Blood Composition and Function
advertisement

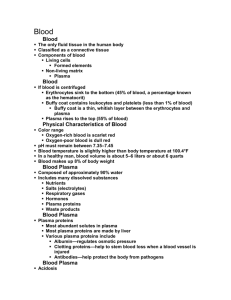
Blood Composition and Function General Composition of Blood • Plasma • Formed Elements Erythrocytes Leukocytes Hematopoesis Hemostasis (Clotting) Transfusion and Blood Typing Developmental Aspects of Blood Blood Composition The only fluid tissue in the human body Classified as a connective tissue • Living cells = formed elements • Non-living matrix = plasma Color range • Oxygen-rich blood is scarlet red • Oxygen-poor blood is dull red pH must remain between 7.35–7.45 Blood temperature is slightly higher than body temperature Hematocrit: Percent of blood volume that is RBCs • 47% ± 5% for males • 42% ± 5% for females Figure 10.1 Blood Cell Types Blood Composition and Function General Composition of Blood • Plasma • Formed Elements Erythrocytes Leukocytes Hematopoesis Hemostasis (Clotting) Transfusion and Blood Typing Developmental Aspects of Blood Erythrocytes (Red Blood Cells) Main function is to carry oxygen Biconcave disks Essentially bags of hemoglobin; few organelles Anucleate (no nucleus) Outnumber white blood cells 1000:1 Contain the plasma membrane protein spectrin and other proteins Major factor contributing to blood viscosity Hemoglobin Molecular structure • Protein globin: two alpha and two beta chains • Heme pigment bonded to each globin chain Iron atom in each heme can bind reversibly to one O2 molecule Each Hb molecule can transport four O2 Sickle Cell Hemoglobin Causes Clotting Normal hemoglobin = HbA Sickle cell hemoglobin = HbS (mutation in single amino acid - missense) Pleiotropic Effects Seen if HbS present HbAHbA = normal HbAHbS = sickle cell trait HbSHbS = sickle cell disease/anemia Fetal Hemoglobin Binds O2 More Avidly Fetal circulation must extract oxygen from maternal circulation Fetal hemoglobin (HbF) binds O2 more avidly than normal hemoglobin (HbA) does Replaced by “adult” hemoglobin just after birth Blood Composition and Function General Composition of Blood • Plasma • Formed Elements Erythrocytes Leukocytes Hematopoesis Hemostasis (Clotting) Transfusion and Blood Typing Developmental Aspects of Blood Leukocytes (White Blood Cells) Differential WBC count (All total 4800 – 10,800/l) Formed elements Platelets Leukocytes Granulocytes Neutrophils (50 – 70%) Eosinophils (2 – 4%) Basophils (0.5 – 1%) Erythrocytes Agranulocytes Lymphocytes (25 – 45%) Monocytes (3 – 8%) Figure 17.9 Leukocyte Levels in the Blood Normal levels are between 4,000 - 11,000 cells per millimeter Abnormal leukocyte levels • Leukocytosis o Above 11,000 leukocytes/ml o Generally indicates an infection (bacterial, fungal, parasitic) o Also caused by some cancers, (including lymphocyte leukemia), hemhorrage, pneumonia • Leukopenia o Abnormally low leukocyte level (< 3,500/ml) o Commonly caused by certain drugs, radiation o Neutropenia (low neutrophil count) common in cancer patients receiving chemotherapy o HIV-AIDS, TB, malaria, influenza also cause leukopenia o Requires careful sanitation and “gowning up” for medical staff Types of Leukocytes Granulocytes • Granules in their cytoplasm can be stained • Include neutrophils, eosinophils, and basophils Agranulocytes • Lack visible cytoplasmic granules • Include lymphocytes and monocytes Figure 10.4 Characteristics of Formed Elements of the Blood N E B Characteristics of Formed Elements of the Blood L M Blood Composition and Function General Composition of Blood • Plasma • Formed Elements Erythrocytes Leukocytes Hematopoesis Hemostasis (Clotting) Transfusion and Blood Typing Developmental Aspects of Blood Hematopoiesis Subdivided into erythropoesis and leukopoesis Erythropoesis ccurs in red bone marrow Erythropoesis Steps 1. Ribosome synthesis 2. Hemoglobin accumulation 3. Ejection of the nucleus and formation of reticulocytes 4. Reticulocytes then become mature erythrocytes Stem cell Hemocytoblast Committed cell Developmental pathway Proerythroblast Early Late erythroblast erythroblast Phase 1 Ribosome synthesis Phase 2 Hemoglobin accumulation Phase 3 Ejection of nucleus