ANORECTAL DISEASES Bernard M. Jaffe, MD Emeritus
advertisement

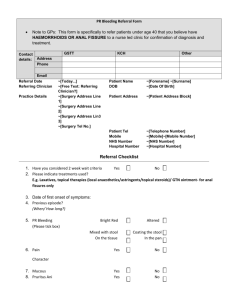
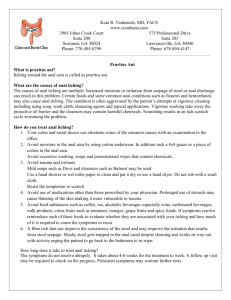
ANORECTAL DISEASES Bernard M. Jaffe, MD Professor of Surgery, Emeritus Tulane University School of Medicine ANAL CANAL • Borders- Coccyx • Ischiorectal Fascia Bilaterally • Female- Perineal Body; MaleUrethra • Disorders Common and Generally Benign • BUT • Painful and Disabling • Divided Into Upper and Lower Segments UPPER VS. LOWER UPPER • Above Dentate Line (Marked by Anal Valves) • Pleated, Folded Mucosa • 12-14 Columns of Morgagni • Anal Crypts Between Columns • Cuboidal Epithelium LOWER • Below Dentate Line • Smooth Mucosa • Absent • Absent • Squamous Epithelium ANAL SKIN • • • • • Continuous with Anal Canal Contains Apocrine Glands Site of Hydradenitis Suppurativa Pain Receptors (Not Stretch) Lesions Drain to Inguinal Nodes VASCULAR • Arterial Supply • Bilateral, Duplicated • Middle and Inferior Hemorrhoidal Arteries Off Internal Iliac • Venous Drainage • Bilateral, Duplicated • Internal Iliac Veins to Inferior Vena Cava ANAL MUSCULATURE • One Tubular Structure Inside Another • Inner- Continuation of Rectal Circular Layer • Extends 1.5cm Beyond Dentate Line • Involuntary • Forms Internal Sphincter • Outer- Continuous Sheet of Striated Muscle of Pelvic Floor • External Sphincter • Voluntary Control HEMORRHOIDS • Abnormal Anal Cushions • Cushions Contain Blood Vessels, Smooth Muscle, Elastic and Connective Tissue • Left Lateral, Right Anterior, Right Posterior Positions • Unknown Causes, Includes Straining • Common During Pregnancy EXTERNAL HEMORRHOIDS • Covered by Anoderm • Distal to Dentate Line • Swell, Causing Discomfort, Difficult Hygiene • Sever Pain Only with Thrombosis INTERNAL HEMORROIDS • Cause Painless Bright Red Bleeding • Prolapse with Defecation • Mucus Secretion • Itching • Pain is Rare (No Mucosal Pain Receptors) HEMORRHOID GRADES • 1◦ Bleeding Diet • 2◦ Prolapse, Bleeding Rubber Band Ligation • 3◦ Prolapse with Hemorrhoidectomy or • Digital Reduction, or Rubber Band Bleeding Ligation • 4.◦ Strangulation Urgent Hemorrhoidectomy OFFICE TREATMENT • • • • • • Dietary Management (for All Grades) Fiber Supplements Local Hygiene Avoidance of Straining Medication to Soften Stool More Extensive- Rubber Band Ligation HEMORRHOIDECTOMY • Indications • Failure of Conservative Measures • Prolapse Requiring Manual Reduction • Strangulation • Ulceration • Commonest Complications • Bleeding • Urinary Retention ANAL FISSURES • • • • • • • Almost Always Directly Posterior If Not- STD’s, Crohn’s, Hydradenitis Associated FindingsSentinal (External) Pile Enlarged Anal Papilla Causes Pain, Mild Bleeding Responds to Sitz Baths, Bulking Agents ABCESSES • Originate in Intersphincteric Plane • Usually From Anal Gland • If Progress Downward to Skin Causes Perineal Abcess • If Progresses to Other Sites • More Complicated • Harder to Treat OTHER SITES OF ABCESS • • • • • Intermuscular- Vertical Tracking Supralevator- Vertical Tracking Tough to Diagnose Ischiorectal- Horizontal Tracking Horseshoe- Circumferential Tracking ABCESS TREATMENT • Drainage is Critical • Superficial Abcess- Office Drainage • Attempt to Localize Site of Origin Within the Anal Lumen • Needle Localization or CT