Pharmacotherapy for Post-Traumatic Stress Disorder Presented by: Ann Wheeler, PharmD, BCPP Date: 01/14/2016
advertisement

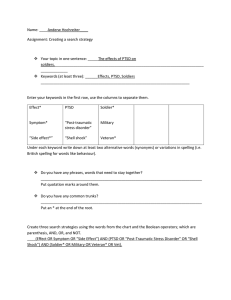
Pharmacotherapy for Post-Traumatic Stress Disorder Presented by: Ann Wheeler, PharmD, BCPP Date: 01/14/2016 Disclosures and Learning Objectives Learning Objectives: • Know the two classes of medications most helpful for PTSD • Be able to discuss the benefits of second-line treatment alternatives Disclosures: Dr. Ann Wheeler has nothing to disclose. PTSD in the Primary Care Setting • Discuss step-wise approach in treatment of PTSD • Gold standard • Indicated medications • Strength of evidence • Second-line treatment recommendations • Topic for next time Pharmacologic Interventions Psychotherapy (CBT) remains the gold standard treatment for PTSD • All of the existing guidelines (6 out of 6) agree that trauma-focused psychological interventions are effective, empirically supported first-line treatments for PTSD • Less agreement among guidelines in regards to pharmacologic interventions • 50% agree that SSRIs are first-line (VA/DoD, APA, ISTSS) • IOM guidelines found minimal evidence for all pharmacologic treatment options Pharmacologic Interventions General Considerations for Pharmacotherapy: • Main goal is to minimize symptoms rather than cure PTSD • Hyperarousal symptoms (nightmares, etc) are the most likely to respond • Medications should never replace therapy unless it is ineffective or declined • Patient preferences need to be incorporated into shared decision-making because they can influence treatment adherence and therapeutic response http://www.thecarlatreport.com/printpdf/5050 http://www.publichealth.va.gov/docs/vhi/posttraumatic.pdf http://www.nice.org.uk/guidance/cg26/resources/guidance-posttraumatic-stress-disorder-ptsd-pdf Pharmacotherapy: Strength of Evidence Drug Class Drug Alpha Blockers Anticonvulsants Antipsychotics SNRIs PTSD Sx Remission Loss of PTSD Dx Prazosin -- -- -- Divalproex -- -- -- Lamotrigine -- -- -- Tiagibine -- -- -- Topiramate M -- -- Olanzapine -- -- -- Risperidone L -- -- Desvenlafaxine -- -- -- Duloxetine -- -- -- Venlafaxine M M -- Strength of Evidence: M=Moderate; L=Low; -- =Insufficient Pharmacotherapy: Strength of Evidence Drug Class Drug PTSD Sx Remission Loss of PTSD Dx SSRIs Citalopram -- -- -- Fluoxetine M -- -- Paroxetine M M -- Sertraline M -- -- TCAs All -- -- -- Other ATDs Bupropion -- -- -- Mirtazapine -- -- -- Nefazodone -- -- -- Trazodone -- -- -- All -- -- -- Benzodiazepines Strength of Evidence: M=Moderate; L=Low; -- =Insufficient Pharmacotherapy: Strength of Evidence Outcome Measure Inducing remission Paroxetine X Venlafaxine X Improving depressive symptoms X X Improving functional impairment X X Improving quality of life X Psychological and Pharmacological Treatments for Adults With Posttraumatic Stress Disorder (PTSD). Comparative Effectiveness Review No. 92. AHRQ Publication No. 13-EHC011-EF. Rockville, MD: Agency for Healthcare Research and Quality; April 2013. www.effectivehealthcare.ahrq.gov/reports/final.cfm. Pharmacology for PTSD: Antidepressants Treatment Recommendations • APA and VA recommend SSRIs as first choice when medications are indicated. Ideal for comorbid MDD. • Sertraline and paroxetine are the only SSRIs with FDA approval for PTSD • Dosing sertraline 50 – 200mg/d, paroxetine 20 - 60mg/d Response • Most studies show a modest response (60% response, 40% remission) http://www.thecarlatreport.com/printpdf/5050, http://www.publichealth.va.gov/docs/vhi/posttraumatic.pdf http://www.nice.org.uk/guidance/cg26/resources/guidance-posttraumatic-stress-disorder-ptsd-pdf http://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/acutestressdisorderptsd-watch.pdf Pharmacology for PTSD: Other ATDs Studies with other antidepressants are mixed • • • Evidence supports use of venlafaxine (75 – 300mg/d) NICE recommends mirtazapine, amitriptyline and phenelzine first-line; however less evidence supporting use No evidence for use of bupropion Sleep may be least likely to respond to SSRI • Consider adding mirtazapine (low dose), trazodone, or a low dose sedating TCA like amitriptyline/doxepin http://www.thecarlatreport.com/printpdf/5050 http://www.publichealth.va.gov/docs/vhi/posttraumatic.pdf http://www.nice.org.uk/guidance/cg26/resources/guidance-posttraumatic-stress-disorder-ptsd-pdf http://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/acutestressdisorderptsd-watch.pdf Pharmacology for PTSD: Antipsychotics Should not be used first-line; should not be used as monotherapy; exception is use for psychotic sx • • Sedating atypicals most likely to show benefit Risperidone is the most researched. VA revised guideline: • • CI for use an adjunctive agent—potential harm exceeds benefits. There is insufficient evidence to recommend any other AAP as an adjunctive agent for PTSD. Other medications are better choices as sedatives http://www.thecarlatreport.com/printpdf/5050 http://www.publichealth.va.gov/docs/vhi/posttraumatic.pdf http://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/acutestressdisorderptsd-watch.pdf Pharmacology for PTSD: Mood Stabilizers Often shown to be ineffective, especially as monotherapy. • Indicated for bipolar disorder w/ or w/o PTSD. • Trials showing effectiveness are typically open-label • Notably, valproate (Depakote) no better than placebo. • Topiramate may be helpful for nightmares and flashbacks. Currently listed as having no demonstrated benefit in VA/DoD Practice Guideline. May be helpful in those dually diagnosed with an alcohol use disorder. http://www.thecarlatreport.com/printpdf/5050 http://www.publichealth.va.gov/docs/vhi/posttraumatic.pdf http://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/acutestressdisorderptsd-watch.pdf Pharmacology for PTSD: Anti-Adrenergics More helpful in the short term Typically associated with less stigma May help with hypervigilance, sleep disturbance (nightmares) and activation • Propranolol 10 - 40mg po 3-4x/day • Clonidine 0.1 - 0.3mg po bedtime and PRN • Prazosin 1 - 3mg po bedtime • Guanfacine not supported in studies http://www.thecarlatreport.com/printpdf/5050 http://www.publichealth.va.gov/docs/vhi/posttraumatic.pdf http://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/ acutestressdisorderptsd-watch.pdf Central alpha-adrenergic agonists (e.g. clonidine) reduce sympathetic outflow from the alpha-2 receptor sites in the CNS, thus decreasing peripheral vascular resistance and slowing the surge of catecholamines. Prazosin is a central and peripheral alphaadrenergic antagonist. Adrenergic Agents Medication Dosing Adverse Effects Monitoring Propranolol 10 - 40mg po TID-QID Fatigue, dizziness constipation, bradycardia, hypotension, depression, insomnia, weakness, disorientation, nausea, diarrhea, hypersensitivity reaction, purpura, alopecia, impotence BP, HR CYP 2D6 substrate (non-selectively antagonizes beta-1 and beta-2 adrenergic receptors) Clonidine 0.1 - 0.3 po qhs Somnolence, headache Hypotension, abdominal pain Fatigue, nightmares, nausea URI, irritability, throat pain, insomnia, constipation, emotional disturbance, xerostomia, bradycardia, dizziness, temperature elevated, diarrhea, otalgia, sexual dysfxn, withdrawal sx (stimulates alpha-2 adrenergic receptors) Prazosin (antagonizes peripheral alpha-1 adrenergic receptors) 1 - 3mg po qhs Hypotension, first-dose asthenia, dizziness, nausea, palpitations, headache, somnolence, hypotension (orthostatic), impotence, priapism, urinary frequency, dyspnea, arthralgia, myalgia