterns
Integumentary: hair changes, skin changes, nails, bruising, wound healing
29/11/2010
43
Most Common Endocrine
Disorders
Thyroid abnormalities
Diabetes mellitus
29/11/2010
44
Diagnostic Tests
GH: fasting, well rested, not physically stressed
Water deprivation: fasting for 12 hours, no fluids/smoking after midnight
T3/T4: no specific preparation
Serum calcium/phosphate: fasting may or may not be required
Collection that needs to be iced or refrigerated
29/11/2010
45
Diagnostic Tests
Cortisol/aldosterone level: two blood samples, client to be up for at least 2 hours before test is drawn
Urine 17-ketosteroids: 24-hour urine collection that needs to be iced or refrigerated
29/11/2010
46
Diagnostic Tests
FBS: fast before the test
HbA1c: No fasting required
2-hour OGTT: drink 75 g of glucose and do not eat anything until blood is drawn
Urine glucose/ketones: fresh urine specimen
Urine microalbumin: fresh urine specimen
29/11/2010
47
Imaging Studies
MRI: metallic implants, lie motionless during test; remove all metal objects
CT scan: assess for allergies to iodine and seafood; lie immobile during the test
Thyroid scan: allergies to iodine and seafood; hold thyroid drugs containing iodine for weeks before the study
29/11/2010
48
Imaging Studies
RAI: fast for 8 hours before; can eat 1 hour after radioiodine capsule/liquid taken; hold thyroid drugs with iodine for weeks before the study
29/11/2010
49
THYROID
DISORDERS
Dr Ibraheem Bashayreh, RN, PhD
29/11/2010
50
Thyroid Anatomy
1The gland as seen from the front is more nearly the shape of a butterfly.
2composed of 2 encapsulated lobes, one on either side of the trachea, connected by a thin isthmus.
3The thyroid extending from the level of the fifth cervical vertebra down to the first thoracic. The gland varies from an H to a U shape, overlying the second to fourth tracheal rings.
4The pyramidal lobe is a narrow projection of thyroid tissue extending upward from the isthmus and lying on the surface of the thyroid cartilage.
29/11/2010
Thyroid Anatomy
5The thyroid is enveloped by a thin, fibrous, nonstripping capsule that sends septa into the gland substance to produce an irregular, incomplete lobulation. No true lobulation exists.
6The weight of the thyroid of the normal nongoitrous adult is: 10-20 g depending on body size and iodine supply.
7The width and length of the isthmus average; 20 mm, and its thickness is ; 2-6 mm .
51
8The lateral lobes from superior to inferior poles usually measure 4 cm . and their thickness is 20-39 mm.
29/11/2010
52
Relations of the Lobes
1-Anterolaterally:
* The sternothyroid
* The superior belly of the omohyoid
* The sternohyoid
* The anterior border of the sternocleidomastoid
2-Medially:
* The larynx & the trachea.
* The pharynx & the oesophagus.
* Associated with these structures are the cricothyroid muscle & its nerve supply, the external laryngeal nerve.
* In the groove between the esophagus and the trachea is the recurrent laryngeal nerve.
29/11/2010
53
Relations of the Lobes
3-Posterolaterally:
The carotid sheath with: The common carotid artery, the internal jugular vein, and the vagus nerve.
Relations of the Isthmus
1-Anteriorly:
The sternothyroids
The sternohyoids
The anterior jugular veins
Fascia & skin.
2-Posteriorly:
The second, third, & fourth rings of the trachea.
29/11/2010
54
Venous Drainage
1-The superior thyroid vein: ascends along the superior thyroid artery and becomes a tributary of the internal jugular vein.
2- The middle thyroid vein: follows a direct course laterally to the internal jugular vein.
3- The inferior thyroid veins : follow different paths on each side. The right passes anterior to the innominate artery to the right brachiocephalic vein or anterior to the trachea to the left brachiocephalic vein. On the left side, drainage is to the left brachiocephalic vein.
Occasionally, both inferior veins form a common trunk called the thyroid ima vein, which empties into the left brachiocephalic vein.
29/11/2010
55
Physiology
The thyroid follicles secretes tri-iodothyronine(T3)and thyroxin(T4)synthesis involves combination of iodine with tyrosine group to form mono and di-iodotyrosine which are coupled to form T3 andT4.
