Gynecologic Pathology as it Relates to General Surgery Lily Shamsnia, MD
advertisement
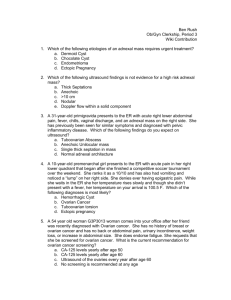
Gynecologic Pathology as it Relates to General Surgery Lily Shamsnia, MD Department of Obstetrics and Gynecology Tulane University School of Medicine GYN vs. General Surgery • Many Gynecologic disorders mimic those of General Surgery, especially regarding etiology of acute and chronic pelvic pain, as well as the diagnosis/treatment of an acute abdomen. • Abdominal pain may be infectious, inflammatory, anatomic or neoplastic Acute right lower abdominal pain in women of reproductive age: Clinical clues Hatipoglu, et. al 290 female patients presenting to ED with acute abdominal pain Patient (n=290), n (%) Age (yr) Acute appendicitis 224 (77.2) 21 (12-24) Perforated appendicitis 29 (10) 22 (14-42) Ovarian cyst rupture 21 (7.2) 24 (15-38) Corpus hemorrhagic cyst rupture 12 (4.2) 21 (13-55) Adnexal Torsion 4 (1.4) 24 (19-30) Alvarado Score Alvarado Score Point Value Abdominal pain migrating to RLQ 1 Anorexia or urine ketone 1 Nausea or vomiting 1 Tenderness in RLQ 2 Rebound tenderness 1 Fever 1 Leukocytosis 2 Neutrophilia 1 Scoring: 0-4: unlikely appendicitis 5-6: consistent with dx of appendicitis 7-8: probable appendicitis 9-10: very probable appendicitis Symptoms/signs of appendicitis similar to many GYN disorders Approach to Acute Abdominal/Pelvic pain in a Female • • • • • History and physical exam Bimanual and speculum exam UPT/ serum bHCG Cervical cultures Radiologic studies DDx pelvic pain of GYN origin • • • • • • • Pelvic Inflammatory Disease (PID) Tubo-ovarian Abscess (TOA) Endometriosis Ruptured or Hemorrhagic Ovarian Cyst Adnexal Torsion Uterine Fibroids Ectopic Pregnancy Pelvic Inflammatory Disease (PID) • Inflammation and infection of the upper female genital tract, including the cervix, fallopian tubes, and uterus. • Peritonitis also may be present. • Early diagnosis and treatment to prevent longterm morbidity is key. • An episode of PID can cause recurrent/chronic PID, chronic pelvic pain, ectopic pregnancy, infertility. PID • Ascending infection from the lower genital tract. – – – – – – – – Neisseria gonorrhoeae, Chlamydia trachomatics, Diptheroids, Gardenella vaginalis, Mycoplasma genitalium, Bacteroides, Anaerobes, Streptococci • > 50% cases have more than one organism isolated PID • Symptoms/signs mimic that of appendicitis due peritoneal irritation and can often be vague/ misleading • Diagnosis missed in up to 35% of patients. • Mucopurulant cervical/vaginal discharge is present with PID PID- CDC Diagnostic Criteria • Minimal Dx Criteria– Pelvic or lower abdominal pain AND – CMT OR uterine tenderness OR adnexal tenderness • Additional criteria: – – – – – – oral temperature >101 F Cervical/vaginal mucopurulent discharge WBC on microscopy of vaginal secretions Elevated ESR Elevated CSR Documented gonorrhea/chlamydia cervical infection • Most specific – Endometrial biopsy showing endometritis – Radiographic imaging showing thickened fluid filled tubes indicative of infection – Laparoscopic abnormalities consistent with PID PID • Ultrasound – Transvaginal preferable – Uterine enlargement/thickened endometrium – Ovarian enlargement (reactive inflammation) – Edematous distended fallopian tubes with hypervascularity on Doppler US • CT scan – Pelvic inflammation and fat stranding, indistinct tissue planes. PID- Ultrasound Ovary Dilated fallopian tube PID- CT scan Right side , normal Left side, thickened/inflamed tubal wall PID- treatment • Outpatient: Ceftriaxone 250 mg IM PLUS Doxycycline 100 mg PO BID x 14 days +/- Metronidazole 500 mg PO BID x 14 days • Inpatient: – A: Cefoxitin 2 g IV q 6 hours PLUS Doxycycline 100 mg PO/IV q 12 hours – B: Ampicillin/Sulbactam 3 g IV q 6 hours PLUS Doxycycline 100 mg PO/IV q 12 hours • Diagnostic laparoscopy vs exploratory laparotomy- If diagnosis is unclear ( i.e. PID vs appendicitis vs TOA), or no improvement with antibiotics PID on laparoscopy Fitz High Curtis • Occurs with pelvic inflammation of PID spreads to right upper quadrant via right paracolic gutter and involves peritoneal surface of liver. • Violin-string adhesions, typically encountered during laparoscopy, typically laparoscopic cholecystectomy Fitz High Curtis Tubo-Ovarian Abscess (TOA) • 35% of women with PID, 20-40 