The Respiratory System I: Anatomy
advertisement
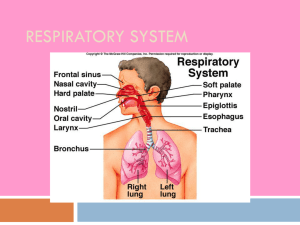
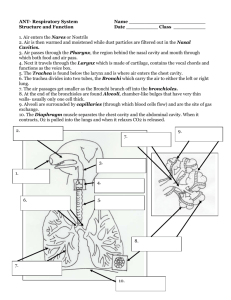
The Respiratory System I: Anatomy Functions of the Respiratory System The Nasal Cavity and Sinuses Pharynx, Larynx, & Trachea Respiratory Mucosa Lungs: Lobes, Bronchioles, & Alveoli Mechanics of Breathing • Pressure Relationships • Inspiration and Expiration • Lung Compliance Respiration Pulmonary ventilation (breathing): movement of air into and out of the lungs External respiration: O2 and CO2 exchange between the lungs and the blood Respiratory system Transport: O2 and CO2 in the blood Internal respiration: O2 and CO2 exchange between systemic blood vessels and tissues Circulatory system Organs of the Respiratory system Key Functions Pulmonary ventilation External respiration Respiratory gas transport Internal respiration External intercostals Functional Anatomy Respiratory zone: site of gas exchange • Microscopic structures: respiratory bronchioles, alveolar ducts, and alveoli Conducting zone: conduits to gas exchange sites • Includes all other respiratory structures Respiratory muscles: diaphragm and other muscles that promote ventilation The Respiratory System I: Anatomy Functions of the Respiratory System The Nasal Cavity and Sinuses Pharynx, Larynx, & Trachea Respiratory Mucosa Lungs: Lobes, Bronchioles, & Alveoli Mechanics of Breathing • Pressure Relationships • Inspiration and Expiration • Lung Compliance Upper Respiratory Tract Cribriform plate of ethmoid bone Sphenoid sinus Posterior nasal aperture Nasopharynx Pharyngeal tonsil Opening of pharyngotympanic tube Uvula Frontal sinus Nasal cavity Nasal conchae (superior, middle and inferior) Nasal meatuses (superior, middle, and inferior) Nasal vestibule Nostril Oropharynx Palatine tonsil Isthmus of the fauces Hard palate Soft palate Tongue Lingual tonsil Laryngopharynx Esophagus Trachea (c) Illustration Larynx Epiglottis Vestibular fold Thyroid cartilage Vocal fold Cricoid cartilage Thyroid gland Hyoid bone Figure 22.3c Anatomy of the Nasal Cavity Function of respiratory mucosa in nasal cavity • Moistens and heats air so lungs are not dehydrated nor cool the body’s core; cools it on way out • Traps incoming foreign particles Function of conchae (projections from lateral walls) • Increase surface area • Increases air turbulence within the nasal cavity Nasal cavity is separated from the oral cavity by the palate • Anterior hard palate (bone) and posterior soft palate (muscle) Function of the sinuses • Lighten the skull • Act as resonance chambers for speech • Produce mucus that drains into the nasal cavity • Cavities within bones surrounding the nasal cavity: frontal, sphenoid, ethmoid, maxillary bones hard palate soft palate The Respiratory System I: Anatomy Functions of the Respiratory System The Nasal Cavity and Sinuses Pharynx, Larynx, & Trachea Respiratory Mucosa Lungs: Lobes, Bronchioles, & Alveoli Mechanics of Breathing • Pressure Relationships • Inspiration and Expiration • Lung Compliance Pharynx (Throat) Muscular passage from nasal cavity to larynx Three regions of the pharynx • Nasopharynx – superior region behind nasal cavity- pseudostratified col. epith. • Oropharynx – middle region behind mouth, stratified squamous epithelium • Laryngopharynx – inferior region attached to larynx The oropharynx and laryngopharynx are common passageways for air and food Auditory tubes enter the nasopharynx Tonsils of the pharynx • Pharyngeal tonsil (adenoids) in the nasopharynx • Palatine tonsils in the oropharynx • Lingual tonsils at the base of the tongue Larynx (Voice Box) Function: Routes air and food into proper channels Plays a role in speech Made of eight rigid hyaline cartilages and a spoon-shaped flap of elastic cartilage (epiglottis) Structures of the Larynx • • Thyroid cartilage o Largest hyaline cartilage o Protrudes anteriorly (Adam’s apple) Epiglottis o Superior opening of the larynx o Routes food to the esophagus and air toward the trachea o Vocal cords (vocal folds) o Glottis – opening between vocal cords Respiratory Mucosa or Epithelium Nasal Cavity and Pharynx • Pseudostratified ciliated columnar epithelium • Superficial to the lamina propria of connective tissue • Mucous secretions from goblet cells contain lysozyme and defensins • Cilia in the nasal cavity move contaminated