Evidenced-Based Care of the Child with Traumatic Head Injury
advertisement

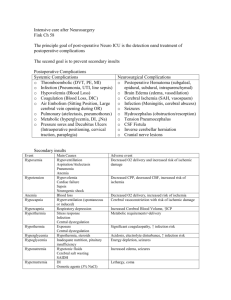
Evidenced-Based Care of the Child with Traumatic Head Injury A. Student The Children’s Hospital of Philadelphia Dr. Abdul-Monim Batiha Objectives • Describe the pathophysiology of traumatic brain injury • Discuss the scientific rationale for the therapeutic interventions used in the care of brain injured children • Provide research based recommendations for the care of children with traumatic brain injury Rhoads & Pflanzer (1996) Human Physiology p. 211 Traumatic Head Injury ALL-NET Pediatric Critical Care Textbook Source: LifeART EM Pro (1998) Lippincott Williams & Wilkins. www.med.ub.es/All-Net/english/neuropage/trauma/head-8htm Layers of the Cranial Vault Anatomy of the Brain www.neurosurgery.org/pubpgages/patres/anatofbrain.html#micro Epidural and Subdural Hematoma ALL-NET Pediatric Critical Care Textbook - Source: LifeART EM Pro (1998) Lippincott Williams & Wilkins. www.med.ub.es/All-Net/english/neuropage/trauma/head-8htm Subarachnoid Hemorrhage Rogers (1996) Textbook of Pediatric Intensive Care pp. 829 Cerebral Spinal Fluid • Produced by the choroid plexus • Average volume 90 - 150 ml – (0.35 ml / minute or 500 ml / day) • Reabsorbed through the arachnoid villi • Drainage may be blocked by inflammation of the arachnoid villi, diffuse cerebral edema, mass effect of hemorrhage or intraventricular hemorrhage Brain Cells Concussion Contusion Intracerebral hemorrhage Rhoads & Pflanzer (1996) Human Physiology p. 213 Neurons Neuroscience for Kids www.faculty.washington.edu/chudler/cells/html Diffuse Axonal Injury • Shearing injury of axons Deep cerebral cortex, thalamus, basal ganglia • Punctate hemorrhage and paranchymal edema Cerebral Blood Flow Regulation of Cerebral Vascular Resistance CBF Normal 50 - 100 ml / min MAP PaCo2 (mmHg) (mmHg) Normal 60 - 150 mmHg Normal 30 - 50 mmHg Rogers (1996) Textbook of Pediatric Intensive Care pp. 648 - 651 Cerebral Edema • Cellular response to injury – Primary injury • Secondary injury – Hypoxic-ischemic injury • Injured neurons have increased metabolic needs • Concurrent hypotension and hypoxemia • Inflammatory response Neuronal Response to Injury Primary mechanical injury & secondary hypoxic-ischemic injury Ca+ Lactate ATP Glucose Acidosis NMDA O2 - Edema Glutamate Cyclooxygenase Lipoxygenase Arachidonic Acid Leukotriene Thromboxane Prostaglandin Fluid Inflammation: Vasoreactivity Thrombosis Neutrophils Monitoring Brain Metabolism Jugular Venous Catheter Jugular Venous Oxygen Saturation (SJVO2) Arteriojugular Venous Oxygen Difference (AJVO2) Cerebral Metabolic Rate For Oxygen (CMRO2) Possible better outcome in adults Cruz (1998) Critical Care Medicine, 26(2) Brain Sensors Brain tissue pH, PaO2, PcO2, lactate Kiening (1997) Neurology Research, 19(3) Cerebral Edema after Head Trauma ALL-NET Pediatric Critical Care Textbook Source: Research by Samuel Neff MD. www.med.ub.es/All-Net/english/neuropage/trauma/head-10htm Monroe- Kellie Principle Rogers (1996) Textbook of Pediatric Intensive Care p. 646 Management of Traumatic Head Injury • Maximize oxygenation and ventilation • Support circulation / maximize cerebral perfusion pressure • Decrease intracranial pressure • Decrease cerebral metabolic rate Monitoring • Serial neurologic examinations • Circulation / Respiration • Intracranial Pressure • Radiologic Studies • Laboratory Studies Scherer & Spangenberg (1998) Critical Care Medicine, 26(1) Fibrinogen and platelets are significantly decreased in TBI patients Ong et al. (1996) Pediatric Neurosurgery, 24(6) GCS, hypoxemia and radiologic evidence of SAH, edema and DAI predict morbidity GCS alone does not predict morbidity Kokoska et