Imaging May Be Necessary to Localize More Complex Abcesses OPERATIVE DRAINAGE • OR Required for • Complex (Horeshoe Abcess) • High (Supralevator) Abcess • Immunocompromised Patients • Patients With Systemic Symptoms FISTULA-IN-ANO • Complicates Anorectal Sepsis in 25% • Originates in Dentate Line in Anal Canal • Presents With Purulent Peri-Anal Drainage • Punctate Indurated Papule With Opening • Inner Opening Identified by Probing at Dentate Line from Drainage Site • May Have Multiple External Drainage Openings TYPES OF FISTULAS • • • • • • Type 1- Intersphincteric Treated by Fistulotomy Type 2- Transsphincteric Type 3- Supersphincteric Type 4- Extrasphincteric Latter 3 Treated With Seton SETON • Monofilament Nylon or Rubber Band • Passed Through Fistulous Tract • Causes Fibrosis and Allows Later (8-12 Weeks) Sphincterotomy Without Loss of Continence • Cutting (Progressively Tightening) Seton Also Acceptable Technique • Difficult Fistulas- Sliding Flap of Mucosa, Submucosa, and Muscle to Cover Internal DIFFICULT FISTULAS • Sliding Flap of Mucosa, Submucosa, and Muscle to Cover Internal Opening • Injection of Fibrin Glue Into Opening • Even With Multiple Openings, There is Generally Only One Internal Opening PILONIDAL SINUS • Midline Sacrocoxxygeal Skin • Acute Abcess • Chronic Sinuses • Rarely Confused With Fistula-in-Ano • Related to Hair, Penetration of Granulation Tissue Into Sinuses • Disease of Young People • Treated by Excision CONDYLOMA ACCUMINATUM • • • • • • Peri-Anal Wart Caused by Human Papilloma Virus Associated With AIDS, Anal Intercourse Difficult to Eradicate- Cautery Podophyllin Significant Risk of Epidermoid Carcinoma HYDRADENITIS SUPPURATIVA • Chronic Inflammatory Process • Occurs in Peri-Anal Area and Other HairBearing Areas • Most Likely Theory- Debris Occludes Apocrine Gland →Purulence → Rupture→ Subqu Infection • Organisms- Strep milleri, Staph aureus, epidermitis, and hominis TREATMENT • • • • • • • Antibiotics Drainage, Debridement Fistulotomy (Distal to Dentate Line) Wide Local Excision With Skin Graft Difficult to Eradicate 30% Recurrence Rate Association With Squamous Carcinoma CROHN’S DISEASE • • • • • • Anorectal Disease in 20% Jeopardizes Continence 2◦ Inflammation Causes Fissures, Abcesses, Fistulas Fistulas Proximal to Dentate Line Can Be First Manifestation of Disease Symptoms- Pain, Bleeding, Soilage, Poor Continence TREATMENT • • • • CONSERVATIVE MANAGEMENT Treat Ileal Crohn’s Dsiease Sitz Baths, Stool Softeners, Analgesics Steroids, 6 M-P, Azothiaprine, Cyclosporine • Avoid Fistulotomy- If Needed, Use Seton • Difficult to Manage- Non-Resposive • Often Extensive EPIDERMOID CARCINOMA • Anal mass With Bleeding, Pruritis • Epidermoid, Basaloid, Cloacogenic, Mucoepidermoid Types • <3cm in Size • 25% Superficial or in Situ • 71% Deep Penetration, 25%Node Positive, 6% Distal Metastases • Increased Frequency in AIDS TREATMENT • Superficial Lesions <2cm- Local Excision • Remainder- Nigro Protocol (Radiation, 5-FU, Mitomycin) • Almost All Respond and TREATMENT • Superficial Lesions <2cm- Local Excision • Remainder- Nigro Protocol (Radiation, 5FU, Mitomycin) • Almost All Respond and Disappear • APR for Failure of Nigro Protocol • Contraindication to RT, Chemo • Deep Invasion • Aggressive Lesion