Reading Guide Antibiotics (CH20)
advertisement

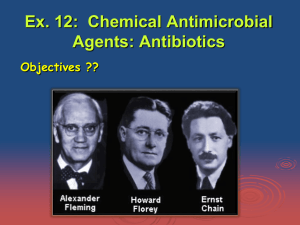
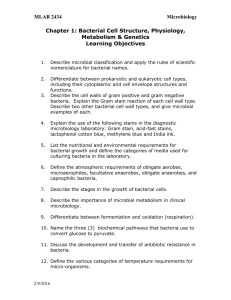
Reading Guide Antibiotics (CH20) This chapter focuses on some key ideas about antimicrobial drugs. We will look at some of the history of antibiotics, discuss the general features of antimicrobial drugs, and then cover some specific classes of drugs and talk about their mechanisms of action. Let’s get started! The history of antibiotics begins much earlier than Alexander Fleming and his moldy plates of S. aureus. The idea of chemicals that can target specific types of cells first came from Paul Erlich. While staining tissues to look at the different cellular structures he noticed that some dyes stain certain parts of cells and not others. This gave him the idea to search for a chemical that would target bacterial cells and not impact human cells. His search for a “magic bullet” to treat the bacterial disease syphilis ended when he identified an arsenic chemical, arsphenamine, to be an effective treatment. Patients weren’t too crazy about being treated with an arsenic compound so he changed the name to “salvarsan”, a name from the merging of “salvation with arsenic”. This was the first documented chemical treatment for bacterial infections, and also considered the first type of chemotherapy. In 1928, Alexander Fleming discovered the mold Penicillium growing on an agar plate with Staphylococcus aureus. What he noticed about the plate was that the mold appeared to be producing something that caused the S. aureus colonies to lyse. He named the agent capable of killing the bacterial cells penicillin but was unsuccessful in isolating the substance. In 1940, Chain and Florey were the first to successfully purify penicillin and test it on a police officer with a S. aureus infection. The drug appeared to help the police officer but there was not enough drug purified to treat him for more than a few days. Once the antibiotic treatment was stopped, the infection returned was more severe than before treatment. From this experience it was recognized that antibiotic treatment need to be maintained for a longer period of time that a few days and the focus became to purify as much penicillin as possible. Once chemists determined the chemical structure of penicillin it was easy to chemically modify the structure and change the characteristics of the drug. For example, penicillin G is chemically modified to produce the drug ampicillin which has a broad range of activity. Some of the important features of antimicrobial drugs to consider when prescribing a drug are the following: 1. Selective toxicity: Antibiotics are selectively toxic meaning that they target specific parts or processes unique to bacterial cells and not human cell. For example, bacterial cells have cell walls made of peptidoglycan while human cells do not. 2. Antimicrobial action: Antimicrobial drugs are either bacteriostatic (inhibit the growth of organisms) or bacteriocidal (kill the organism). Can you think of some examples of targets for drugs that would be bacteriostatic versus bactericidal? 3. Spectrum of activity: Antibiotics have a targeted range of activity, meaning that they are most effective against certain kinds or groups of bacteria. Antibiotics with a narrow range of activity typically target only a small group or specific kind of organism, for example gram positive bacteria. Drugs with a broad range of activity target a much bigger group of organisms, for example both gram positive and gram negative bacteria. One of the side effects of treating a patient with a broad range antibiotic is that the drugs will also impact the normal microbiota resulting suppression of them. This can often cause an imbalance in the patient leading to other types of infections such as yeast infections or another condition known as antibiotic-associated colitis caused by Clostridium difficile. Let’s talk about some of the mechanisms of action of antimicrobial drugs. Remember that these drugs are selectively toxic since they target specific parts and metabolic pathways unique to bacteria. Look at Fig 21.2 for a summary of these key targets of antibiotics. The first class of drugs I want to review are the ones that target cell wall synthesis. The drugs that are in this category are the penicillins, cephalosporins, and other beta-lactam drugs. They are often referred to as beta-lactam drugs because the structure of the drugs all include a beta-lactam ring. (see Fig. 21.4) These drugs all work by inhibiting the synthesis of peptidoglycan, specifically by interfering with the enzymes (known as penicillin binding proteins or PBPs) which