years old, small percentage postmenopausal. • 2/3 are unilateral- may lead to misdiagnosis of appendicitis if on right side. • Initial insult to the female genital tractinoculation and destruction of fallopian tube epithelium a purulent exudate with low oxygen environment favorable for anaerobic organisms. • Inflammatory response induces edema, ischemia, and necrosis of fallopian tube. TOA • Surrounding structures may become involved in the expanding inflammation and walled off abscess, including ovary, round ligament, broad ligament, contralateral fallopian tube and ovary, appendix, bowel, and bladder. • With expansion, rupture of TOA can occur. • TOAs can be the result of non- gynecologic disease, including diverticulitis, appendicitis, inflammatory bowel disease, and surgery. TOA • Polymicrobial: – – – – – – – – E. coli, Bacteroides Peptostreptococcus Enterococcus Klebsiella Staphylococcus Streptococcus H. influenza. • N. gonorrhoeae and C. trachomatis are rarely cultured from TOAs. • Anaerobic bacteria are present in 60-100% of TOA cultures. TOA • Lower abdominal pain (acute vs chronic), nausea/vomiting • +/- fevers/chills- up to 50% of patients are afebrile • If bowel is involved- anorexia/diarrhea • Leukocytosis- present but not reliable indicator • Palpable abdominal/pelvic mass, rebound tenderness/guarding • CMT, mucopurulent discharge, vaginal discharge/abnormal bleeding TOA- Imaging • Ultrasound- sensitivity > 90% for diagnosis. – Transabdominal- larger field of view for identifying adnexal masses. – Transvaginal- detailed view of pelvic anatomy and vasculatyure. • Appear complex, multilocular, cystic with thickened walls and internal echoes/debris. • Tubal and ovarian architecture disordered with destruction of planes between the ovary and developing abscess. • Cogwheel sign- thickening of endosalpingeal folds. TOA- Imaging • CT scanning if diagnosis is unclear- septated tubular structure with thickened walls. • Hydronephrosis/hydroureter may be seen when surrounding tissue is involved with the inflammation. • Gas bubbles within the fluid collection- highly specific for TOA • TOA vs. appendicitis- TOA was highly associated with appearance of abnormal ovary, peri-ovarian fat stranding, small bowel and recto-sigmoid thickening, and free fluid in the pelvis. TOA on US TOA on CT Appendicitis on US Appendicitis- CT Imaging TOA- Treatment • Treat infection and preserve fertility • Mainstay of therapy is antibiotics +/additional drainage procedures ( image guided transabdominal or transvaginal approach) • Parenteral antibiotics until 48 hours afebrile; continuation of oral antibiotics for 14 days TOA- Surgical Treatment • 1) Concern for alternative surgical emergency i.e. appendicitis, cholecystitis, bowel obstruction/perforation • 2) Failure of clinical response after 48-72 hours of medical therapy • 3) Intra-abdominal rupture of TOA- emergent surgery warranted due to hemodynamic instability, sepsis, multi-system organ failure TOA on laparoscopy Endometriosis • Defined as presence of endometrial glands and stroma outside uterine cavity. • Most accepted theory- development is retrograde menstruation. Other theories include coelemic metaplasia of endometrial tissue with lymphatic spread, and transformation of embryonic rests. Endometriosis • Prevalence - 7-10% in general population; up to 50% in infertile women • 60% of women with dysmenorrhea, 87% of women with CPP • Symptoms- dysmenorrhea, dyspareunia, CPP, pain with ovulation, micturition, defection • Risks- early menarche, short menstrual cycles, reduced parity, heavy bleeding • Increased risk- tall /thin women, excess alcohol and caffeine Endometriosis • Most common location of endometrial implants is the ovaries, followed by deep/central pelvis and vesico-uterine pouch • 60% of Stage IV disease involves intestinal tract (rectum, sigmoid, colon, appendix, small bowel) • With Stage IV disease- pain mediated by deep infiltrating endometrial lesions in muscular propria of surrounding organs Endometriosis Treatment • 1st line- NSAIDs and hormonal therapy • If pain is refractory, surgical intervention is warranted, with laparoscopic ablation or removal (preferred) of endometrial implants • With significant bowel/bladder involvement, laparotomy may be required Endometriosis • MRI- superior for