al. (1998), Journal of Pediatric Surgery, 33(2) Hypotension is predictive of morbidity GCS and PTS are not predictive of outcome Respiratory Support: Maximize Oxygenation • Hypoxemia is predictive of morbidity – Ong et al. (1996) Pediatric Neurosurgery, 24(6) • Neurogenic pulmonary edema / concurrent lung injury – Positive End Expiratory Pressure • May impair cerebral venous return – Cooper et al. (1985) Journal of Neurosurgery, 63 – Feldman et al. (1997) Journal of Neurosurgical Anesthesiology, 9(2) • PEEP > 10 cm H2O increases ICP Respiratory Support: Normoventilation Hyperventilation : Historical management more harm than good? Originally adapted from Skippen et al. (1997) Critical Care Medicine, 25 ALL-NET Pediatric Critical Care Textbook www.med.ub.es/All-Net/english/neuropage/\protect/vent-5htm Evidence Supporting Normoventilation • Forbes et al. (1998) Journal of Neurosurgery, 88(3) • Marion et al. (1995) New Horizons, 3(3) • McLaughlin & Marion (1996) Journal of Neurosurgery, 85(5) • Muizelaar et al. (1991) Journal of Neurosurgery, 75(5) • Newell et al. (1996) Neurosurgery, 39(1) • Skippen et al. (1997) Critical Care Medicine, 25(8) • Yundt & Diringer (1997) Critical Care Clinics, 13(1) Use of Hyperventilation ... • Management of very acute elevation of intracranial pressure • Preemptive for activities known to increase intracranial pressure • No lower than 32-35 cmH20 --- Moderate and transient Suctioning • Hyper-oxygenation • Mild / moderate hyperventilation Brown & Peeples (1992) Heart & Lung, 21 Parsons & Shogan (1982) Heart & Lung, 13 • Intratracheal / intravenous lidocaine Donegan & Bedford (1980) Anesthesiology, 52 Wainright & Gould (1996) Intensive & Critical Care Nursing, 12 • As needed basis and individualize according to patient response 53% Percent increase in ICP with suctioning 0% Hypervent IV lido IT lido Wainright & Gould (1996) Circulatory Support: Maintain Cerebral Perfusion Pressure 6 5 Number of Hypotensive Episodes Good Moderate Severe Vegetative Dead 4 3 2 1 0 Outcome Kokoska et al. (1998), Journal of Pediatric Surgery, 33(2) Circulatory Support: Maintain Cerebral Perfusion Pressure • Adelson et al. (1997) Pediatric Neurosurgery, 26(4) – Children (particularly < 24 months old) are at increased risk of cerebral hypoperfusion after TBI – Low CBF is predictive of morbidity • Rosner et al. (1995) Journal of Neurosurgery, 83(6) – Management aimed at maintaining CPP (70 mmHg) improves outcomes CPP = MAP - ICP Lowering ICP Brain Blood CSF Mass • Evacuate hematoma Bone • Drain CSF – Intraventricular catheters use is limited by degree of edema and ventricular effacement • Craniotomy – Permanence, risk of infection, questionable benefit • Reduce edema • Promote venous return • Reduce cerebral metabolic rate • Reduce activity associated with elevated ICP Hyperosmolar Therapy: Increase Blood Osmolarity Brain cell Fluid Blood vessel Movement of fluid out of cell reduces edema Osmosis: Fluid will move from area of lower osmolarity to an area of higher osmolarity Diuretic Therapy Osmotic Diuretic • Mannitol (0.25-1 gm / kg) • Increases osmolarity • Vasoconstriction (adenosine) / less effect if autoregulation is impaired and if CPP is < 70 • Initial increase in blood volume, BP and ICP followed by decrease • Questionable mechanism of lowering ICP Loop Diuretic • Furosemide • Decreased CSF formation • Decreased systemic and cerebral blood volume (impairs sodium and water movement across blood brain barrier) • May have best affect in conjunction with mannitol • Rosner et al. (1987) Neurosurgery, 21(2) • Pollay et al. (1983) Journal of Neurosurgery, 59 ; Wilkinson (1983) Neurosurgery,12(4) Hypertonic Fluid Administration • Fisher et al. (1992) Journal of Neurosurgical Anesthesiology, 4 – Reduction in mean ICP in children 2 hours after bolus administration of 3% saline • Taylor et al. (1996) Journal of Pediatric Surgery,31(1) – ICP is lowered by resuscitation with hypertonic saline vs. lactated ringers solution in an animal model • Qureshi et al. (1998) Critical Care Medicine, 26(3) – Reduction in mean ICP within 12 hours of continuous infusion of 3% saline acetate solution – Little continued benefit after 72 hours of treatment Hyperosmolar Therapy Goal: Sodium 145-155 Sodium: square ICP: circle Qureshi et al. (1998) Critical Care Medicine, 26(3) Promote Venous Drainage Keep neck mid-line and elevate head of bed …. To what degree? Feldman et al. (1992) Journal of Neurosurgery, 76 March et al. (1990) Journal of Neuroscience Nursing, 22(6) Parsons & Wilson (1984) Nursing Research, 33(2) Dicarlo in ALL-NET Pediatric Critical Care Textbook www.med.ub.es/All-Net/english/neuropage/\protect/icp-tx-3.htm Reduction of Cerebral Metabolic Rate • Reduction in cerebral oxygen requirement – Anticonvulsants - Prevent seizure activity – Pentobarbital • Adverse effects include hypotension and bone marrow dysfunction • Used only after unsuccessful attempts to control ICP and maximize CPP with other therapies • Improved outcome not fully supported by research Traeger et al. (1983) Critical Care Medicine, 11 Ward et al. (1985) Journal of Neurosurgery, 62(3) Reduction of Cerebral Metabolic Rate: Hypothermia • Metz et al. (1996) Journal of Neurosurgery, 85(4) – 32.5 C reduced cerebral metabolic rate for oxygen (CMRO2) by 45% without change in CBF, and intracranial pressure decreased significantly (p < 0.01) • Marion et al. (1997) New England Journal of Medicine, 336(8) – At 12 months, 62% of patients (GCS of 5-7) cooled to 32-33 C have good outcomes vs. 38% of patients in control group Side-effects: Potassium flux Coagulopathy Shivering Skin Breakdown Slow re-warming Close monitoring No pediatric studies! ICP management continued... Management of Pain & Agitation • Opiods • Benzodiazepines Management of Movement • Neuromuscular blockade Difficult to assess neurologic exam Monitor for hypotension Short acting agents beneficial Do opiods increase CBF? Increased ICP with concurrent decreased MAP and CPP has been documented. Elevation in ICP is transient and there is no resulting ischemia from decreased MAP / CPP. Albanese et al. (1999) Critical Care Medicine, 27(2) Nursing Activities and ICP 20 18 16 14 ICP 12 Turning Suctioning Bathing 10 8 6 4 2 0 Before During After Rising (1993) Journal of Neuroscience Nursing, 25(5) Nursing Activities and ICP 20 18 16 14 ICP 12 10 Suctioning Turning 8 Bathing 6 4 2 0 Before During After Rising (1993) Journal of Neuroscience Nursing, 25(5) Family Contact and ICP Presence, touch and voice of family / significant others... • Does not significantly increase ICP • Has been demonstrated to decrease ICP Bruya (1981) Journal of Neuroscience Nursing, 13 Hendrickson (1987) Journal of Neuroscience Nursing, 19(1) Mitchell (1985) Nursing Administration Quarterly, 9(4) Treolar (1991) Journal of Neuroscience Nursing, 23(5) Summary of Recommended Practices • Maximize oxygenation (PEEP < 10) • Normoventilate • Suction only as needed, limit passes, pre-oxygenate, +/- pre-hyperventilate (not < 30), use lidocaine when possible • Maintain blood pressure and maintain CPP > 60 • Evacuate intracranial blood • Drain CSF with ventriculostomy when possible Summary of Recommended Practices • Hyperosmolar therapy • Avoid hyperthermia, +/- hypothermia • Prevent seizures • Reserve pentobarbital for refractory conditions • Mid-line neck, elevated head of bead, ? not > 30 degrees • Treat pain and agitation - consider pre-medication for nursing activities • Avoid hyperglycemia • Allow family contact