Cr at baseline; vital signs frequently if cardiac conduction disturbance; HR, BP at baseline, after dose increases, then periodically BP Pharmacology for PTSD: Benzodiazepines May be helpful for sleep in the short-term (≤5 days), BUT… Avoid in active or recent substance abuse • SA in 40% of PTSD (75% if combat-related) Risks: • Potential disinhibition, difficulty integrating the traumatic experience, interfering with the mental processes needed to benefit from psychotherapy, increased falls and mental clouding in the elderly, psychomotor and cognitive impairment, and dependence/addiction Minimal evidence for actual benefit Little evidence for or against buspirone http://www.thecarlatreport.com/printpdf/5050, http://www.publichealth.va.gov/docs/vhi/posttraumatic.pdf Future Research • Glucocorticoid receptors—modulate the effects of stress and development of PTSD • Neuropeptides: corticotropin releasing factor (CRF), adrenocorticotropin hormone (ACTH), substance P, neuropeptide Y—improve resiliency of the brain to the effects of trauma. BBB is a challenge. Intranasal oxytocin has demonstrated some benefit in decreasing hyperarousal symptoms. • D-cycloserine may facilitate extinction of conditioned fear • Memantine (Namenda)—prevents neurodegeneration by protecting against glutamatergic destruction of neurons through its antagonism of the NMDA receptor. May be useful in preventing hypothesized neurodegeneration in the hypothalamus and memory loss in PTSD. General Considerations Define realistic treatment goals: • Reduction in PTSD symptom severity • Suicidal behavior • Substance misuse • Social isolation • Comorbid psychopathology • Global function/quality of life Assess response using validated scales General Considerations Common clinical barriers • Fear of possible side effects (e.g. sexual side effects) • Feeling medication is a “crutch” and that taking it is a weakness • Fear of being addicted • Taking only occasionally when symptoms get severe • Using “self medication” General Considerations When to discontinue treatment: • Effective treatments (treatment goals have been met) should be continued for a significant period of time • Generally >1 year • Those with early robust response may consider shorter duration General Considerations When to discontinue treatment: • Intolerable side effects • Lack of treatment effectiveness • Partial effectiveness • Switch vs. augmentation strategies • Augmentation—difficult to determine if effectiveness is from 2nd agent or from a combination of the two. Only way to determine is to slowly taper first agent. General Considerations First-line • SSRIs Second-line — examine symptoms Symptoms Drug Class Selection Excessively aroused, hyperreactive, dissociative episodes Adrenergic agent Fearful hypervigilant, paranoid, psychotic Atypical antipsychotic Comorbid major depression Other antidepressant (venlafaxine) Labile, impulsive, aggressive Mood stabilizer Psychological and Pharmacological Treatments for Adults With Posttraumatic Stress Disorder (PTSD). Comparative Effectiveness Review No. 92. AHRQ Publication No. 13-EHC011-EF. Rockville, MD: Agency for Healthcare Research and Quality; April 2013. www.effectivehealthcare.ahrq.gov/reports/final.cfm. Pharmacologic Treatment of PTSD Treatment Considerations First-line treatment recommendation Psychotherapy (CBT) First-line pharmacologic treatment options SSRIs (dosing is similar to depression) • Best evidence with paroxetine Second-line pharmacologic treatment options Define realistic treatment goals and monitor for improvement • • • • • • Reduction in PTSD symptom severity Suicidal behavior Substance misuse Social isolation Comorbid psychopathology Global function/quality of life The End Somatic Symptom Disorder 1/21/16