detection of endometriomas- hyperintense signal of T1 weighted imaging or hypodense signal of T2 imaging • CT- endometrioma appears as cystic mass with hyderdense clot within • US- used to assess endometrioma involving ovary- hypoechoic cystic structure Endometrioma on MRI Endometrioma on US Endometriosis on laparoscopy Catamenial pneumothorax • Recurrent pneumothorax occurring within 72 hours of onset of menses. • SOB, CP, cough; usually RIGHT sided • Manifestation of thoracic endometriosis, likely via transdiaphragmatic lymphatic/vascular transplantation of endometrial tissue • Confirmed by presence of endometrial glands and stroma within pleura or diaphragm Ruptured/Hemorrhagic Ovarian Cysts • Most common- functional cysts, including corpus luteal cysts/ follicular cysts, which are more prone to rupture due to increased vascularity as part of the menstrual cycle • Rupture typically occurs between 20-26 days of menstrual cycle (i.e. luteal phase, after ovulation has occurred) Ruptured/Hemorrhagic Ovarian Cysts • Mittelschmerz- sensation of pain and release of peritoneal fluid associated with physiologic rupture of corpus luteum, cyst during ovulation • Ruptured cyst- most commonly right sided • Usual symptoms- acute pain, vaginal bleeding, nausea/vomiting, shoulder tenderness • If associated with massive hemorrhage- signs of circulatory collapse Ruptured/Hemorrhagic Ovarian Cysts • Ultrasound- thin wall, anechoic; with hemorrhage and clotting of blood- internal echoes appear with fluid and debris • With massive hemorrhage- free intraperitoneal fluid present, while cyst itself is collapsed Hemorrhagic Ovarian Cysts Ruptured/Hemorrhagic Ovarian Cysts • Hemodynamically stable- conservative management, analgesia, observation • Unstable- emergent surgical intervention, even if diagnosis is uncertain • If active/uncontrollable bleeding presentoophorectomy recommended; otherwise, conservative management with preservation of ovary is preferred Ovarian Torsion • Partial/complete twisting of adnexa around its vascular pedicle ( infundibulopelvic ligament and tubo-ovarian ligament) • Vascular and lymphatic obstruction results, leading arterial occlusion and ovarian necrosis • Right adnexa most commonly involved, possibly due to longer utero-ovarian ligament on the right vs. decreased mobility of left adnexa due to presence of sigmoid colon Ovarian Torsion • Commonly associated with ovarian mass (cyst, neoplasm, etc) as a fixed point around which adnexa may twist • Previous pelvic surgery also increases risk, likely due to post surgical adhesions around which adnexa can twist • Patients with ovarian hyperstimulation syndrome (due to assisted reproductive technology) also at increased risk Ovarian Torsion • Acute pelvic/abdominal pain; prolonged pain associated with high risk of necrosis • Nausea, vomiting, dysuria, urinary retention, frequency, urgency • Low grade leukocytosis/fever less common • Peritoneal signs Ovarian Torsion • Ultrasound- gold standard • Enlarged ovary (>5 cm) with edema • Absent arterial/venous flow is highly specific for torsion • Pelvic free fluid present with infarction/hemorrhage Ovarian Torsion No Doppler Flow Ovarian Torsion “Whirlpool sign” Ovarian Torsion • Preferred surgical treatment- laparoscopic detorsion with salvage of adnexa • Oophorectomy warranted if ovary appears necrotic, ovarian mass present, or there is evidence of peritonitis • If ovary is salvageable, consider ovarian suspension to decrease likelihood of recurrence. Ovarian Torsion Ovarian Torsion Ovarian Torsion in Pregnancy • Adnexal torsion is the most common complication of an adnexal mass occurring during pregnancy, typically in 1st and 2nd trimesters • If ovarian mass without torsion is noted, surgery is performed in 2nd trimester • If torsion is present, surgery is warranted regardless of gestational age Uterine Fibroids • Most common pelvic tumor in women; consist of hormonally responsive smooth muscle cells, which can lead to progression during pregnancy or with hormonal contraceptive use, and typically regress after menopause • Most common symptoms- abnormal vaginal bleeding, pelvic pain and pressure • Hydronephrosis can occur with chronic impingement of ureter Uterine Fibroids Degenerating fibroids that have outgrown/lost blood supply can present as acute