form the peptide bridge (remember the tetrapeptide side chains). These drugs will only impact bacterial cells which are growing and synthesizing new cell walls. Existing bacteria with cell walls will not be impacted by the drugs. So…..would these drugs be considered bactericidal or bacteriostatic? How does a patient get rid of a bacterial infection when treated with this class of drugs if the drug prevents them from growing??? The first beta-lactam discovered was Penicillin G from the mold Penicillium chrysogenum. It was found to be unstable in stomach acid and so could only be administered by injection. Penicillin V, also a natural penicillin, is stable in stomach acid and can be given as oral medication. Both of these are narrow spectrum drugs, targeting only gram positive bacteria. Resistance to these antibiotics is found when bacteria have the enzyme penicillinase which cleaves the beta-lactam ring inactivating the drug. Once the chemical structure of the penicillins was identified, new version of the drugs were made by changing the side chains. Some new versions were resistant to penicillinase and used for treating patients with penicillinase resistant Staphylococcus infections. Some examples are methicillin and dicloxicillin. Other modifications to the chemical structure gave the drugs a broad spectrum of activity, they now worked against both gram positive and gram negative bacteria. Some examples of broad spectrum drugs are ampicillin and amoxicillin. And the last group of drugs I want to mention as chemical modifications of the penicillin structure are the drugs which included a beta-lactamase inhibitor into the composition. Essentially two drugs in one, the antibiotic and an enzyme inhibitor, both working well on a broad range of organisms and especially with strains that produce a beta-lactamase. (Beta-lactamases are enzymes that break apart the betalactam ring of beta-lactam drugs. These differ from penicillinases in that penicillinases only are effective at targeting the beta-lactam ring of the penicillins). The best example of this “combo” drug is the drug Augmentin. The cephalosporins also target cell wall synthesis and have a beta-lactam ring. They tend to be more resistant to beta-lactamases, don’t work as well against gram positive bacteria. This class of drugs also has experienced changes to the chemical structure giving rise to categories of first, second, third generation drugs. Vancomycin is the last one in this group of drugs that target the cell wall structure. It inhibits cell wall synthesis at a different place, by binding to the terminal amino acids of the side chains and preventing the formation of peptidoglycan. It is used to treat patients who have gram positive infections with beta-lactamase organisms. It is not absorbed by the stomach so must be administered by IV. Watch for discussion of evolved resistance of MRSA (methicillin-resistance S. aureus) to be VRSA (Vancomycin-resistant S. aureus). The other big target of antimicrobial drugs are the ones that inhibit protein synthesis. Think of the places where these drugs could target to inhibit the process of making proteins. Since the ribosomes are key to the process of making proteins, they tend to be the target for binding sites of these drugs. …and remember that the sizes of the ribosomes are different in bacteria compared to human ribosomes. Look over the target for the drugs in the classes aminoglycosides, tetracyclines, macrolides, and oxazolidinones. As you review the characteristics of the drugs in these categories, think of whether or not the drug is bacteriostatic or bactericidal. There are some drugs which inhibit nucleic acid synthesis. They are the fluoroquinolones and rifamycins. The fluoroquinolones inhibit the enzymes necessary for the coiling of the DNA, such as DNA gyrase. Examples of these drugs are ciprofloxacin and moxifloxacin. The rifamycins block RNA polymerase from initiating transcription. The drug Rifampin is the most common used one in this group, often used as one of the primary drug treatments for patients with TB. The sulfonamides and trimethoprim are groups of drugs that inhibit the ability of the cell to make folic acid from para-aminobenzoic acid. The sulfonamides work as competitive inhibitors, inhibiting an enzyme in the pathway. Trimethoprims also inhibit an enzyme in the same pathway and are often used in combination with the sulfonamides. These drugs are used to treat patients with urinary tract infections caused by E. coli. How do you know if a drug will work as a treatment for a patient? One way to determine this is to do a Kirby-Bauer disc diffusion test, just like we did in lab!