Pharynx
advertisement
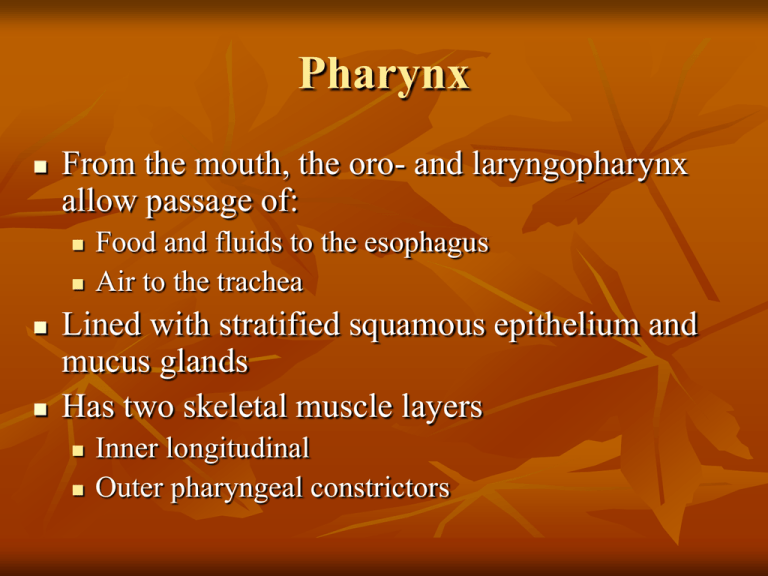
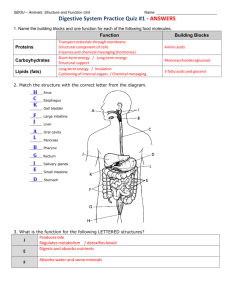
Pharynx From the mouth, the oro- and laryngopharynx allow passage of: Food and fluids to the esophagus Air to the trachea Lined with stratified squamous epithelium and mucus glands Has two skeletal muscle layers Inner longitudinal Outer pharyngeal constrictors Esophagus Muscular tube going from the laryngopharynx to the stomach Travels through the mediastinum and pierces the diaphragm Joins the stomach at the cardiac orifice Esophageal Characteristics Esophageal mucosa – nonkeratinized stratified squamous epithelium The empty esophagus is folded longitudinally and flattens when food is present Glands secrete mucus as a bolus (compacted food product) moves through the esophagus Muscularis changes from skeletal (superiorly) to smooth muscle (inferiorly) Digestive Processes in the Mouth Food is ingested Mechanical digestion begins (chewing) Propulsion is initiated by swallowing Salivary amylase begins chemical breakdown of starch The pharynx and esophagus serve as conduits to pass food from the mouth to the stomach Deglutition (Swallowing) Coordinated activity of the tongue, soft palate, pharynx, esophagus, and 22 separate muscle groups Buccal phase – bolus is forced into the oropharynx Deglutition (Swallowing) Pharyngeal-esophageal phase – controlled by the medulla and lower pons All routes except into the digestive tract are sealed off Peristalsis moves food through the pharynx to the esophagus Stomach Chemical breakdown of proteins begins and food is converted to chyme Cardiac region – surrounds the cardiac orifice Fundus – dome-shaped region beneath the diaphragm Body – midportion of the stomach Pyloric region – made up of the antrum and canal which terminates at the pylorus The pylorus is continuous with the duodenum through the pyloric sphincter Stomach Greater curvature – entire extent of the convex lateral surface Lesser curvature – concave medial surface Lesser omentum – runs from the liver to the lesser curvature Greater omentum – drapes inferiorly from the greater curvature to the small intestine Stomach Nerve supply – sympathetic and parasympathetic fibers of the autonomic nervous system Blood supply – celiac trunk, and corresponding veins (part of the hepatic portal system) Microscopic Anatomy of the Stomach Muscularis – has an additional oblique layer that: Allows the stomach to churn, mix, and pummel food physically Breaks down food into smaller fragments Microscopic Anatomy of the Stomach Epithelial lining is composed of: Goblet cells that produce a coat of alkaline mucus The mucous surface layer traps a bicarbonate-rich fluid beneath it Gastric pits contain gastric glands that secrete gastric juice, mucus, and gastrin Glands of the Stomach Fundus and Body Gastric glands of the fundus and body have a variety of secretory cells Mucous neck cells – secrete acid mucus Parietal cells – secrete HCl and intrinsic factor Glands of the Stomach Fundus and Body Chief cells – produce pepsinogen Pepsinogen is activated to pepsin by: HCl in the stomach Pepsin itself via a positive feedback mechanism Enteroendocrine cells – secrete gastrin, histamine, endorphins, serotonin, cholecystokinin (CCK), and somatostatin into the lamina propria Stomach Lining The stomach is exposed to the harshest conditions in the digestive tract To keep from digesting itself, the stomach has a mucosal barrier with: A thick coat of bicarbonate-rich mucus on the stomach wall Epithelial cells that are joined