Normoblast Figure 17.5 Reticulo- Erythrocyte cyte Fate of Erythrocytes Unable to divide, grow, or synthesize proteins Wear out in 100 to 120 days When worn out, are eliminated by phagocytes in the spleen or liver • Iron is salvaged for reuse • Heme is degraded to yellow the pigment bilirubin • Liver secretes bilirubin (in bile)) into the intestines Lost cells are replaced by division of hemocytoblasts Control of Erythrocyte Production Rate is controlled by a hormone (erythropoietin) Kidneys produce most erythropoietin as a response to reduced oxygen levels in the blood (hypoxia) Hypoxia can develop from hemorrhage, low O2 in air, insufficient hemoglobin Homeostasis is maintained by negative feedback from blood oxygen levels Platelets Important in Clotting Small fragments of megakaryocytes Formation is regulated by thrombopoietin Blue-staining outer region, purple granules Form a temporary platelet plug that helps seal breaks in blood vessels Stem cell Hemocytoblast Developmental pathway Megakaryocyte Platelets Blood Composition and Function General Composition of Blood • Plasma • Formed Elements Erythrocytes Leukocytes Hematopoesis Hemostasis (Clotting) Transfusion and Blood Typing Developmental Aspects of Blood Hemastasis: Blood Clotting Step 1 Vascular spasm • Smooth muscle contracts, causing vasoconstriction. Step 2 Platelet plug formation Collagen fibers • Injury to lining of vessel exposes collagen fibers; platelets adhere. • Platelets release chemicals that make nearby platelets sticky; platelet plug forms. Platelets Fibrin Step 3 Coagulation • Fibrin forms a mesh that traps red blood cells and platelets, forming the clot. Figure 17.13 Hemastasis Undesirable Clotting Thrombus • A clot in an unbroken blood vessel • Can be deadly in areas like the heart Embolus • A thrombus that breaks away and floats freely in the bloodstream • Can later clog vessels in critical areas such as the brain, causing a stroke (CVA) Bleeding Disorders Thrombocytopenia • Platelet deficiency • Even normal movements can cause bleeding from small blood vessels that require platelets for clotting Hemophilia • Hereditary bleeding disorder • Normal clotting factors are missing or deficiency in Vit. K. mild hemophilia Blood Composition and Function General Composition of Blood • Plasma • Formed Elements Erythrocytes Leukocytes Hematopoesis Hemostasis (Clotting) Transfusion and Blood Typing Developmental Aspects of Blood Blood Groups and Transfusions Large losses of blood have serious consequences • Loss of 15 to 30 percent causes weakness • Loss of over 30 percent causes shock, which can be fatal Transfusions are the only way to replace blood quickly Transfused blood must be of the same blood group Human Blood Groups Blood contains genetically determined proteins A foreign protein (antigen) on a donated RBC may be attacked by the immune system Blood is “typed” by using antibodies that will cause blood with certain proteins to clump (agglutination) Human Blood Groups There are over 30 common red blood cell antigens The most vigorous transfusion reactions are caused by ABO and Rh blood group antigens ABO Blood Groups and Alleles Components of Blood of this Type anti-A anti-B anti-B anti-A Rh Blood Groups and Hemolytic Deaseas of Newborns Named because of the presence or absence of one of eight Rh antigens (agglutinogen D) Dd dd Most Americans are Rh+ The danger is only when the mother is Rh– and the father is Rh+, and the child inherits the Rh+ factor • Problems can occur in second and subsequent pregnancies when the baby’s Rh+ blood enters Rh– maternal circulation: erythroblastosis fetalis (hemolytic disease of the newborn) • RhoGAM injections contain anti-Rh antibodies that quickly clear the maternal circulation of Rh protein Dd dd This baby, if from the second or subsequent pregnancy, could have complications in an Rh- mother Blood Composition and Function General Composition of Blood • Plasma • Formed Elements Erythrocytes Leukocytes Hematopoesis Hemostasis (Clotting) Transfusion and Blood Typing Developmental Aspects of Blood