Urinary I. Introduction and anatomical features
advertisement

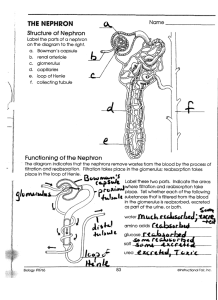
Urinary I. Introduction and anatomical features A. Introduction: The kidneys receive blood from the renal artery. The renal artery branches into a series of capillary beds. Those capillary beds are surrounded by a cup that leads to a tube. Here, some plasma is squeezed out of the capillaries; it is captured by the cup and then sent into the tube. Lining the tube are cells, one single layer of cells. These cells examine the subset of plasma and decide what is waste and what is valuable. Anything that is NOT waste will be plucked out of the tube and returned to the blood by these cells. Anything that IS waste stays in the tube. The kidneys contain millions of these “cup and tube” devices. All of the tubes lead to the collecting area of the kidney, which leads to the ureter. The “cup and tube” devices are called nephrons. The “cup” part of the nephron is called Bowman’s Capsule. Terms: filtration, reabsorption, secretion B. Blood supply to the kidneys- the renal artery enters at the hilus. It branches into the interlobar arteries that travel through the columns, they branch further, leading to the afferent arterioles that enter the Bowman’s capsule of each nephron. The afferent arterioles branch into a capillary bed called a glomerulus within the Bowman's capsule. The glomerulus merges back into the efferent arteriole which leaves Bowman’s capsule. The efferent arteriole branches again into the peritubular capillaries and vasa recta (also capillaries) which wrap around the tubules of the nephron. The peritubular capillaries merge into venules, which merge into the interlobar veins. The interlobar veins merge into the renal vein, which leaves the kidney at the hilus. C. Nephrons- this is where fluid (a subset of plasma) leaves the blood, and urine is produced by returning nutrients to blood, and keeping waste products out of the blood. 1. The "entrance" to a nephron- where blood fluid enters: the renal corpuscle a. Blood plasma enters each nephron in a little capsule called Bowman's capsule. It contains a double layer of epithelium. The inner (visceral) layer lines the glomerulus (capillary bed). The outer (parietal) layer forms the outer wall, and is continuous with a tubule that will carry blood fluids away. This is similar to the serous membranes we've discussed, in that it resembles a balloon with a fist pushed into it (in this case, the glomerulus is the "fist"), and there is a fluid-filled space between the layers. This space is called the capsular space. b. The glomerulus is a ball of capillaries within Bowman's capsule. The afferent arteriole brings blood into the glomerulus, and the efferent arteriole carries blood away from it. The glomerular capillaries are fenestrated, and they are surrounded by a basement membrane. c. The filtration membrane- blood fluid is forced across the fenestrated capillaries, the basement membrane, and between the filtration slits into the capsular space. These three layers, collectively, are called the filtration membrane. Each layer is more restrictive in terms of the size of particles it will let cross. For example, the fenestrated capillaries allow most proteins to cross, but the filtration slits allow no proteins to cross. The filtration membrane allows most plasma solutes, but not proteins, to pass into the capsular space. Proteins are among the largest molecules in the plasma. Red blood cells are way too huge to cross the filtration membrane. The subset of plasma that has entered the nephron is now called filtrate. 2. The tubules- receive filtrate from the renal corpuscle. Peritubular and vasa recta capillaries wrap around the tubules. As filtrate travels through the tubules, substances we don't want to get rid of (ex., glucose and amino acids) are reabsorbed (returned to the blood). In addition, some undesired substances in the blood are moved into the tubules for excretion (secreted). Each section has a different function, which is reflected in their anatomy and permeability to specific substances. Keep in mind that when a cell is permeable to a substance, like water or Na+, that means the cell has channels that specifically let that substance through. The only substances that don't need channels are relatively small and relatively uncharged. a. The Proximal Convoluted Tubule- receives filtrate from the renal corpuscle. Simple cuboidal with microvilli. Most reabsorption and secretion of solutes occurs here b. Loop of Henle- filtrate moves from the PCT to the loop of Henle, which includes the descending and ascending limbs, as well as the thin portions (descending and part of the ascending) and thick portion (part of the ascending). For simplification, we will use descdening and thin interchangeably, and ascending and thick interchangeably. i. The descending loop (thin segment)- Simple squamous, no microvilli permeable to water but not to solutes most water reabsorption occurs here ii. The ascending loop (thick segment)Cuboidal with sparce microvilli Not permeable to water but permeable to solutes, especially Na+, ClLots of Na+ reabsorption occurs here c. Distal Convoluted Tubule Simple Cuboidal, sparce microvilli Reabsorption and secretion of some solutes and water, particularly under the influence of hormones. Notably, Na+ and Ca++ reabsorption. d. Collecting ducts Similar to DCT- reabsorption and secretion, influenced by hormones. Two cell populations. One cell type responsible for H2O and Na+ reabsorption and urea secretion. The other cell type responsible for H+ and HCO3- reabsorption or secretion (acid-base balance). 