Lecture 21: Dissemination, Virulence, and Epidemiology
advertisement

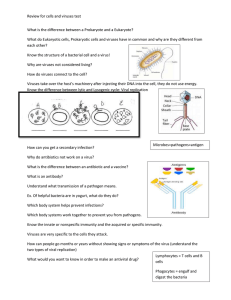
Lecture 21: Dissemination, Virulence, and Epidemiology Text: Flint et al, Chapter 14 General points • To establish a successful infection, viruses must – – – – Find a way to enter the host Find a way to get through the host defences Move through the host Find the right cell types to infect • To spread infection, viruses must – Find a way for new viral progeny to exit infected cells and host – Find a way to survive outside of host Initiation of infection • Sufficient virus must be available – High concentrations. • • – High survivability in harsh exterior environments • • • • Dilution pH changes Dissecation Cells at site of infection must be 1. 2. 3. • A sneeze droplet contains up to 100 million Rhinovirus particles. Similar amount of Hepatitis B in 1ml of infected blood. Accessible Susceptible Permissive Local host defenses must be – – Absent or Initially ineffective Viral Entry: respiratory tract • Common route for viruses • Aerosolized droplets – Coughing, sneezing – Large droplets deposited in nose – Smaller ones further down the Resp. tract • Must overcome – Clearance by mucus – Inactivation by antibodies – Destruction by macrophages. Viral Entry: respiratory tract Fig. 14.2 Viral Entry: alimentary tract • Common route of entry and dispersal • Virus must be resistant to – Stomach acids – Bile bases (detergents) • Destroys most enveloped viruses. • Somehow many Coronaviruses survive – Proteases • Many viruses, e.g. Reovirus particles, are actually activated by intestinal proteases. Viral Entry: into M cells Viral Entry: into M cells • Most of gut is lined with columnar villous epithelial cells. – Apical sides are densely packed with microvilli – “Brush border” coated with glycoproteins, glycolipids and mucus – Difficult to penetrate • M cells: lymphoid cells scattered throughout gut – Thin, absorptive, – Normally transmit antigens to underlying lymphtocytes via transcytosis • Some viruses infect only M cells – e.g. Rotavirus, Coronavirus transmissible gastroenteritis – Lyse M cells, cause mucosal inflammation, diarrhea – Others transcytose through M cells into underlying basal membranes and extracellular space. e.g. Reoviruses – From there, can go to • Lymphatic system • Circulatory system • Rest of host Viral Entry: through Urogenical tract –Physical barriers: mucus, low pH (vagina only) –Viral entry via tears and abrasions due to normal sexual activity –Viruses can infect epithelium and cause local lesions, e.g. some papillomaviruses –Others infect underlying tissues, and invariably spread and persist »Neurons, e.g. herpesviruses »Lymphoid tissue, e.g. HIV Viral Entry: through eyes • • • • Physical barriers: tears, mucus, proteases Entry via abrasions, poor sanitation Most infections are localized: conjunctivitis Herpesvirus Type I infections can spread to neurons and become persistent Viral entry: through skin • Presents formidable physical barriers • Entry via breaks in skin • Abrasions, e.g. papillomaviruses: usually local • Insect bites, e.g. West Nile • Animal bites, e.g. rabies • Behavior: needles, tattoos, body piercing Fig. 14.4 Evasion of host defenses • Active and passive mechanisms • Active: knock out immune mechanisms • Passive: – Overwhelming numbers – Infect immunonaive organs, e.g. Rabies Kinetics of viral replication and immune response Fig. 14.5 Viral Spread • After replication at site of entry, virus can – Remain localized • e.g. rhinovirus in respiratory epithelium – Spread to other tissues • e.g. polio from gut epithelium to neural tissues • Disseminated infection – virus spread to other tissues • Systemic infection – virus spread to many organs • Shedding – release of virus from infected cells/tissues Polarized viral spread • Direction of virus particle release determines how virus will spread • Release at apical membranes: localized or limited infection – e.g. Influenza • Release at basal membranes: disseminated/systemic infections – e.g. VSV Fig. 14.6 Vessicular Somatitis Virus Hematogenous Spread • Spread through the blood. • Virus replicates at site of entry, exits infected cells • Enters bloodstream – primary viremia • Infects other organs, replicates, exits into bloodstream – secondary viremia • Replicates yet again in other organs, exits passed on. Fig. 14.7 Neural spread • Many viruses spread from primary site of infection by entering local nerve endings • Typically, such viruses enter from a nerve ending or axon • Replicate in the cell body • Directionally exit the neuron: retrograde vs. antiretrograde • Routes of entry can be – Neural: poliovirus, herpesviruses – Olfactory: herpesviruses, coronaviruses – Hematogenous: polio, coxackievirus, mumps, measles, CMV Neural spread Box 14.3. anterograde vs retrograde spread Fig. 14.11 pathways of neural spread Fig. 14.12: olfactory spread Organ invasion • From viremia, subsequent replication requires invasion of new cells and tissues • Three main types of blood vessel-tissue interfaces provide routes for invasion 1. Capillary: very tight basement membrane 2. Venule: contains pores through basement membrane 3. Sinusiod: very leaky, macrophages form part of blood-tissue junction Fig. 14.13 Viral entry routes into the liver Fig. 14.15 Virus shedding and transmission Shedding: release of infectious viruses from infected host • Respiratory secretions. e.g rhinoviruses, influenza viruses – Aerosolization – sneezing, coughing – Contamination of fomites by nasal secretions • Saliva. e.g. mumps, cytomegalovirus, rbies – – – – Aerosolization – sneezing, coughing Contamination of fomites – spitting, coughing, wiping hands Kissing, grooming (animals) Animal bites • Feces, e.g. enteric and hepatic viruses – Poor sanitation, food contamination, sexual exchange • Blood, e.g. sindbis viruses (West Nile), Denge virus, hepatitis, HIV – Transmission by biting insects, during sex, childbirth, exposure to contaminated blood • Urine (viruea) – Hantaviruses, arenaviruses • Semen – HIV, some herpesviruses, hepatitis B • Milk – Mouse Mammary tumor virus, Mumps, CMV • Skin lesions – Poxviruses, HSV, varicella zoster, papillomaviruses, Ebola virus Epidemiology • • 1. 2. 3. 4. 5. 6. Definition: The study of the occurrence of a disease in a population. Includes: Mechanisms of viral transmission Risk factors for infection, Population size required for virus transmission Geography Season Means of control Mechanisms of viral transmission • • • • • • • • Aerosol Food and water Fomites Body secretions Sexual activity Birth Transfusion/transplant Zoonoses (animals, insects) Factors that promote transmission • • • • Virus stability Virus in aerosols and secretions Asymptomatic shedding Ineffective immune response Geography and Season • Vector ecology; School year; Home heating season Risk factors • • • • • • • • Age health immunity occupation travel lifestyle children sexual activity Critical population size Numbers of seronegative susceptible individuals Means of control • Quarantine – SARS • Vector elimination – mosquito control and West Nile • Immunization – MMR, DPT, etc… • Antivirals – triple therapy and AIDS