Celine Bicquart Advanced Laryngeal
advertisement

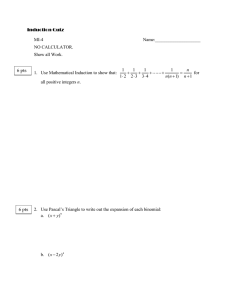
Celine Bicquart Advanced Laryngeal Cancers October 19, 2006 Overview of Talk Case Presentation Anatomy and Lymph Node Drainage of the Larynx Overview of Laryngeal Epidemiology Staging of Patient Review of Literature Patient Treatment Plan DS ID: 49 y/o male HPI: Hoarse since January 2006 with odynophagia and dysphagia. 10 lb wt loss in August. Referred to ENT at OHSU. 8/16/06- CT neck- 17 x 14mm enhancing soft tissue lesion filling L piriform sinus. Involves L. supraglottis, L glottis, L subglottis with midline focal area of destruction of thyroid cartilage. +Posterior L level III adenopathy. HPI cont’d FNA of L neck node- Metastatic poorly- differentiated SqCCa with high N:C ratio. 9/15/06- Total larynectomy, L neck dissection II-IV, L hemithyroidectomy, Pec major flap. Path: 4.3cm G3 Invasive Squamous Cell, negative margins. Invades through thyroid cartilage, but thyroid gland uninvolved. 4/14 Level II. +ECE. 2/6 Level III. –ECE. 1/8 Level IV. –ECE. +perineural invasion. Indeterminate angiolymphatic space invasion. PMH: Seizures Meds: Dilantin 300mg qd, Oxycodone q3-5h, Nicotine patch 21mg qd Allergies: NKDA PSH: Laryngectomy SH: Single. Lives in Portland. Receives disability, previously did odd jobs. Smoked 1.5ppd x 30y. Cut back in 05/06. Now uses nicotine patch. Drinks 1-2 drinks qd. PE: Healing incisions of left neck dissection and pec major flap. Stoma appears patent. No fistula noted. No discharge from stoma noted. Supraglottis- high incidence of LN metastasis: jugulodigastric, jugulocarotid, juguloomohyoid. GlottisSubglottis- 1 ant: mid and lower jugular to prelaryngeal node ???? 2 post: paratracheal 12000 new cases yearly- 2% of all cancers 60-65% glottic 30-35% supraglottic 5% subglottic M:F p53-mutated in 47% smokers Signs and Symptoms Hoarseness- MC presenting sx of glottic ca Sore throat- MC presenting sx of supra ca Odynophagia- MC presenting sx of supra ca Foreign Body Sensation Dysphagia Stridor Pain Hemoptysis Otalgia- via vagus and nerve of Arnold. Weight loss Risk Factors: Airway obstruction -Tobacco -Alcohol Evaluation and Work-up Complete H&P Assess for adenopathy in neck. Loss of Thyroid click: sign of post-cricoid extension. Mass over thyroid signifies thyroid cartilage invasion. Indirect mirror exam for visualization. “EEEeeeeee.” Fiberoptic flexible laryngoscopy. CXR for metastatic evaluation CBC, LFTs. If abnormal, may get CT abd, bone scan. CT, MRI Performed before bx. MRI is better to delineate soft-tissue extent of primary tumor. CT is better for evaluating bone invasion. CT also very useful for detecting subclinical LN metastasis. Want to look for pre-epiglottic, periglottic space invasion, subglottic and extralaryngeal extension, and cartilage invasion. Direct laryngoscopy with bx for tissue dx, disease extent. Usually performed as part of panendoscopy to r/u multiple tumors. Squamous Cell Carcinoma of the Larynx 95% SqCCa. TVC- well to mod-diff Supra and subglottis- more poorly diff Following surgery, DS has had a slow recovery. FT still in place secondary to residual swelling. Patient reports dysphagia. Patient also reports dyspnea on exertion. Clinical Question My patient’s cancer was a T4, for which the standard of care had been a total laryngectomy followed by adjuvant radiation. TL results in disease control rates of 70-80%; and with TE punctures for voice restoration, patients can eventually regain their verbal communication skills. In light of this good disease control rate, is there a way to obtain equivalent survival while sacrificing less quality of life? Looked at induction chemo + definitive RT vs. conventional TL + PORT Stratified according to KPS, Stage III vs. IV, Nodes, tumor site 322 T3 or T4 SqCC 2 cycles cisplatin + 5-FU + Response (CR of PR) Larynectomy + RT: 50, 60, 65-73.8cGy No response 1 more cycle + RT 66- 76 cGy Salvage laryngectomy Patients with no response or locally recurrent disease underwent salvage laryngectomy. VA Trial After two cycles of chemotherapy: CR 31% and PR 54%. (Overall response 85%) At median