Circulatory Systems: Open vs. Closed, Heart Function
advertisement

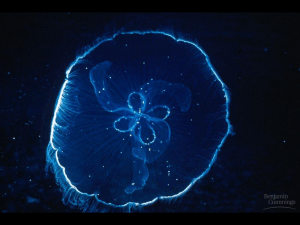
Circulatory systems Gastrovascular cavity thin body walls flagella stir fluid Fig. 9.1 Open circulatory system hemolymph large volume low pressure most invertebrates Closed circulatory system blood small volume high pressure vertebrates some invertebrates Circulatory systems cardiovascular components (pump + tubes) valves, muscles a) External pump •blood pushed by compression of surrounding muscles •direction of flow determined by valves e.g. human leg veins, arthropod limbs b) Peristaltic contractions •blood vessels or peristaltic hearts contract •waves of contractions push blood c) Contractile chamber closed chambers, valves (e.g. vertberate heart) Fig. 9.2 Types of circulatory systems 1. OPEN CIRCULATORY SYSTEM (most invertebrates) Low pressure (< 1.5 kPa) High volume (30% body vol.) Slow velocity Fig. « 9.7 » Electrical conduction in the mammalian heart depolarization (contraction) repolarization (relaxation) Normal pacemaker is the SINOATRIAL NODE Heart beat: begins at SA node spreads through atria delayed at AV node spreads through ventricles Fig. 9.23 2. CLOSED CIRCULATORY SYSTEM (cephalopods, vertebrates) High pressure (>12 kPa) Low volume (5-10%) High velocity Distribution regulation Ultrafiltration Lymphatic system Fig. 9.10 Circulation in fish (water breathing) respiratory and systemic circulations in series sinus venosus – precursor of SA node in mammals Circulation in birds and mammals respiratory and systemic circulations in parallel Four chambered heart Two completely separate circuits pulmonary circuit (low pressure) systemic circuit (high pressure) Anatomy of the mammalian heart adult heart four chambers complete separation of left and right heart fetal heart foramen ovale ductus arteriosus pulmonary circuit not functional CARDIAC VALVES •thin flaps of fibrous tissue •move passively in response to differential pressures •prevent flow of blood Atrioventricular valves RA → RV LA → LV Semilunar valves RV PA Pulmonary SL valve LV DA Aortic SL valve (larger & stronger) Heart Murmurs Valve deformities abnormal blood flow murmurs CORONARY CIRCULATION •heart receives 4-5% of blood pumped •coronary arteries arise at base of aorta •blood enters only during ventricular relaxation due to force of elastic recoil of aorta •blockage of coronary arteries causes heart failure •coronary bypass Electrical conduction in the mammalian heart depolarization (contraction) repolarization (relaxation) Normal pacemaker is the SINOATRIAL NODE Heart beat: begins at SA node spreads through atria delayed at AV node spreads through ventricles Fig. 9.23 GAP JUNCTIONS cells coupled metabolically and electrically via hydrophilic channels Passage of: - inorganic ions - small water-soluble molecules: amino acids sugars nucleotides - electrical signals Fig. 4.2 The structure of gap junctions Fig. 9.25 Electrocardiogram (ECG) tracings P wave depolarization of atrium QRS depolarization of ventricle T wave repolarization of ventricle (repolarization of atrium masked by QRS) CARDIAC CYCLE cardiac contraction (systole, 0.3 sec in human) cardiac relaxation (diastole, 0.5 sec in human) right side of heart left side of heart Fig. 9.19 Pressure changes in the heart and arteries of mammals •greater pressure in left heart (supplies systemic circuit) •lower pressure in right heart (supplies pulmonary circuit) N.B. same volume changes at different pressures Fig. 9.26 STROKE VOLUME (SV) = (end diastolic vol. - end systolic vol.) in healthy humans at rest stroke volume ~ (140 - 60) ml = 80 ml both ventricles eject same volume of blood (total blood volume in humans 5-6 L) SV regulated by: end diastolic volume SV EDV mean arterial pressure SV 1/MAP contractility SV C End-diastolic volume determined by: venous filling pressure venoconstriction, skeletal muscle pump atrial pressure ventricular distensibility filling time Blood Pressures in human circulation usually reported as mm Hg ( = torr) normal range 120-130/80-85 mm Hg (systolic/diastolic pressure) CARDIAC OUTPUT (CO) = stroke volume x heart rate in healthy humans at rest, heart rate ~70 beats/min cardiac output = 80 ml x 70 = 5.6 L/min Frank-Starling Law of the Heart Contractility EDV Increase in EDV causes: • in myocardial stretch • in contractile tension • in ventricular systolic pressure ventricular filling during diastole, ejection during systole heart receives & ejects given volume of blood each cardiac cycle. Fig. 9.28 CIRCULATION How do velocity and pressure change as blood flows from heart through various blood vessels: Geometry of Blood Vessels (dog) Type D(mm) Number Aorta 10 1 Arteries 3 40 Arterioles 0.02 40000000 Capillaries 0.008 1200000000 600 Venules 0.03 80000000 Veins 6 40 Vena Cava 12.5 1 Total area (cm2) 0.8 3 125 60 570 11 1.2 Total volume (mL) 30 60 25 110 220 50 Laminar and turbulent flow in vessels Poiseuille's equation relationship between pressure and flow in small terminal arteries, capillaries, and veins Q (flow rate) = (P1- P2) pr4 8Lη (P1- P2) pressure difference r radius of vessel L length of vessel η viscosity of fluid flow flow resistance = pressure difference r4 1/ distance 1/ viscosity (P1 - P2) Q = 8Lη pr4 Flow & resistance most influenced by vessel diameter Fig. 9.29 COMPLIANCE increased P stretch increased volume increased r decreased resistance increased flow Compliance = D volume/D pressure Venous system: very compliant \volume reservoir large volume changes result in small pressure changes Arterial system: less compliant \ pressure reservoir maintain capillary flow Compliance of veins 24x greater than arteries: (except elastic aortae which dampen pressure oscillations) tunica intima: endothelium tunica media: smooth muscle elastin tunica externa: collagen Fig.9.31 Blood flow in vertebrate circulatory systems •high and variable pressure in ventricle •low pressure, steady flow in capillaries, venules, veins •velocity increase in venous system FUNCTIONS OF ARTERIAL SYSTEM 1. 