NHS Greater Manchester Safe & Sustainable Programme AGMA Health Commission 13
advertisement

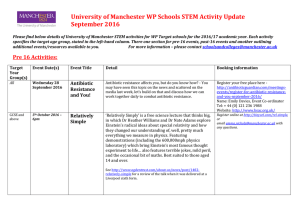
NHS Greater Manchester Safe & Sustainable Programme AGMA Health Commission 13th July 2012 Leila Williams, Director of Service Transformation Partnership Safe & Sustainable Public Health Voluntary Sector Local Authority Scope • Accepted approach of co-design & co-production • Reform of different parts of healthcare system – in parallel & together – each at different stages moving forward • Need to recognise interdependencies but make and maintain momentum in each area • Make progress locally where change can be made locally Potential barriers to success include: Barriers Mitigating action Loss of focus • Clear understanding of scope and how related work programmes fit together Public resistance to change • Clear messages being developed • Programme of communication & engagement across Greater Manchester • Shared responsibility for delivery Politics & elections • MPs briefing • Civic leadership within whole system leadership framework • Consultation planned for 2013 Organisations’ perceptions • Involvement of provider organisations A public facing name .... • together with public & residents, partners, providers • healthier citizens & organisations • ‘says what it does on the tin’ Safe & Sustainable Framework: Step 1 Completed by July 2012 Identified & established a Clinical Congress Completed initial Case for Change Template Reviewed & Sourced Data Developed DRAFT Case for Change Document Amended DRAFT Case for Change based following Clinical Congresses Case for change snap shot: Variation in practice & outcomes • 550 lives a year in Greater Manchester (& Cheshire) could be saved if the UK meets the European average survival rates – about 1 per practice – late presentation a key factor • Emergency general surgery is carried out in 10 acute hospitals in Greater Manchester, but not always with consultant staff present and not always with routine admission to a critical care bed after surgery, even for high risk cases - leads to inconsistent quality of care and poorer patient outcomes • The number of emergency medical readmissions within two days of discharge has gradually increased over the last two years Safe & Sustainable Variation in practice & outcomes • Centralisation of stroke services for 1/3 of patients is saving 250 lives a year in GM. Most District Acute Stroke centres are failing to deliver key performance indicators. Plans to centralise remaining services to save more lives • Patients admitted to cardiology wards have a 20% lower mortality rates compared to those admitted to general wards • Even after Making it Better, we still have children’s inpatient units that average less than 13 overnight beds filled (summer and winter)! Safe & Sustainable Step 1: Where are we now? Step 4: Step 2:Where do we want to be? Step 3: What is the Gap? THE STORY for Public Discussion A conversation about .... Change is imperative & change is good Our commitment to We know because ourwe GM residents We can’t achieve this have already seen it What does best care without you But more change islook like? We all need to take needed Creating a shared responsibility to create vision better services What Everyone needs tochanges may be needed to achieve the take an active contribution to health best? Discussion