Document 15682114
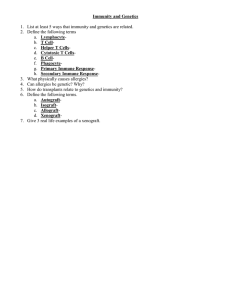
advertisement

The Immune System The body’s protective response to invading foreign organisms Immune System: Functions Protects from pathogens and foreign molecules Parasites Bacteria Viruses Removes dead/damaged cells Attempts to recognize and remove abnormal cells Immune System: Pathologies Incorrect responses Autoimmune disease Overactive responses Allergies Lack of response Immunodeficiency disease (AIDS) Body Defenses: Two Lines First line of defense Physical and chemical barriers: Skin, epithelial linings, and cilia Acids, mucous, and lysozymes Second line of defense Innate, non-specific, immediate response Acquired; attack a specific pathogen (antigen) 3 processes needed for immunity: Inflammation Immunity Cell-mediated Immunity Antibodymediated/Humoral Lymphatic System: Anatomy Figure 24-2a Key Cells of the Immune System Leukocytes (white blood cells) Cells of the Immune System Figure 24-4 Cells Leukocytes: 5 major categories. Neutrophils: Phagocytic cells that wander throughout the connective tissue destroying bacterias. Eosinophils: Phagocytic cells that destroy allergens, antigen & anti-body complexes, & some inflammatory chemicals. Surround larger parasites & attack them with enzymes to weaken or destroy them. Defend against allergies & parasitic worm infections. Basophils: Helper cells that secrete vasodilators & anticoagulants in order to speed other leukocytes to the infected zone. Cells Lymphocytes: A variety of cells active in the immune response. Natural Killer Cells (NK Cells): Attack any cell with an unusual plasma membrane, such as cells that are infected by a virus or have become cancerous. Cytolysis: Perforin protein is injected into the cell to cause it to “explode”. Granzymes: Cause the cell to self-destruct. Found in the spleen, red bone marrow, & lymph nodes. Monocytes: Wandering cells that eventually turn into macrophages. Inflammation (natural immunity) Inflammation: One of the body’s most common responses to tissue damage. Occurs in roughly the same way in any tissue. Four Cardinal signs of Inflammation: Redness Swelling Heat Pain Major cells of inflammation: Neutrophils: 1st line defense against invaders in blood and ECF. Destroy invaders by phagocytosis Absolute neutrophil count is used to determine a person’s risk for infection Major cells of inflammation: Macrophages Preform phagocytosis, repair injured tissue Stimulate CMI + AMI Long life span and plenty of energy to degrade many foreign proteins. Cells Phagocytes •Cells under attack release histamine. •Purpose is to engulf and destroy invaders Major cells of inflammation: Basophils Cause the manifestation of inflammation Contain chemicals that act on b. vessels Heparin inhibits blood clotting Histamine constricts small veins & respiratory smooth muscle Major cells of inflammation: Eosinophils Act against infestations of parasitic larvae Can inhibit and induce inflammation Number increases during allergic reaction Immune System Specific Immune Defenses: Cells specifically geared toward fighting certain invaders, and remembering previous foreign invaders so that they can be rapidly eliminated in the future. Immune System Two Divisions of the Immune System: 1. Humoral Immunity aka AntibodyMediated Immunity: 2. Driven by B cells. Cell-mediated immunity: Driven by T cells. What is specific immunity? Specific response Memory for future reinvasion Antibody-based B cells primary actors Cell-mediated T cells only Antigens Antigen: Typically large molecules, often proteins. Antigen Processing Major Histocompatability Complex (MHC): “Self-antigens” that are unique to all of your body cells except red blood cells. Help T-cells recognize which cells are foreign. MHC-1s: Cells that posses MHC and are labeled “you” by the T-cells. Antibodies Also known as immunoglobulins Some act as labels to identify antigens for phagocytes Some work as antitoxins Some attach to bacteria making them less active i.e. block toxins for e.g. those causing diphtheria and tetanus easier for phagocytes to engulf Some cause agglutination (clumping together) of bacteria Humoral Immunity Humoral Immunity aka AntibodyMediated Immunity B cells (B-lymphocytes) produce antibodies to engage in a complex purging process. Immunoglobulins Antibodies made up of glycoproteins called globulins. Antigen-Binding (Igs) Site Tips of each chain are called variable regions & are areas where the antibody attaches to the antigen. B -Lymphocytes Receptors recognize an antigen on the surface of the invader, the B-cell divides rapidly. Antigens are presented to the B-cells by macrophages B -Lymphocytes Type Number of ag binding sites Site of action