ANS I. Introduction/Overview of the ANS >A. Comparisons with the SNS
advertisement

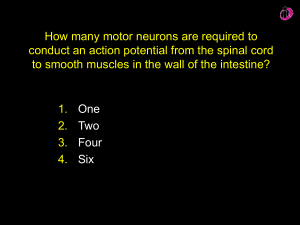
ANS I. Introduction/Overview of the ANS >A. Comparisons with the SNS >>1. ANS effectors are smooth muscle, cardiac muscle, and glands (what does the SNS target?) >>2. Autonomic motor neurons synapse in ganglia (do SNS neurons?) >>>the Pre-ganglionic neuron originates in the brain or spinal cord >>>the Ganglionic neuron has its cell body in a ganglion, and there it synapses with the axon terminals of the Pre-ganglionic neuron. The ganglionic neuron sends its Post-ganglionic fiber, or axon, to its effector (what are the effectors of the ANS?) >>3. Preganglionic axons are type-B fibers, postganglionic axons are type-C fibers (what does this mean? Do ANS axons conduct faster or slower than SNS fibers?) >>4. SNS motor neurons all release Ach on effectors, and it's always excitatory. ANS motor neurons, on the other hand, may release Ach (parasympathetic) orNE (sympathetic) on their effectors. Depending on the receptor type and effector, Ach and NE can be either excitatory or inhibitory. >B. Overview of the divisions >>1. Parasympathetic- the "resting and digesting" division. When parasympathetic activity dominates, >>>heart rate and blood pressure decline >>>GI tract motility increases, and excretory activity increases (defecation and urination) >>>respiratory rate and volume decrease (breaths are shallow and slow) >>>energy in the form of glycogen and triglycerides is stored >>2. Sympathetic- the "stress, exercise, and emergency" division. When sympathetic activity dominates, >>>heart rate, blood pressure, and muscle tone increase >>>GI tract motility and excretory activity decrease >>>respiratory rate and volume increase (breaths are deep and fast) >>>alertness increases >>>energy stores are mobilized, so glycogen is broken down to release glucose to the blood, and triglycerides are released to the blood from adipose. II. Parasympathetic division >A. Preganglionic fibers travel in cranial nerves and sacral spinal nerves (trivia: 90% of all parasympathetic preganglionic fibers travel through the vagus nerve & its branches) >B. The preganglionic neuron synapses with the ganlionic neuron/s in a ganlion near the effector or in the effector. Preganglionic axons release Ach onto ganglionic neuron, whose postganglionic axons release Ach onto its effector. >C. Preganglionic fibers are long, postganglionic fibers are short. >D. Functions -increase GI tract motility -relax GI tract sphincters -increase digestive gland activity -increase excretory activity -conserve energy (reduce heart rate, respiration rate, store fats, etc) -constrict pupils -prepare for sexual activity III. Sympathetic division >A. The effectors innervated by the parasympathetic division are also innervated by the sympathetic division, and the two divisions generally have opposing effects. However, the sympathetic division serves some effectors that ARE NOT served by the parasympathetic. Effectors that only receive sympathetic innervation include: smooth muscle lining blood vessels, the arrector pili muscles, sweat glands, and the adrenal glands. So, for instance, the degree of constriction of blood vessels is dependent on the sympathetic division only. >B. Synapses and ganglia >>1. Preganglionic fibers travel through the T1-L2 spinal nerves. They release Ach onto ganglionic neurons in ganglia (see below). The postganglionic axons release NE (most) or Ach (some) onto their effectors. Preganglionic fibers are generally short, postganglionic fibers are generally long. >>2. They synapse with their ganglionic neurons in one of 3 places: >>>a. Sympathetic chain ganglia- paired, near the spinal cord on either side >>>b. Collateral ganglia- unpaired, located anterior to the vertebral column >>>c. Adrenal medulla- the center of the adrenal glands. The adrenal glands are located on top of the kidneys. In the adrenal medulla, specialized neurons produce and release NE and Epinephrine into the blood. This is unusual because this means that NE can serve both as a neurotransmitter and as a hormone. Hormones are chemicals that are released into the blood and can have widespread effects on many different types of cells throughout the body. NE and E have similar effects. >>3. The telodendria, or axon terminal branches, of postganglionic fibers are specialized to release Nt all along the branches, rather than just at the synaptic terminal. Remember that the axon is a long fiber that carries an action potential. The end of the axon contains small branches called telodendria. Normally, the ends of the telodendria form swollen knobs that release Nt in response to an action potential. In the post-ganglionic fibers of the sympathetic division of the ANS, the swollen areas of the telodendria are not restricted to the very ends. Instead, several areas along the telodendria swell and synapse with effectors. These swollen areas release Nt in response to action potentials arriving from the axon, just like synaptic knobs. They are called varicosities. Varicosities allow one neuron to wrap its telodendria around its effector and release Nt all over it at once. *So, a ganglion is a swollen area of a whole nerve, which contains the axon terminals and cell bodies of MANY neurons. A telodenrion is a type of axon terminal which occurs on ONE neuron. >C. Functions -decrease GI activity and all related digestive functions -shunt blood to skeletal muscle, brain and heart (constrict most