mucus posteriorly to throat; tracheal cilia move mucus upward into pharynx • Bronchi have cartilaginous reinforcement Trachea & Bronchi • Pseudostratified ciliated columnar epithelium • Cartilaginous support of hyaline cartilage deep to the lamina propria Bronchioles • Simple cuboidal epithelium and cartilage Alveoli • Simple squamous epithelium Trachea (Windpipe) Connects larynx with bronchi Lined with ciliated mucosa • Beat continuously in the opposite direction of incoming air • Expel mucus loaded with dust and other debris away from lungs Walls are reinforced with C-shaped hyaline cartilage Mucosa • Pseudostratified ciliated columnar epithelium • Lamina propria (connective tissue) Submucosa Seromucous gland in submucosa Hyaline cartilage (b) Photomicrograph of the tracheal wall (320x) Figure 22.6b The Respiratory System I: Anatomy Functions of the Respiratory System The Nasal Cavity and Sinuses Pharynx, Larynx, & Trachea Respiratory Mucosa Lungs: Lobes, Bronchioles, & Alveoli Mechanics of Breathing • Pressure Relationships • Inspiration and Expiration • Lung Compliance Lungs Occupy most of the thoracic cavity • Apex is near the clavicle (superior portion) o Base rests on the diaphragm (inferior portion) • Each lung is divided into lobes by fissures o Left lung – two lobes o Right lung – three lobes Diaphragm Lungs: Primary Bronchi Formed by division of the trachea Enters the lung at the hilus (medial depression) Right bronchus is wider, shorter, and straighter than left • More likely to get infections in right lung than left Bronchi subdivide into smaller and smaller branches (with rings) Lungs: Linings (Pleura) • Thin, doublelayered serosa • Pleural fluid provides lubrication and surface tension Respiratory Tree Divisions Primary bronchi Secondary bronchi Tertiary bronchi Bronchioles Bronchioles Bronchioles end in terminal bronchioli • All but the smallest branches have reinforcing cartilage • Lined with simple cuboidal epithelium Terminal bronchioles end in alveoli Capillaries Surround Alveoli to Pick Up O2 and Deliver CO2 Terminal bronchiole Respiratory bronchiole Smooth muscle Elastic fibers Alveolus Capillaries Figure 22.9a Respiratory bronchiole Alveolar duct Alveolar pores Alveoli (b) Alveolar sac Figure 22.8b Alveolar Structure and Cellular Composition (The Respiratory Membrane) Red blood cell Nucleus of type I (squamous epithelial) cell Alveolar pore Capillary O2 Capillary CO2 Alveolus Alveolus Type I cell of alveolar wall Macrophage Endothelial cell nucleus Respiratory membrane Red blood cell Alveoli (gas-filled in capillary Type II (surfactantair spaces) secreting) cell Type II cells also secrete antimicrobial proteins Alveolar epithelium Fused basement membranes of the alveolar epithelium and the capillary endothelium Capillary endothelium External respiration: O2 and CO2 flow easily down their concentration gradients, into and out of alveoli across thin, simple squamous epithelium Figure 22.9c The Respiratory System I: Anatomy Functions of the Respiratory System The Nasal Cavity and Sinuses Pharynx, Larynx, & Trachea Respiratory Mucosa Lungs: Lobes, Bronchioles, & Alveoli Mechanics of Breathing • Pressure Relationships • Inspiration and Expiration • Lung Compliance Pressure Relationships in the Thoracic Cavity Respiratory pressures are described relative to Patm • A negative respiratory pressure is less than Patm • A positive respiratory pressure is greater than Patm • Zero respiratory pressure = Patm = 760 Hg at sea level Intrapulmonary and Intrapleural Pressures Intrapulmonary (intra-alveolar) pressure (Ppul) • Pressure in the alveoli • Fluctuates with breathing • Always eventually equalizes with Patm Intrapleural pressure (Pip): • Pressure in the pleural cavity that fluctuates with breathing • Expressed as a negative pressure (less than Patm and Ppul), caused by opposing forces: • Elastic lung recoil and alveolar surface tension are forces that promote lung collapse (when Pip = Ppul, lungs collapse) • Elasticity of the chest wall pulls the thorax outward; promotes lung expansion Lungs are Inflated if Transpulmonary Pressure > 0 Atmospheric pressure Parietal pleura Thoracic wall Visceral pleura Pleural cavity Intrapleural pressure 756 mm Hg (–4 mm Hg) Intrapulmonary 756 pressure 760 mm Hg 760 Lung Diaphragm (Relative to Patm= 0 mm Hg) Transpulmonary