f/u of 33 months, the estimated 2-year survival was 68 percent (95% CI, 60 to 76%) for both tx groups (P = 0.9846) VA Trial VA Trial Toxicity due to RT was similar in both arms. Grade 2 mucositis slightly higher in chemo group 38% vs. 24% in TL group. Higher incidence of surgical complications in salvage cases after RT vs. just after chemo. VA Trial Patterns of recurrence differed significantly between the two groups, with more local recurrences (P = 0.0005) and fewer distant metastases (P = 0.016) in the chemotherapy group than in the surgery group. A total of 59 patients in the chemotherapy group (36 percent) required total laryngectomy. So….64% preserved their larynx without compromising OS. Induction chemo does enhance the effectiveness of RT, but since no direct comparison was made between chemoRT vs. RT alone, the role of chemo remains uncertain. Determine if chemo followed by XRT was comparable with standard surgery +PORT in pts with T2-4, N0-2b SCCA of the pyriform sinus or AE fold Multi-centered, prospective, randomized trial T2-4 SqCCa of pyriform sinus of AE fold 100 induction chemo x 3 cycles 94 TL, PP + PORT CR: XRT PR or CR assessed after each cycle. If after any cycle, no response, went directly to surgery. Only CR went on to XRT EORTC Trial 97/100 pts. started chemo as randomized. 60/97 proceeded to complete chemo + RT. (70Gy, 65Gy) 8/97 required surgical salvage. (55Gy, 60Gy) 92/94 pts. had surgery as randomized. 89/92 had post-op RT. (60Gy) Chemotherapy complete responders were more frequent among those with T2 disease (82%) than those with T3 (48%) or T4 (0%) disease. 3y Disease Free Survival CI: 0.52-1.43 Chemo 43% + RT S+ 31% PORT 3y Overall survival chemo (57%)>surgery (43%) at 3 years but equal at 5 years. NB- small number of pts. at 5y. CI: 0.50- 1.48 Chemo 57% + RT S+ 43% PORT 5y 25% 27% 5y 30% 35% No difference in locoregional failure. Increase in distant mets in surgery group (36%) compared to (25%) in chemo arm. p<.041 Survival with functional larynx with no LR, tracheostomy, FT, gastrostomy at 3 and 5 years = 28% and 17% respectively. Rate of functional larynx in those who died of causes other than local disease progression and died with a functional larynx at 3 and 5 years= 42% and 35% respectively. EORTC study: conclusions Induction chemo is safe for hypopharyngeal cancer. Fewer distant mets and increased time until mets appear CR: T2 (82%) > T3 (48%) > T4 (0%) Conclusions so far… Organ preservation is possible Role of induction chemo is still not exactly known. Distant metastases decreased, and time to DM increased. EORTC trial had small number of patients. Lower larynx preservation rates in the EORTC was a result of more stringent selection criteria. Determine role of induction chemo vs concurrent chemo vs radiation alone in laryngeal preservation for pts with stage 3 and 4 SqCCa of the larynx T1 and high-volume T4 tumors where excluded (>1cm into tongue base or penetrating cartilage invasion) Multi-center, prospective, randomized -cisplatin 100mg/m2; 5-FU 1000mg/m2 -For concurrent: cisplatin given on day 1,22,43 of RT -RT to primary: 70Gy in 35 @2Gy -RT to neck, supraclav, post. neck: 50Gy -Salvage RT for those who failed induction chemo was 5070Gy -Questionnaires were filled out at baseline and at each f/u. Induction Chemo Arm 168/174 patients received induction chemo. 144 had either a CR (21%) or PR (64%), allowing them to receive PORT. 24/168 patients who could not go onto RT. Only 7 went directly to RL. 11/24 received chemo/RT, and all had CR, and of these, only 1 needed TL. At end of RT: 150/174 (86%) had CR. Concurrent ChemoRT arm 120/172 (70%) received all 3 doses cisplatin. 