The hormones are stored in follicles bound to thyrogobulin .
When hormones released in the blood they are bound to plasma proteins and small amount remain free in the plasma .
The metabolic effect of thyroid hormones are due to free (unbound)T3 and T4.
90%of secreted hormones is T4 but T3is the active hormone so, T4is converted to T3 peripherally.
29/11/2010
56
Physiological control of secretion
Synthesis and libration of T3 and T4 is controlled by thyroid stimulating hormone(TSH)secreted by anterior pituitary gland.
TSH release is in turn controlled by thyrotropin releasing hormone (TRH)from hypothalamus .
Circulating T3and T4 exert –ve feedback mechanism on hypothalamus and anterior pituitary gland .
So, in hyperthyroidism where hormone level in blood is high ,TSH production is suppressed and vice versa.
29/11/2010
57
Hormone
Thyroid Hormones
Function Stimulated by
T3/T4 h metabolic rate h protein synthesis h energy production
Most important hormone in day today regulation of metabolic rate i metabolic rate i
T3/T4 h
TSH
Calcitonin i blood calcium concentration i the reabsorption of Ca and Ph from bones to blood
Calcitonin “tones” down serum
Ca levels h blood Ca levels
29/11/2010
58
HYPOTHYRODISM
Hypothyroidism is the disease state in humans and animals caused by insufficient production of thyroid hormone by the thyroid gland .
•
•
INCEDENCE
30-60 yrs of age
Mostly women
Clinical Manifestations:
1. Goiter.
2. Fatigue.
3. Constipation.
4. Weight gain.
5. Memory and mental impairment and decreased concentration.
6. Depression.
7. Menstrual irregularities and loss of libido.
8. Coarseness or loss of hair.
9. Dry skin and cold intolerance.
29/11/2010
59
Clinical Manifestations:
10. Irregular or heavy menses.
11. Infertility.
12. Hoarseness.
13. Myalgias.
14. Hyperlipidemia.
15. Reflex delay.
16. Bradycardia, elevated diastolic BP.
17. Hypothermia.
18. Ataxia.
19. Decreased serum T4,T3 levels.
29/11/2010
60
LABORATORY ASSESSMENT
T3
T4
TSH
29/11/2010
61
TREATMENT
LIFELONG THYROID HORMONE REPLACEMENT
levothyroxine sodium (Synthroid, T4, Eltroxin)
IMPORTANT: start at low does, to avoid hypertension, heart failure and MI
Teach about S&S of hyperthyroidism with replacement therapy
29/11/2010
62
MYXEDEMA DEVELOPS
Rare serious complication of untreated hypothyroidism
Decreased metabolism causes the heart muscle to become flabby
Leads to decreased cardiac output
Leads to decreased perfusion to brain and other vital organs
Leads to tissue and organ failure
LIFE THREATENING EMERGENCY WITH HIGH
MORTALITY RATE
With low metabolism metabolites build up inside the cells which increases mucous and water leading to cellular edema
Edema changes client’s appearance
Nonpitting edema appears everywhere especially around the eyes, hands, feet, between shoulder blades
Tongue thickens, edema forms in larynx, voice husky
29/11/2010
63
PROBLEMS SEEN WITH MYXEDEMA
COMA
Coma
Respiratory failure
Hypotension
Hyponatremia
Hypothermia
hypoglycemia
29/11/2010
64
TREATMENT OF MYEXEDEMA COMA
Patent airway
Replace fluids with IV.
Give levothyroxine sodium IV
Give glucose IV
Give corticosteroids
Check temp, BP hourly
Monitor changes LOC hourly
Aspiration precautions, keep warm
29/11/2010
Hyperthyroidism
65
Hyperthyroidism is a condition caused by the effects of too much thyroid hormone on tissues of the body. Although there are several different causes of hyperthyroidism, most of the symptoms that patients experience are the same regardless of the cause.
Clinical Manifestations:
1. Heat intolerance.
2. Palpitations, elevated systolic BP.
3. Weight changes.
4. Menstrual irregularities and decreased libido.
5. Increased serum T4, T3.
6. Exophthalmos (bulging eyes)
7. Goiter.
8. Insomnia.
9. Muscle weakness.
10. Heat intolerance.
11. Diarrhea.
29/11/2010
66
Clinical presentation of specific condition
THYROIDITIS:
Thyroiditis is an inflammation (not an infection) of the thyroid gland. Several types of thyroiditis exist .