pressure 760 mm Hg –756 mm Hg = 4 mm Hg Figure 22.12 The Respiratory System I: Anatomy Functions of the Respiratory System The Nasal Cavity and Sinuses Pharynx, Larynx, & Trachea Respiratory Mucosa Lungs: Lobes, Bronchioles, & Alveoli Mechanics of Breathing • Pressure Relationships • Inspiration and Expiration • Lung Compliance Pulmonary Ventilation: Expanding and Contracting the Lungs Subdivided into inspiration and expiration • Mechanical processes that depend on volume changes in the thoracic cavity • Can use Boyle’s Law to understand • P1V1 = P2V2 • Volume changes cause pressure changes • If the volume of the lungs increases, the air pressure within them decreases • Pressure changes cause gases flow to equalize pressure Inspiration: An Active Process Sequence of events Changes in anteriorposterior and superiorinferior dimensions Changes in lateral dimensions (superior view) 1 Inspiratory muscles contract (diaphragm descends; rib cage rises). 2 Thoracic cavity volume increases. Ribs are elevated and sternum flares as external intercostals contract. 3 Lungs are stretched; External intercostals contract. intrapulmonary volume increases. 4 Intrapulmonary pressure drops below Patm (–1 mm Hg). 5 Air (gases) flows into lungs down its pressure gradient until intrapulmonary pressure is 0 (equal to atmospheric pressure). Diaphragm moves inferiorly during contraction. Figure 22.13 (1 of 2) Expiration: Normally a Passive Process Sequence of events Changes in anteriorposterior and superiorinferior dimensions Changes in lateral dimensions (superior view) 1 Inspiratory muscles relax (diaphragm rises; rib cage descends due to recoil of costal cartilages). 2 Thoracic cavity volume Ribs and sternum are depressed as external intercostals relax. decreases. 3 Elastic lungs recoil External intercostals relax. passively; intrapulmonary volume decreases. 4 Intrapulmonary pressure rises above Patm (+1 mm Hg). 5 Air (gases) flows out of lungs down its pressure gradient until intrapulmonary pressure is 0. Diaphragm moves superiorly as it relaxes. Forced expiration is an active process: it uses abdominal and internal intercostal muscles Pressure anim. I online Pressure anim II online Figure 22.13 (2 of 2) Atelectasis Atelectasis (lung collapse) • Plugged bronchioles collapse of alveoli • Wound that admits air into pleural cavity (pneumothorax) The Respiratory System I: Anatomy Functions of the Respiratory System The Nasal Cavity and Sinuses Pharynx, Larynx, & Trachea Respiratory Mucosa Lungs: Lobes, Bronchioles, & Alveoli Mechanics of Breathing • Pressure Relationships • Inspiration and Expiration • Lung Compliance Physical Factors Influencing Pulmonary Ventilation Three factors that must be overcome by inspiratory muscles 1. Airway resistance (friction, usually insignificant if bronchioles wide open, increasing with smaller diameters) 2. Alveolar surface tension (alleviated by Type II alveolar cell surfactant) 3. Lung compliance: the change in lung volume that occurs with a given change in transpulmonary pressure (lung “stretchiness”) Lung Compliance: Ease of Lung Expansion Compliance is normally high (easily inflated) due to • Lung tissue is readily distensible (stretched outwards) • Surfactant alleviates alveolar surface tension Compliance is reduced (as in “stiff lungs”) by • Nonelastic scar tissue (fibrosis) • Reduced production of surfactant (e.g. death of Type II cells) • Decreased flexibility of the thoracic cage Homeostatic imbalances that reduce compliance • Paralysis of intercostal muscles Emphysema Features of Emphysema Chronic inflammation promotes lung fibrosis (tends to decrease lung compliance) Airways collapse during expiration Type II surfactant cells die, reducing surfactant production and decreasing compliance Alveoli enlarge as adjacent chambers break through, increasing lung compliance somewhat (easier to inflate) Patients use a large amount of energy to exhale, normally a passive process Overinflation of the lungs leads to a permanently expanded barrel chest Cyanosis appears late in the disease The Respiratory System I: Anatomy Functions of the Respiratory System The Nasal Cavity and Sinuses Pharynx, Larynx, & Trachea Respiratory Mucosa Lungs: Lobes, Bronchioles, & Alveoli Mechanics of Breathing • Pressure Relationships • Inspiration and Expiration • Lung Compliance