40/172 (23%)received 2 doses. At end of RT: 154/172 (90%) had CR. RT alone arm At end of RT: 148/172 (86%) had CR. 2 and 5 year overall survival did not differ • 76% vs 74% vs 75% at 2 years • 55% vs 54% vs 56% at 5 years Disease Free Survival Concurrent 2y 52% p<.02 61% p<.006 5y 38% 36% RT alone 44% 27% Induction # LF LCR Induction 61 64% Concurrent 35 80% RT alone 72 58% Concurrent resulted in significantly fewer LRs compared to both induction chemo and RT alone. Concurrent vs Induction p<.02. Concurrent vs. RT alone p<.001 No statistical difference between induction and RT alone arms. Effect on Distant Metastases 2y 5y Induction 9% 15% Concurrent 8% 12% 16% 22% p<.03 RT alone Chemo reduced the rate of DMs. The only statistically significant difference was between the concurrent vs. RT alone arm. p<.03 number Laryngeal Preservation at 3.8y % Induction 125/173 72% Concurrent 145/172 84% RT alone 116/173 67% IMPORTANT!! Induction chemotherapy followed by RT when compared to RT alone, did not significantly improve the rate of laryngeal preservation. Conclusion from RTOG 91-11 Concurrent chemoRT is superior to both induction chemo and RT alone in regards to locoregional control, laryngeal preservation, and distant metastases. Induction chemo showed benefits in only improving DFS, and decreasing rate of DMs. No effect on LR or OS. Overall survival does not differ significantly between treatment arms. (76% at 2y) Concurrent chemo does cause twice as severe mucosal effects, potentially contributing to delayed recovery of swallowing in this group. Is laryngeal preservation (LP) with induction chemotherapy (ICT) safe in the treatment of hypopharyngeal SCC? Final results of the phase III EORTC 24891 trial. Journal of Clinical Oncology, 2004 ASCO Annual Meeting Proceedings (Post-Meeting Edition). Vol 22, No 14S (July 15 Supplement), 2004: 5531 Chemo + RT 5y PFS 10yPFS 32% 11% 8.5% S + PORT 26% 5y OS 10y OS Chemo + RT 38% 13% S+ PORT 33% 14% Ultimate disease control, including successful salvage after XRT, was not significantly different between both arms. As of 12/2003, 14 % of pts in arm 1 and 17 % of pts in arm 2 were still alive. The hypopharynx SCC evolution was the cause of death in 43 pts in arm 1 and in 41 pts in arm 2. In arm 2 survival with a functional larynx in place was 22 % at 5y and 9 % at 10y. Conclusions: this final analysis has confirmed the preliminary results with similar survival curves as compared with conventional treatment and allowed 2/3 of the survivors to retain their larynx. Additional therapies Molecular targets have been identified which may hold promise in the treatment of H&N SqCCa. Overexpression of EGFR is recognized in more than 95% of SqCCas. The EGFR and its ligands, EGF and TFG alpha are important in cell proliferation, adhesion, invasion and angiogenesis. Administration of the EGFR monoclonal antibody (cetuximab) has been shown to increase radiosensitization, decrease tumor cell line growth and increase apoptosis. Other novel chemotherapeutics include agents to inhibit tyrosine kinase, angiogenesis inhibitors, and agents that have selective toxicity to hypoxic cells. Function and Quality of Life Preserving the larynx is great, but not as great if the larynx is not effective. How well does it function after concurrent chemoRT? How do patients feel about their ability to communicate and swallow? Long-term Quality of Life After Treatment of Laryngeal Cancer Jeffrey E. Terrell, MD; Susan G. Fisher, PhD; Gregory T. Wolf, MD; for the Veterans Affairs Laryngeal Cancer Study Group . Arch Otolaryngol Head Neck Surg. 1998;124:964-971 1998 follow up: 46/65 surviving pts, 71% RR • 25 surgery+PORT, 21 experimental arm • HNQOL, SF-36 General Health Measure Short Form, Beck Depression Inventory, alcohol and smoking surveys. Quality of Life f/u of VA Study Those with larynx fared significantly better from the standpoint of speech communication. At 2 years post-treatment, patients with successful organ preservation had regained their pretx level of functioning for 2/3 measures tested (intelligibility and reading rate) and exceeded pretx performance on the 3rd (a communication profile used to assess general communication status). TL + PORT pts had a decrease in all 3 speech communication-related measures despite availability of all modes of speech rehabilitation and therapy. Measures of swallowing dysfunction were similar between both arms. Quality of Life f/u to VA study Pts with successful organ preservation: had better scores on all domains of the SF-36 compared to those who underwent TL. scored significantly better on the bodily pain and mental health domain of the SF-36. scored significantly better on the emotion domain and their impression of their response to treatment on the HNQOL survey. At long-term f/u, 10 of 45 patients had BDI scores consistent with moderate or severe depression. 