3. Juxtaglomerular Apparatus- Region of the nephron where the DCT gets sandwiched between the afferent and efferent arterioles. In this area, the afferent arteriole and the DCT contain specialized cells that help to maintain filtration pressure. a. Afferent arteriole contains Juxtaglomerular (JG) cells, which secrete renin, and act as mechanoreceptors that monitor stretch (blood pressure). b. DCT contains macula densa, a group of specialized cells adjacent to the JG cells, and act as chemoreceptors and mechanoreceptors that monitor solute concentration and flow rate of the solute. Macula densa cells cause autoregulatory constriction and dilation of the arterioles. II. Kidney Physiology A. Glomerular Filtration 1. Net Filtration Pressure- Hydrostatic pressure of blood entering the glomerulus pushes fluid out of the capillaries and into the Bowman's capsule. Like filtration at other capillaries, it is opposed by other pressures (for instance, osmotic pressure). After all opposing pressures are considered, the average Net Filtration Pressure is about 10 mmHg, and fluid moves out of the glomerulus. This pressure is just perfect to get a good balance of getting enough wastes into the tubules, without pushing too much good stuff out of the blood or damaging the filtration membrane. 2. Glomerular Filtration Rate- The amount of filtrate formed per minute. The GFR is directly proportional to the NFP. Another reason the NFP is carefully maintained is that if the GFR is too high (that is, too much fluid leaves the blood), the tubules will be overloaded and won't have enough time to reabsorb all the desired materials back into the blood. 3. Regulation of Glomerular Filtration- Again, the NFP and GFR must be carefully maintained to make sure that enough wastes are removed from the blood, and enough nutrients are recovered to the blood. This is accomplished through autoregulation, hormonal controls, and sympathetic stimulation. Filtration Pressure is maintained by constricting or dilating the afferent and efferent arterioles. To increase Filtration Pressure, the afferent arteriole can be dilated, the efferent arteriole can be constricted, or both. To decrease Filtration Pressure, the opposite is true. So, if blood pressure rises, for instance, the afferent arteriole could constrict to make sure that the NFP does not rise much above 10 mmHg, and vice versa. a. Autoregulation- this occurs continuously to maintain NFP/GFR, with small adjustments constantly compensating for small changes in blood pressure. Smooth muscle of the arterioles responds automatically, and macula densa cell secretions affect this as well. b. Neuroendocrine Control- these are more concerned with tissue perfusion of the REST of the body, and will cause the kidneys to adjust NFP/GFR to help out; ie, GFR may be increased or reduced to help adjust general body blood pressure. Kidneys will sacrifice GFR, either increase it or decrease it, if needed to help out with the rest of the body. i. The Renin-AngiotensinII mechanism- When pressure coming into the afferent arteriole drops substantially enough, this indicates a drop in general body pressure and JG cells secrete renin. Review renin from the vessels chapter! Angiotensin II causes constriction of both afferent and efferent arterioles, and some blood will be shunted away from kidneys. GFR may be slightly reduced. ii. Atrial Natriuretic Peptide- When pressure in the atria of the heart increases, ANP is released. At the kidneys, ANP causes the afferent arterioles to dilate and the efferent arteriole to constrict. This actually increases NFP/GFR, but by doing so causes increased urine output (and subsequent loss of water thereby lowering blood pressure). iii. Sympathetic influence- a severe sympathetic activation shunts blood away from kidneys by causing both arterioles to constrict. Reduces GFR. Also causes JG cells to secrete renin. B. Tubular Reabsorption and secretion- Again, solutes and water are purposefully reabsorbed or secreted once filtrate gets to the tubules. This is accomplished by channels embedded in the membranes of cells lining the tubules. 1. Mechanisms for moving solutes to or from the blood include: Passive diffusion through channels (water) Facilitated diffusion Active transport Coupled transport: some examples- Na+ and K+ (countertransport), HCO3- and Cl- (countertransport), Na+ and glucose (cotransport) 2. Since reabsorption of water-soluble substances depends on transport through channels, the amount of a substance that can be reabsorbed is dependent on the number of channels available. If the amount of a substance exceeds the number of channels available to reabsorb it, then some will end up in the urine. For example, if you take a multi-vitamin B supplement, you will urinate most of the B6 molecules. That’s because the amount of B6 molecules greatly exceeds the number of channels available for its reabsorption. The number of channels available to reabsorb specific substances is called the transport max. Glucose almost never exceeds its transport max in healthy individuals, so urine tests for glucose can indicate problems. Proteins should not be present in the urine either, but for a different reason; why is that? C. Absorptive capabilities of the tubules- I covered most of this already (see tubule section in anatomy), so I'll just add a little more info on some. 1. PCT- again, highly permeable to most solutes and water. Most solute reabsorption and secretion occurs here, and by the time filtrate reaches the loop of Henle, virtually all glucose and amino acids have been reclaimed to the blood. 