by tight junctions Gastric glands that have cells impermeable to HCl Damaged epithelial cells are quickly replaced Digestion in the Stomach The stomach: Holds ingested food Degrades this food both physically and chemically Delivers chyme to the small intestine Enzymatically digests proteins with pepsin Secretes intrinsic factor required for absorption of vitamin B12 Regulation of Gastric Secretion Neural and hormonal mechanisms regulate the release of gastric juice Stimulatory and inhibitory events occur in three phases Cephalic (reflex) phase: prior to food entry Gastric phase: once food enters the stomach Intestinal phase: as partially digested food enters the duodenum Cephalic Phase Excitatory events include: Sight or thought of food Stimulation of taste or smell receptors Inhibitory events include: Loss of appetite or depression Decrease in stimulation of the parasympathetic division Gastric Phase Excitatory events include: Stomach distension Activation of stretch receptors (neural activation) Activation of chemoreceptors by peptides, caffeine, and rising pH Release of gastrin to the blood Gastric Phase Inhibitory events include: A pH lower than 2 Emotional upset that overrides the parasympathetic division Intestinal Phase Excitatory phase – low pH; partially digested food enters the duodenum and encourages gastric gland activity Inhibitory phase – distension of duodenum, presence of fatty, acidic, or hypertonic chyme, and/or irritants in the duodenum Initiates inhibition of local reflexes and vagal nuclei Closes the pyloric sphincter Releases enterogastrones that inhibit gastric secretion Regulation and Mechanism of HCl Secretion HCl secretion is stimulated by ACh, histamine, and gastrin through second-messenger systems Antihistamines block H2 receptors and decrease HCl release Response of the Stomach to Filling Stomach pressure remains constant until about 1L of food is ingested Relative unchanging pressure results from reflex-mediated relaxation and plasticity Response of the Stomach to Filling Reflex-mediated events include: Receptive relaxation – as food travels in the esophagus, stomach muscles relax Adaptive relaxation – the stomach dilates in response to gastric filling Plasticity – intrinsic ability of smooth muscle to exhibit the stress-relaxation response Gastric Contractile Activity Peristaltic waves move toward the pylorus at the rate of 3 per minute This basic electrical rhythm (BER) is initiated by pacemaker cells (cells of Cajal) Gastric Contractile Activity Most vigorous peristalsis and mixing occurs near the pylorus Chyme is either: Delivered in small amounts to the duodenum or Forced backward into the stomach for further mixing Regulation of Gastric Emptying Gastric emptying is regulated by: The neural enterogastric reflex Hormonal (enterogastrone) mechanisms These mechanisms inhibit gastric secretion and duodenal filling Regulation of Gastric Emptying Carbohydrate-rich chyme quickly moves through the duodenum Fat-laden chyme is digested more slowly causing food to remain in the stomach longer Small Intestine: Gross Anatomy Runs from pyloric sphincter to the ileocecal valve Has three subdivisions: duodenum, jejunum, and ileum Small Intestine: Gross Anatomy The bile duct and main pancreatic duct: Join the duodenum at the hepatopancreatic ampulla Are controlled by the sphincter of Oddi The jejunum extends from the duodenum to the ileum The ileum joins the large intestine at the ileocecal valve Small Intestine: Microscopic Anatomy Structural modifications of the small