I.Male Reproductive System Organs Ducts Glands
advertisement
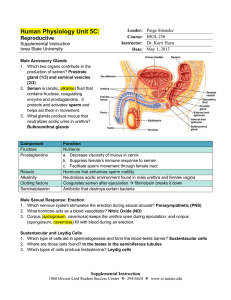
I.Male Reproductive System Organs: testes, ducts, glands & supporting structures Supporting structures include scrotum & penis Ducts: epididymis, ductus deferens, ejaculatory ducts & urethra Glands: seminal vesicles, prostate, bulbourethral glands Figure 23.1 A. Scrotum Pouch that supports the testes Septum separates into separate sections for each testis Sperm requires temperatures 2-3oC below body temperature allows raising and lowering testes to adjust temperature B. Testes Paired oval glands 200-300 lobules containing seminiferous tubules Sperm producing cells and nurse cells (protect sperm) C. Epididymis Stores sperm before ejaculation Comma shaped on top of testes Figure 23.2a Figure 23.2b D. Spermatogenesis Occurs in seminiferous tubules Cell types involved: spermatagonia, sertoli cells & interstitial cells (leydig cells) move into->epididymis Spermatogenesis stages Takes ~65-75 days from first division to release ~300 million /day Life span ~ 48 hrs in female tract Figure 23.3 E. Sperm Structure: Head, middle, tail tail- flagellum = motility Middle - mitochondria = energy Head-chromosomes + acrosomal cap acrosome-enzymes-> penetrating egg Figure 23.4 F. Sperm route Testes ->Epididymis vas (ductus) deferens urethra G. Semen 2.5-5 ml per ejaculation 50-150 million sperm per ml When number falls below 20 million/ml – sterile 7.2-7.7 ph H. Accessory Glands Seminal vesicles- seminal fluidFructose (sperm ATP production + alkalinity (neutralize acid in tracts) 60% of ejaculate Prostate- surrounds upper urethra Increases volume + adds antibiotics Citric acid for energy 25% of ejaculate Bulbourethral glands: More alkalinity + mucus fluid Pre ejaculate 10 % of ejaculate I. Penis Contains urethra- Passage Glans for semen & urine has external urethral oriface Uncircumcised glans covered by prepuce Figure 23.6 II.Female Reproductive System Ovaries: paired organs- produce secondary oocytes ova (after fertilization) Hormones: progesterone & estrogens From same embryonic tissue as testes uterine (fallopian) tubes & uterus vagina External organs (vulva or pudendum) A. Histological Structure of Ovary Germinal epithelium- covers surface Ovarian cortex: connective tissue containing follicles Follicle; oocyte + surrounding cells Surrounding cells nourish oocyte & produce hormones Grows during maturation Graafian follicle ovulation Post ovulation corpus luteum Progesterone, relaxin & inhibin Figure 23.6 Figure 23.7 B. Uterine Tubes Two tubes- extend laterally from uterus End in fringe Fimbriae Fimbriae sweep secondary oocyte into tube Oocyte moved by cilia lining wall Zygote reaches uterus in ~7 days C. Uterus Pathway for sperm & site of implantation Fundus -Dome-shaped area above tubes= Body – tapering central portion Cervix- narrow opening into vagina Uterine cavity- interior of body Vagina extends from exterior to cervix Receptacles for penis and outlet for menstrual flow Fornix- recess surrounds cervix Acid environment- prevents bacterial growth Smooth muscular layer- adjusts for intercourse or birth Thin membrane fold can cover vaginal orifice = hymen Figure 23.9 Perineum & vulva (cont.) Clitoris- small cylindrical mass of erectile tissue & nerves Also contains prepuce & glans External urethral oriface- anterior to vaginal oriface Female Reproductive Cycle 20-34 days- cycles in both ovaries & uterus Ovarian cycle= maturation of follicle, ovulation & corpus luteum formation Uterine Cycle= menstrual cycle controlled by hormones from ovary Estrogens growth of endometrium Progesterone supports endometrium for implantation Combine cycles = Reproductive cycle Figure 23.12 Hormonal Regulation GnRH (hypothalamus) controls GnRH FSH & LH FSH follicle growth & estrogen secretion High estrogen LH surge ovulation LH supports corpus luteum progesterone & estrogen secretion + relaxin & inhibin Inhibin decreased FSH release Gonadotropin releasing hormone= GnRH Comes from hypothalamus and stimulates the release of FSH from pituitary. Hormones FSH – Follicle stimulating hormone Follicle stimulated to start maturing an egg Starts to rise at the end of the cycle and during menstruation. An egg starts to mature. Spikes during ovulation LH- Lutenizing hormone Peaks as estrogen peaks Helps to cause ovulation Hormones Estrogen: Development & maintenance of reproductive structures & secondary characteristics Tells the uterine lining to build up From follicle Progesterone maintains uterine lining for implantation Prepares breast for milk production From corpus luteum hCG- human chorionic gonadotropin Made by embryo Tells corpus luteum to keep making progesterone to maintain lining Relaxin= relaxes uterus- inhibits myometrium Inhibin- inhibits FSH release Phases of Cycle Menstrual phase: ~1st 5 days of cycle Several Ovarian follicles enlarge Decreased progesterone & estrogen uterine arteries constrict endometrium sloughs off Preovulatory- between menstruation & ovulation Ovaries: follicles grow & secrete estrogen & inhibin one dominates Uterus: growth of new endometrium Phases of Cycle (cont.) Ovulation Release of 2o oocyte with LH surge PostovulatoryOvaries: follicle collapses corpus luteum (luteal phase) If no fertilization FSH & LH corpus albicans & decreased Progesterone menstruation Phases of Cycle (cont.) If fertilization & division human chorionic Gonadotrophin (hCG) stimulates corpus luteum secretion Uterus: Progesterone & estrogens complete development of uterus for implantation Figure 23.13