9 of those 10 had undergone TL. Conclusions from VA Study Better QOL in the CT+RT appears to be related to more freedom from pain, better emotional well being, and lower levels of depression than to preservation of speech function RTOG91-11 Speech Percentages of speech impairment at 1 and 2y. Induction 1y 2y 6% 3% Concurrent 11% 6% RT alone 8% 13% No difference among 3 groups in regard to speech at 12 or 24m. Moderate speech impairment: difficulty in pronouncing some words and being understood on the telephone. RTOG 91-11-Laryngeal Function @1y Soft foods Induction No swallow 9% 0% Concurrent 23% 3% RT alone 15% 3% No difference in groups’ QOL 2-yr all three groups similar with 16%, 15%, 14% reporting difficulty swallowing Grade and frequency of toxic acute effects was similar in the induction and RT alone arms: mostly grade 3 in-field effects on skin and mucous membranes. Concurrent chemoRT had chemo-related toxic acute effects (neutropenia, severe N/V, increased rates of severe radiation-related mucosal, pharyngeal and esophageal effects. Rates of late toxic effects were similar among groups. Patients who are treated with larynxpreserving modalities are still at risk of having to undergo salvage laryngectomy in the future. In these patients, is there any added morbidity associated with salvage laryngectomy? Danish Society for Head and Neck Oncology (2003) Wanted to look at surgical outcome of 472 pts with salvage laryngectomy after XRT from 1987-1997 Specific outcome looked at was development of pharyngocutaneous fistula. 89 fistulas lasting > 2 weeks; Overall fistula rate = 19% Number of TLs per year decreased linearly (from 58 to 37), whereas the annual number of fistulae increased slightly (from 7 to 11). • RR in 1987 =12% • RR in 1997 =30% •Grau C, Johansen LV, Hansen HS, Andersen E, Godballe C, Andersen LJ, Hald J, Moller H, Overgaard M, Bastholt L, Greisen O, Harbo G, Hansen O, Overgaard J. Salvage Laryngectomy and Pharyngocutaneous Fistulae after Primary Radiotherapy for Head and Neck Cancer: a National Survey From DAHANCA. Head and Neck. Sep 2003. 25:711-716. Danish Study Increased rate attributed to: • Higher stages offered XRT as definitive therapy • Decrease in individual surgical experience with TL Other significant RFs for fistulae included: -younger patient age - primary advanced T and N stage. RR 2x’s higher in initial T3-4 than T1-2 - nonglottic primary site. Fistula OR 2.08 Surgical complication rates were low. No differences in systemic complications between treatment arms Complications independent of the time from the end of treatment to TL Fistulas occurred in: • Arm 1 = 25% • Arm 2 = 30% • Arm 3 = 15% Conclusions from RTOG Salvage Salvage post laryngeal preservation has acceptable morbidity. 1/3 will develop fistula Locoregional control is excellent: 74%, 74%, 90% Overall Survival for TL patients at 2y: 69% 71% 76% Conclusions from RTOG Salvage Survival following salvage laryngectomy not influenced by initial organ preservation treatment. Treatment of DS Although had TL, needs post-op RT: -cartilage invasion -perineural invasion -multiple positive nodes -nodes with ECE He will be treated on RTOG 0234: Surgery + RT + Cetuximab followed by either docetaxel or cisplatin. Setup of Radiotherapy of the Larynx Patient supine. Face mask on. Borders: superior- 2cm above mastoid tip inferior- bottom of cricoid cartilage posterior- behind spinous process Off cord at 40Gy. Cord block on laterals. Wedge used. Boost stoma. Dose Plan BEV Supraclav BEV- Lateral Side Effects of RT to larynx Soreness Dysphagia Odynophagia Erythema, Desquamation of Neck Weight Loss Acknowledgments Dr. John Holland Dr. Carol Marquez Dr. Charles Thomas Dr. Arthur Hung Dr. Marsha Crittenden Dr. Parag Sanghvi Dr. Tarka McDonald Dr. Patrick Gagnon Dr. Sam Wang Lori Ismach Tony He