intestine wall increase surface area Plicae circulares: deep circular folds of the mucosa and submucosa Villi – fingerlike extensions of the mucosa Microvilli – tiny projections of absorptive mucosal cells’ plasma membranes Small Intestine: Histology of the Wall The epithelium of the mucosa is made up of: Absorptive cells and goblet cells Enteroendocrine cells Interspersed T cells called intraepithelial lymphocytes (IELs) IELs release cytokines Small Intestine: Histology of the Wall Cells of intestinal crypts secrete intestinal juice Peyer’s patches are found in the submucosa Brunner’s glands in the duodenum secrete alkaline mucus Intestinal Juice Secreted by intestinal glands in response to distension or irritation of the mucosa Slightly alkaline and isotonic with blood plasma Largely water, enzyme-poor, but contains mucus Liver The largest gland in the body Superficially has four lobes – right, left, caudate, and quadrate The falciform ligament: Separates the right and left lobes anteriorly Suspends the liver from the diaphragm and anterior abdominal wall Liver The ligamentum teres: Is a remnant of the fetal umbilical vein Runs along the free edge of the falciform ligament Liver: Associated Structures The lesser omentum anchors the liver to the stomach The hepatic blood vessels enter the liver at the porta hepatis The gallbladder rests in a recess on the inferior surface of the right lobe Liver: Associated Structures Bile leaves the liver via: Bile ducts, which fuse into the common hepatic duct The common hepatic duct, which fuses with the cystic duct These two ducts form the bile duct Liver: Microscopic Anatomy Hexagonal-shaped liver lobules are the structural and functional units of the liver Composed of hepatocyte (liver cell) plates radiating outward from a central vein Portal triads are found at each of the six corners of each liver lobule Figure 23.24c Liver: Microscopic Anatomy Portal triads consist of a bile duct and Hepatic artery – supplies oxygen-rich blood to the liver Hepatic portal vein – carries venous blood with nutrients from digestive viscera Figure 23.24d Liver: Microscopic Anatomy Liver sinusoids – enlarged, leaky capillaries located between hepatic plates Kupffer cells – hepatic macrophages found in liver sinusoids Liver: Microscopic Anatomy Hepatocytes’ functions include: Production of bile Processing bloodborne nutrients Storage of fat-soluble vitamins Detoxification Secreted bile flows between hepatocytes toward the bile ducts in the portal triads Composition of Bile A yellow-green, alkaline solution containing bile salts, bile pigments, cholesterol, neutral fats, phospholipids, and electrolytes Bile salts are cholesterol derivatives that: Emulsify fat Facilitate fat and cholesterol absorption Help solubilize cholesterol Enterohepatic circulation recycles bile salts The chief bile pigment is bilirubin, a waste product of heme The Gallbladder Thin-walled, green muscular sac on the ventral surface of the liver Stores and concentrates bile by absorbing its water and ions Releases bile via the cystic duct, which flows into the bile duct Regulation of Bile Release Acidic, fatty chyme causes the duodenum to release: Cholecystokinin (CCK) and secretin into the bloodstream Bile salts and secretin transported in blood stimulate the liver to produce bile Vagal stimulation causes weak contractions of the gallbladder Regulation of Bile Release Cholecystokinin causes: The gallbladder to contract The hepatopancreatic sphincter to relax As a result, bile enters the duodenum