2. 3. 4. Deliver blood to capillaries Pressure reservoir Dampen oscillations in pressure and flow Selectively control blood distribution Arterial volume & pressure depend on: -cardiac output (filling) -capillary flow (emptying) -capillary flow depends on ∆ P (Parterial - Pvenous) Aorta is a pressure reservoir Arterial blood pressure systolic (max) diastolic (min) Fig. 9.34 Functions of Venous System 1. return blood to heart (skeletal muscle pump) 2. blood storage reservoir (large volume, low pressure) 3. maintain arterial pressure and capillary flow Venous compliance related to large volume ARTERIOLES •control blood distribution to tissues •surrounded by smooth muscle •vasoconstriction, vasodilation Q (flow rate) = (P1- P2) pr4 8Lh nutritional flow waste disposal regulation of cell activities Capillaries · · · · · thin-walled (<0.5 mm) small diameter (7 mm) extensively branched; no cell > 0.1 mm from capillary large surface area low blood velocity minimum diffusion difference maximum surface area and time for exchange except for capillaries in brain, no carrier-mediated transport exchange by diffusion through endothelial cell membrane or through capillary pores Capillary structure muscle, lung, adipose tissue kidney, intestine discontinuous capillary bone marrow, liver, spleen, Fig. 9.32 Regulation of circulation Priorities: maintain continuous perfusion of brain & heart then supply other organs as needed maintain ECF volume & composition hyperemia increased capillary flow ischemia cessation of capillary flow tissue metabolism vessel dilation flow brain and heart continuously perfused, last to be deprived of capillary flow Distribution of cardiac output during exercise Supplying O2 during exercise in human increase O2 delivery via: increased Hb saturation increase O2 extraction increased cardiac output Medullary cardiovascular center receives inputs from Baroreceptors carotid sinus aortic arch subclavian common carotid pulmonary artery Mechanoreceptors atrial ventricular Chemoreceptors arterial ventricular Skeletal muscle afferent fibres Baroreceptors Monitor blood pressure e.g. carotid sinus baroreceptors spontaneous resting AP rate blood pressure = stretch vessel wall AP rate decrease CO via bradycardia and decrease peripheral vascular resistance \ blood pressure (negative feedback) Mechanoreceptors Monitor stretch e.g. atrial myelinated B-fibres spontaneous resting AP rate sensitive to atrial filling rate&volume blood volume venous volume = venous P atrial filling AP rate increase heart rate and increase diuresis \ blood volume (negative feedback feedback) Peripheral Chemoreceptors Monitor O2, CO2, pH in arterial blood primary effect on regulation of ventilation During normal breathing: decrease O2, increase CO2 = decrease pH hyperventilation peripheral vasodilation (except lungs) increased cardiac output During apnea (e.g. diving) decreased O2 peripheral vasoconstriction (except brain and heart) bradycardia decreased cardiac output Baroreceptor reflex Fig. 9.41 Capillary Filtration Fig.9.36 Oncotic P = colloid osmotic P due to [protein] plasma> [protein] interstitial fluid Blood P>Oncotic P Oncotic P> P Blood Consequences of capillary filtration bulk fluid flow in interstitial spaces a v carrying small organic molecules & ions ~85% of filtered fluid is uptaken (except in kidney) but 15% not recovered gradual net loss of fluid from blood and edema SOLUTION? LYMPHATIC SYSTEM - parallels veins in structure, function, and topography - no connection with arterial system - low pressure FUNCTION ·return lymph to circulatory system (3 L/day in humans) ·filter lymph at lymph nodes ·lymphocytes secrete antibodies and destroy cells ·carry chylomicrons from intestine to circulatory system ·carry albumin from liver to circulatory system Fig. 9.37 Causes of Edema Increased blood pressure increases filtration pressure at arterial end of capillaries \ more fluid is filtered Increased tissue protein increases solutes in tissue interstitial fluid \less fluid reabsorbed at venous end of capillaries usually localized edema due to leakage of plasma protein Decreased plasma protein decreases solutes in plasma \less fluid reabsorbed at venous end of capillaries caused by: liver disease (decreased protein production) kidney disease (leakage into urine) protein malnutrition Obstruction of lymph vessels lymph accumulates e.g. infections of filaria round worm Hb Saturation arterial (fully saturated) ~97% venous at rest mild exercise heavy exercise 75% 58% 27% Increased cardiac output (= stroke vol x heart rate) via: stroke volume heart rate In human: at rest heavy exercise trained athlete CO (L) SV (ml) HR (bpm) 5.6 18 5 80 80 100 70 220 50