1-Hashimoto's Thyroiditis. Hashimoto's Thyroiditis (also called autoimmune or chronic
lymphocytic thyroiditis) is the most common type of thyroiditis.
Fatigue-Depression-Modest weight gain--Cold intolerance-Excessive sleepiness-Dry, coarse hair-Constipation-Dry skin-Muscle cramps-Increased cholesterol levels-Decreased concentration-Vague aches and pains-Swelling of the legs
2-De Quervain's Thyroiditis. (also called subacute or granulomatous thyroiditis). The thyroid gland generally swells rapidly and is very painful and tender.]
Patients will experience a hyperthyroid period as the cellular lining of colloid spaces fails, allowing abundant colloid into the circulation, with neck pain and fever. Patients typically then become hypothyroid as the pituitary reduces TSH production and the inappropriately released colloid is depleted before resolving to euthyroid. The symptoms are those of hyperthyroidism and hypothyroidism. In addition, patients may suffer from painful dysphagia. There are multi-nucleated giant cells on histology.Thyroid antibodies can be present in some cases.There is decreased uptake on isotope scan.
29/11/2010
67
Clinical presentation of specific condition
3-Silent Thyroiditis. Silent Thyroiditis is the third and least common type of thyroiditis ..
Silent thyroiditis features a small goiter without tenderness and, like the other types of resolving thyroiditis, tends to have a phase of hyperthyroidism followed by a phase of hypothyroidism then a return to euthyroidism. The time span of each phase is not concrete, but the hypo- phase usually lasts 2-3 months.
29/11/2010
68
Pressure effect:
Dysphagia. breathlesness & orthopnoea.
Hoarseness.
Facial congestion.
29/11/2010
69
Goitre
Enlargement of thyroid gland.
Classification:
Simple (non-toxic) goitre.
Toxic goitre.
Neoplastic goitre.
Inflammatory goitre.
29/11/2010
70
Simple (non-toxic) goitre
include: simple hyperplastic goitre (colloid goiter)
Cause: -physiological in pregnancy, puberty
-iodine definiecy.
Appearance: Large, smooth firm, non-tendern goitre
Effect: euythyroid & pressure effect.
Multinodular goitre.
Cause: presence of areas of hyperplasia & areas of hypoplasia in gland.
Appearance: Large, irregular, nodular goiter
Effect: euythyroid & pressure effect.
29/11/2010
71
Toxic goitre
Grave’s disease
Cause: Autoimmune disease characterizeby presence of antibodies stimulate TSH receptors in gland.
Appearance: Diffuce, nodular, hyperemic gland.
Effect: hyperthyroidism.
Toxic Multinodular goiter (plummer’s disease)
Cause: Toxic effect of MNG
Appearance: Large, irregular, nodular goiter.
Effect: hyperthyroidism
29/11/2010
72
Neoplastic goitre
Include :
benign : adenoma
malignant : papillary, follicular, anaplastic, medullary and lymphoma
Cause: -complication of MNG.
-radiation
Appearance: Enlarged goiter associated with lymphadenopathy
Effect: -pressure effect.
-euthyroid.
-invasive effect
29/11/2010
73
Inflammatory goitre
Rediel’s thyroditis
Cause: Fibrosis of thyroid
Appearance: Enlarged stony hard thyroid
Effect: Pressure effect
De quervain’s thyroiditis
Cause: Viral infection
Appearance: Diffuse, firm, tender swelling
Effect: Mild hyperthyroidism
Hashimoto’s thyroiditis
Cause: Autoantibody against thyroid gland.
Appearance: Diffuse, enlarged, non-tender goitre
Effect: Hypothyroidism
29/11/2010
74
Investigation :
Laboratory investigation:
-serum T3, T4.
-serum TSH.
-serum LATS: ( Long Acting Thyroid Stimulator) in grave’s disease
-thyroid antibodies: in hashimoto’s disease.
-serum cholesterol increase cholesterol level in hypothyroidism
29/11/2010
75
LABORATORY ASSESSMENT
IN HYPERTHYROIDISM:
T3
T4
TSH in Graves disease
Radioactive Thyroid Scan
Ultrasonography: used to determine goiter or nodules
EKG: note tachycardia
29/11/2010
76
Radiological Investigation:
-chest and neck x-ray:
Show descend of thyroid gland to thorax and mediastanal shifting in retrosternal goitre.