Functions IgG 2 •Blood •Tissue fluid •CAN CROSS PLACENTA •Increase macrophage activity •Antitoxins •Agglutination IgM 10 •Blood •Tissue fluid Agglutination IgA 2 or 4 •Secretions (saliva, tears, small intestine, vaginal, prostate, nasal, breast milk) •Stop bacteria adhering to host cells •Prevents bacteria forming colonies on mucous membranes IgE 2 Tissues •Activate mast cells HISTAMINE •Worm response When help arrives . . . The T-helper cell receptor “docks” with the B cell’s MHComplex B cells proliferate . . . Antigen & T-helper cell Naïve cell Proliferation of cell line B cells differentiate into . . . Antibody producing cells [attack mode] Memory cells [remembers & future protection] Antigen & T-helper cell antibodies memory AMI in summary An invaders attacks… Antigen is phagocytized by the B cell Broken into non-infective pieces & attached to MHC which is placed on the cell membrane surface here it is recognized by the helper T cell… Cell Mediated Immunity Cellular Immunity: Lymphocytes directly attack & destroy foreign cells & infected host cells. T-Cells or T-lymphocytes activated by a specific antigen. Cellular Immunity Types of T-Cells involved in Cell-mediated Response: Cytotoxic T-Cells: Responsible for actual attacking of the foreign body or infected cell. Helper T-Cells: Stimulate other helper Tcells, cytotoxic T-cells, and B cells. Suppressor T-Cells: Help regulate the attack & prevent tissue destruction. Memory T-Cells: Remain as an immune response and stimulate faster responses if the same antigen invades again. T Lymphocytes: Cell-Mediated Roles of T lymphocytes and NK cells in cellmediated immunity Figure 24-16 What happens in a cellmediated response? The key events: Surveillance Attack Memory and recognition Types of Immunity Active Immunity: You encountered the pathogen yourself and developed your own antibodies to it. Passive Immunity: You received antibodies directly introduced into the body. Naturally Acquired: Antibodies are received through natural means. Artificially Aquired: Antibodies are received through artificial (scientific) methods. Vaccination A preparation containing antigenic material: Whole live microorganism Dead microorganism Attenuated (harmless) microorganism Toxoid (harmless form of toxin) Preparation of harmless ags Disorders of the Immune System Hypersensitivity Disorders Allergy Anaphylaxis Transfusion reactions, transplant rejection Immunodeficiency Disorders HIV/AIDS Autoimmune Systemic lupus erythematosus, rheumatoid arthritis etc. Hypersensitivity Excessive reaction to an antigen (allergen) to which most people do not react Includes Allergies Transplant reaction Transfusion Hypersensitivity Disorders Reaction may be Local (gastrointestinal, skin, resp, conjuctaval) or systemic (anaphylactic) Q: What factors affect the severity of a hypersensitivity reaction? Host response Exposure amount Nature of the allergen Route of allergen entry Repeated Exposure ( Hypersensitivity Assessment Subjective Information Pruritus, nausea and uneasiness History of present illness Onset, frequency and duration of symptoms Nature and progression of s/s Possible exposures of known allergens/common allergens Chronic, seasonal or single episode Aggravating & alleviating factors Hypersensitivity Assessment Physical Assessment Respiratory Cardiovascular S/Sx caused by Vasodilation—Flushing, Hypotension, Edema Shock followed by cardiovascular collapse and respiratory arrest GI S/Sx caused by Bronchoconstriction—SOB, difficulty breathing, wheezing, & coughing Sneezing, excessive nasal secretions, inflamed nasal membranes Nauses, vomiting, diarrhea Skin Rash, areas of raised inflammation (urticaria/hives) Hypersensitivity Studies & Medical Management Studies—CBC, Total serum IgE levels, skin testing Medical Management Immediate intervention Symptom management & long term control Environmental control Hypersensitivity—Medications Oxygen—if respiratory assistance needed Bronchodilators Antihistamines—symptom management & long term control First Generation—Prototype Diphenhydramine Second Generation—Prototype Fexofenadine Leukotriene inhibitors—Inhibits the release of leukotrienes from mast cells & basophils) Emergency bronchodilator—Epinephrine 1:1,000 SQ– Anaphylactic reactions (may need to following with IV Epi) Prototype—montelukast (Singulair) Steroids—symptom management & long term control Systemic—Prototype Prednisone Allergies When the immune system responds to harmless substances Allergens – antigenic substances Allergens include house dust, animal skin, pollen, house dust mite and its faeces Immunoglobulins and Allergic Response Allergen triggers the B cell to make IgE antibody, which attaches to the