vessels, dilate those going to muscle, brain and heart): increase blood pressure, alertness, and readiness for exercise -mobilize energy stores (fat and glycogen breakdown) -increase heart rate and respiratory rate; dilate airways -dilate pupils -complete sexual activity IV. Neurotransmitters and receptors of the ANS >A. Fiber types based on the Nt they release- right now we're talking about what goes on at axon terminals (release of Nt from the presynaptic neuron) >>1. Cholinergic- release Ach, which acts directly. Found on: >>>All preganglionic fibers of the ANS, so the preganglionic fibers of both divisions release Ach >>>All parasympathetic postganglionic fibers, and a few sympathetic postganglionic fibers (ex, those serving sweat glands) >>2. Adrenergic- release NE, which acts indirectly. Found on: >>>Most sympathetic postganglionic fibers >>3. (This will be for extra credit only) Nitroxidergic- release NO (nitric oxide). NO is a powerful vasodilator (causes blood vessels to dilate). Found on: >>>Some sympathetic postganglionic fibers >B. Receptor types based on what Nt they bind to and how they respondright now we're talking about what goes on at cell bodies and dendrites of a postsynaptic neuron or effector (binding of Nt released from the presynaptic neuron) See table 14.3, pg. 513 >>1. Receptors that bind to Ach-cholinergic. There are two types of cholinergic receptors: >>>a. Nicotinic- When Ach binds to nicotinic receptors, it causes a direct EPSP. Nicotinic receptors are found on (in general, neuron cell bodies/dendrites): >>>>all ganglionic neuron cell bodies and dendrites >>>>neurons of the adrenal medulla >>>>(FYI: also motor end plates of skeletal muscle) >>>b. Muscarinic- When Ach binds to muscarinic receptors, it can be either excitatory or inhibitory. Often indirect. Muscarinic receptors are found on (in general, effectors): >>>>All parasympathetic effectors- again, excitatory on most, inhibitory on cardiac muscle. >>>>Some sympathetic effectors- excitatory or inhibitory. For example, - Ach binding muscarinic receptors on sweat glands is excitatory; - Ach binding muscarinic receptors on blood vessels is inhibitory; blood vessels with muscarinic receptors are found serving skeletal muscle and the brain. >>2. Receptors that bind to NE (or E, from the blood)- adrenergic. NE and E cause indirect effects on target cells. There are two broad categories of adrenergic receptors, alpha and beta. Within each of these categories are subcategories. >>>a. Alpha-receptors- NE binding to alpha receptors can be excitatory or inhibitory, depending on the cell type. For example, NE binding to alpha receptors on most smooth muscle lining blood vessels causes EPSPs, or blood vessel constriction. There are 2 subcategories; here are some examples of where they are found and how they affect their cells when NE binds: -alpha 1 receptors: >on most blood vessels, cause vasoconstriction (EPSP) -alpha 2 receptors: >on pancreas and other secretory glands, cause inhibition >>>b. Beta-receptors- again, excitatory or inhibitory. For example, NE binding to beta receptors on smooth muscle lining blood vessels causes IPSPs, or blood vessel dilation. NE binding to beta-receptors on target cells also increases general metabolic activity. For example, adipose cells contain beta-receptors, and they release triglycerides in response to binding of NE. There are 3 subcategories; here are some examples of where they are found and how they affect their cells when NE binds: -beta 1 receptors: >on cardiac muscle, cause increased heart rate (EPSP) >on kidneys, cause renin release -beta 2 receptors: >on blood vessels serving the heart, cause vasodilation (IPSP) >on digestive organs, decrease muscular activity (IPSP) -beta 3 receptors: >on adipose tissue, cause lipolysis V. ANS tone > Autonomic neurons are always active to some extent. The "resting" condition of ANS effectors is determined by the degree of influence of each of the divisions. For instance, heart rate is determined by the amount of NE (excitatory) from sympathetic fibers versus the amount of Ach (inhibitory) from parasympathetic fibers. Cardiac muscle is always receiving some of both. When heart rate increases, the amount of NE increases, and the amount of Ach decreases. Another example: remember that blood vessel diameter (degree of constriction) is determined by the sympathetic division. Smooth muscle lining vessels is always receiving some NE, so the smooth muscle lining vessels is always tone. To dilate or constrict a vessel, the sympathetic division releases more or less NE onto the smooth muscle. Depending on where the vessel is located in the body, NE can be excitatory (cause constriction) or inhibitory (cause dilatation). This is, of course, based on the receptor types. VI. Visceral Reflexes- like somatic reflexes, these are simple reflex arcs between sensory and motor neurons that bypass the brain. They can involve an interneuron between sensory and motor neurons, or they can be direct connections. Synapses can occur in the gray matter of the spinal cord, or can occur in ganglia. When synapses occur in ganglia, the reflex bypasses the CNS; this is called a short reflex, and it is unique to the ANS. An example of a long reflex controlled by the ANS is the constriction of pupils in response to bright light. Short reflexes occur in the enteric nervous system: an extensive network of visceral neurons in the GI tract that communicate via reflex arcs, and function to some extent without input from the CNS.