abdominal pain Ultrasoundanechoic, irregular cystic spaces within the fibroid, indicating necrosis Ectopic Pregnancy Defined as any pregnancy outside uterine cavity, most commonly in the fallopian tube (ampulla> isthmus> fimbria), abdominal cavity, ovary, cervix, or uterine cornua Typically occur between 6-10 weeks gestation, and is the leading cause of death during the 1st and 2nd trimesters of pregnancy Ectopic Pregnancy • Risk factors- previous ectopic pregnancy, history of PID, previous pelvic surgery, smoking, infertility, intrauterine device use • Symptoms- pelvic pain, vaginal bleeding • Quantitative bHCG- initial test – if >1500 mIU/mL, pregnancy can be seen on transvaginal US – If > 5000 mIU/mL, pregnancy can be seen on abdominal US Ectopic Pregnancy • US evaluation- 1st evaluate if pregnancy is intrauterine; at 5 weeks gestation (corresponding to bHCG between 10002000 mIU/mL) a gestational sac should be visible Ectopic Pregnancy • With ectopic pregnancy- gestational sac/fetal pole +/- cardiac activity seen outside the uterine cavity • Adnexal mass separate from ovary with empty uterus, free fluid in pelvis, tubal “donut” sign and “ring of fire” on Doppler ultrasound Ectopic Pregnancy on US Ectopic Pregnancy- “Ring of Fire” Ectopic Pregnancy • If unruptured and hemodynamically stablecan consider conservative management with medical therapy i.e. Methotrexate with follow up of serial bHCG levels at day 4 and day 7 after injection, and then weekly until negative • If bHCG fails to decrease by 15% from day 4 to day 7 after MTX injection, consider additional MTX injection vs. surgery Ectopic Pregnancy • If ruptured, emergent surgery is indicated, especially if hemodynamically unstable • Depending on degree of patient stability, surgical approach via laparoscopy (preferred) versus laparotomy, with salpingostomy versus salpingectomy • Salpingectomy indicated with uncontrolled bleeding, severely damaged fallopian tube, large gestational sac (> 5 cm) Ectopic Pregnancy Appendicitis in Pregnancy • 1/800 - 1/1500 pregnancies, incidence slightly higher in the second trimester • Appendiceal rupture occurs more frequently in pregnant women, especially in the third trimester -possibly due to inconclusive symptoms/reluctance to operate on pregnant women delaying diagnosis and treatment; associated with higher risk of fetal loss (36% vs. 1.5%) Appendicitis in Pregnancy • Less likely classic presentation, especially in late pregnancy – More GI complaints – Leukocytosis is common with pregnancy • Pain typically originates at McBurney's point regardless of the stage of pregnancy; however, location of the appendix migrates a few centimeters cephalad with the enlarging uterus • In the third trimester, pain may localize to the mid or even the upper right side of the abdomen Appendicitis in Pregnancy • US- wide variation in the diagnostic performance during pregnancy; gravid uterus can interfere with visualizing the appendix and performing graded compression (particularly in the third trimester) • CT imaging- when clinical findings and ultrasound examination are inconclusive and MRI is not available Appendectomy in Pregnancy • Open preferred if late gestation • Laparoscopic – slight left lateral positioning if 2nd trimester and beyond – avoid cervical instrumentation – open entry techniques/ trocar placement under direct visualization – limit intra-abdominal pressure to less than 12 mmHg Cholelithiasis in Pregnancy • Gallstones are more common during pregnancydecreased gallbladder motility/increased cholesterol saturation of bile – Estrogen increases cholesterol secretion – Progesterone reduces bile acid secretion and slows gallbladder emptying, promoting the formation of stones via biliary stasis • In pregnant women with biliary colic, supportive care will lead to resolution of symptoms in most cases, but the symptoms frequently recur later in pregnancy Cholelithiasis in Pregnancy • 1st episode - supportive care vs. cholecystectomy (laparoscopic if in 1st/2nd trimesters) – low risk of fetal mortality and high risk of disease relapse/need for urgent surgery later in pregnancy. • Acute cholecystitis cholecystectomy – If near term- conservative management is preferable as surgery is technically difficult, with plan for cholecystectomy 6 weeks postpartum The End! Questions?