mast cell; when that allergen reappears, it binds to the IgE and triggers the mast cell to release its chemicals Allergic Responses First exposure Sensitization Activation, clone B cells, form antibodies and memory cells Re-exposure Many antibodies, activated T cells, intensified response, inflammation Allergies Histamine causes blood vessels to widen and become leaky. Fluid and white blood cells leave capillaries. The area of leakage becomes hot, red and inflamed Hypersensitivity—Latex Allergies Latex products in health care—Gloves, tourniquets, electrode pads, tape, urinary catheters, B/P cuffs, stethoscopes, IV tubing & syringes, O2 masks, etc. Type I anaphylactic hypersensitivity reaction from rubber latex proteins Exposure—skin, mucous membranes, inhalation or blood Reaction—ranges from erythema, urticaria, rhinitis, conjuctivitis to asthma & full blown anaphylactic shock Latex Allergy Risk factors for latex allergies Long term exposure Hx of hay fever, asthma & allergies to certain foods Fruits/vegetables—avocado, guava, kiwi, bananas, tomatoes, peaches, grapes, apricots, potatoes Nuts—water chestnuts, hazelnuts, peanuts NIOSH Recommendations—National Institute of Occupational Safety & Health Gloves—powder free, non-latex when unlikely to be in contact with infectious materials, avoid oil-based hand lotions when wearing glove, hand wash w/ soap after removal Frequent cleaning of areas with latex-containing dust Know s/sx of latex allergy—if symptoms develop avoid direct contact with latex gloves and products Medical-alert bracelet & Epi pen Hypersensitivity—Anaphylaxis Most severe IgE-mediated allergic reaction Potentially fatal Symptoms are often severe with a rapid onset Fall in B/P, laryngeal edema, bronchospasms leading to CV collapse, MI and Resp. failure First sign may be an “uneasiness” or “sense of impending doom” or nausea followed quickly by respiratory difficulty and a drop in B/P Signs—wheezing/stridor, severe dyspnea, congestion, tachycardia, hypotension, cyanosis, pallor, N/V, diarrhea Anaphylaxis Decision tree for patient with anaphylactic reaction Hypersensitivity—Anaphylaxis Patient education Avoidance of allergen S/Sx requiring immediate medical intervention Medication management Self administration of subcut epinephrine (Epi-pen) Importance of Benadryl in addition to epinephrine Prevention—taking preventive medications as ordered Medic-alert identification Hypersensitivity—Transfusion Reactions Mild to moderate hypersensitivity reactions S/Sx—Low grade fever, possible chills, urticaria, diarrhea, cough Stop the transfusion, administer NS IV, Benadryl, Tylenol, diuretic and a possible steroid Restart transfusion after symptoms subside at a slower rate Hemolytic reactions S/Sx—Fever, chills/rigors, urticaria, wheezing, hypotension Stop the transfusion, O2, NS IV, epinephrine (severe), antihistamines Hypersensitivity—Transplant Rejection “Graft versus Host Disease” GVHD Reaction occurs approx 7-10 days after transplant once blood supply to new tissue has developed Sensitized lymphocytes cause sloughing at the graft site Long-term immunosuppressive therapy— Corticosteroids (Prednisone), cyclosporin (Sandimmune) & azathioprine (Imuran) Immunodeficiency Disorders Primary Genetic May affect phagocytic function, B cells and/or T cells, or the complement system Secondary Acquired Contributing causes: Burns, malnutrition, chronic stress, diabetes Primary Immunodeficiency's Usually seen in infants and young children Manifestations: vary according to type; severe or recurrent infections; failure to thrive or poor growth; and positive family history Potential complications: recurrent, severe, potentially fatal infections Treatment: varies by type; treatment of infection; pooled plasma or immunoglobulin; GM-CSF or GCSF; thymus graft, stem cell, or bone marrow transplant Immunodeficiency—Nursing Management & Patient Teaching Monitor for S/Sx of infection Monitor lab values Dietary support Management of stress & anxiety Reduce risk of infection—hand washing, hygiene, avoiding crowds Medication management Autoimmune Disorders Development of a cellular and/or humoral response to one’s own tissue Disorders tend to cluster—many individuals have more than one autoimmune disorder Genetic predisposition likely Examples—rheumatoid arthritis (RA), systemic lupus erythematosus, ulcerative colitis, multiple sclerosis (MS), psoriasis, type 1 diabetes, etc Treatment Symptom management Plasmapheresis/plasma exchange—removal of plasma (immunoglobuin—IgG, antigen-antibody complexes, & inflammatory mediators) and replacement with NS, LR, FFP or albumin Immunosuppressive therapy to prevent recovery of IgG production Autoimmune Diseases