2. Loop of Henle- The thin segment is responsible for most water reabsorption, and the thick segment is responsible for Na+ and Cl- reabsorption (which drives the reabsorption of water in the thin segment, as we will see soon). 3. DCT and Collecting ducts- Further reabsorption and secretion occurs here, and these tubules are especially sensitive to hormonal input. Notably, i. Aldosterone- causes tubule cells to build Na+ - K+ countertransport channels. In this case, Na+ is reabsorbed to the blood. Indirectly, aldosterone causes water retention because water "follows" Na+. So, aldosterone causes the reabsorption of Na+ and water, and the secretion of K+. (Promotes Na+ and water conservation) ii. ADH- causes tubule cells to build water channels. This allows more water to be reabsorbed to the blood. (Promotes water conservation) iii. PTH and calcitriol- cause tubule cells to build (or open) Ca++ channels, increasing Ca++ reabsorption. (Promotes Ca2+ conservation) iv. H+ and HCO3- reabsorption and secretion can also be adjusted here, helping to maintain blood pH. No hormone needed here; we’ll revisit with electrolytes. 4. Back to the Loop of Henle: the Counter Current Mechanism, how water is reabsorbed. The water channels in cells are always open. So, cells cannot actively "pump" water in the desired direction. Therefore, they use the principle of osmosis to direct water movement. Remember that osmosis predicts that water will move from a hypotonic solution to a hypertonic solution. So, if you are a cell, and you "want" water to move in a particular direction, you can establish a gradient of solute concentration and water will follow that gradient. That's exactly what cells of the thick segment of the loop of Henle do. We'll start there. The thick segment of the loop of Henle is completely impermeable to water. In this section, cells pump Na+ and Cl- into the interstitium (or peritubular space). Na+ and Clbuild up in the peritubular space, which becomes quite concentrate. In fact, it becomes hypertonic to the filtrate in the thin segment. Now we will back up a bit, and look at filtrate entering the thin segment. The thin segment is right next to the thick segment, and they share peritubular space. Remember that the thin segment is highly permeable to water. Fluid entering the thin segment is suddenly thrown into highly hypertonic surroundings. Water gets sucked right out of the thin segment, moving passively by osmosis. At this point, we've gotten water to leave the tubules and enter the interstitium. But we still need to get it back to the blood. A network of capillaries wraps around the loop, the vasa recta. Blood in these capillaries moves in the opposite direction as filtrate in the loop. Now we need to go back to the thick segment of the ascending loop. Here, blood is traveling down the peritubular capillaries. Cells of the thick segment are busy pumping out Na+ and Cl-, and blood entering this area enters a very concentrate environment. Instead of letting water go, the peritubular capillaries instead let Na+ and Cl- enter. So, as blood enters this concentrate environment, Na+ and Cl- rush into the blood, and it becomes very concentrate. As it travels down the loop, blood absorbs more and more Na+ and Cl-. Then, the capillaries wrap around the base of the loop and blood travels up, past the descending, thin segment. Here, the blood is so concentrate that it is in fact hypertonic to the peritubular space (interstitium). At any given point along the descending loop, blood in the adjacent peritubular capillaries is hypertonic to the peritubular space. And recall, the peritubular space is hypertonic to the filtrate. So, along the descending loop water leaves the filtrate by osmosis. Since the blood is even MORE hypertonic, water just keeps on going and moves right into the blood, which is carried completely away. So, along the descending, thin segment of the loop of Henle, at any given point the peritubular space is hypertonic to the filtrate, and blood in the adjacent peritubular capillaries is hypertonic to the peritubular space. Water moves by osmosis straight from the filtrate into the blood. Voila, water is reabsorbed. Now, take a few moments to draw this process out. Start with the thick segment pumping out NaCl. Draw the capillaries running next to the loop, and indicate with arrows the direction of filtrate and blood movement. Show blood moving to the descending loop. Indicate with arrows water moving out of the filtrate and entering the blood by osmosis. Go ahead, it'll be fun!