-iodine isotopes
By i.v injection of I131. Then, use gama rays to show hot and cold nodules.
-CT scan
Show thyroid size and if there is compression to trachea
29/11/2010
77
Endoscopic investigation:
-bronchoscopy: show compression and infiltration of trachea by tumer
Biopsy :
-fine needle aspiration biopsy.
-true-cut biopsy.
29/11/2010
78
DRUG THERAPY
Antithyroid drugs:
Thioamides : blocks thyroid hormone production; takes time
propylthiouracil (PTU)
methimazole (Tapazole)
carbimazole (Neo-Mercazole)
Need to control cardiac manifestations (tachycardia, palpitations, diaphoresis, anxiety) until hormone production reduced: use Beta-adrenergic blocking drugs : propranolol
(Inderal, Detensol)
29/11/2010
79
DRUG THERAPY
Iodine preparations :
Lugol’s Solution
SSKI (saturated solution of potassium iodide)
Potassium iodide tablets, solution, and syrup
ACTION:
decreases blood flow through the thyroid gland
This reduces the production and release of thyroid hormone
Takes about 2 wks for improvement
Leads to hypothyroidism
29/11/2010
80
DRUG THERAPY
Lithium Carbonate
ACTION: inhibits thyroid hormone release
NOT USED OFTEN BECAUSE OF SIDE EFFECTS: depressions, diabetes insipidus, tremors, N&V
29/11/2010
81
DRUG THERAPY
RADIOACTIVE IODINE THERAPY:
Receives RAI in form of oral iodine
Takes 6-8 Weeks for symptomatic relief
Additional drug therapy used during this type of treatment
Not used on pregnant women
29/11/2010
82
SURGICAL MANAGEMENT
Why use surgery?
Used to remove large goiter causing tracheal or esophageal compression
Used for pts who do not have good response to antithyroid drugs
TWO TYPES OF SURGERIES :
1.
2.
Total thyroidectomy (must take lifelong thyroid hormone replacement)
Subtotal thyroidectomy
29/11/2010
83
PREOPERATIVE CARE
Patient should become euthyroid before surgery to prevent thyroid crisis.
Assessmment vocal cord condition
Low weight:
Hi protein, hi CHO diet for days/weeks before surgery
29/11/2010
84
PRE-OPERATIVE CARE
1.
2.
3.
Antithyroid drugs to suppress function of the thyroid
Iodine prep (Lugols or K iodide solution) to decrease size and vascularity of gland to minimize risk of hemorrhage, reduces risk of thyroid storm during surgery
Tachycardia, BP, dysrhythmias must be controlled preop
29/11/2010
85
PREOPERATIVE TEACHING
Teach C&DB
Teach support neck when C&DB
Support neck when moving reduces strain on suture line
Expect hoarseness for few days (endotracheal tube)
C&DB: cough & deep breathing
29/11/2010
86
1.
2.
3.
4.
5.
6.
7.
8.
9.
POST-OP THYROIDECTOMY NURSING
CARE
VS, I&O, IV
Semifowlers
Support head
Avoid tension on sutures
Pain meds, analgesic lozengers
Humidified oxygen, suction
First fluids: cold/ice, tolerated best, then soft diet
Limited talking , hoarseness common
Assess for voice changes: injury to the recurrent laryngeal nerve
29/11/2010
87
POSTOP THYROIDECTOMY NURSING
CARE
CHECK FOR
HEMORRHAGE 1st 24 hrs:
Look behind neck and sides of neck
Check for c/o pressure or fullness at incision site
Check drain
REPORT TO MD
CHECK FOR
RESPIRATORY DISTRESS
Laryngeal stridor (harsh hi pitched resp sounds)
Result of edema of glottis, hematoma,or tetany
Trach set/airway/ O2, suction
CALL MD for extreme hoarseness
29/11/2010
88
Complication of operation:
Hemorrhage
Recurrent laryngeal nerve damage.
Superior laryngeal nerve damage
Hypoparathyrodism
Hypothyroidism
Septesis
Postoperative infection
Hypertrofic scaring (keloid)
29/11/2010
89
Thank You !!
29/11/2010