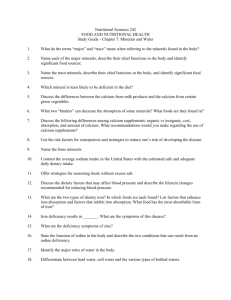
WATER
advertisement

WATER The water in body fluids: • Carries nutrients and waste products throughout the body • Maintains the structure of large molecules such as proteins and glycogen • Participates in metabolic reactions • Aids in regulation of body temperature • Maintains blood volume and pH balance • Acts as a lubricant and cushion around joints and inside eyes, and the spinal cord ELECTROLYTES • • • • • Water in the body contains numerous dissolved minerals, called electrolytes, that are kept in constant balance When salts, such as NaCl, dissolve in water, they break apart into + and – ions + = cations (sodium and potassium) - = anions (chloride and phosphate) Unlike pure water which conducts electricity poorly, ions dissolved in water carry an electrical current, hence they are called electrolytes ELECTROLYTES Na+ is the major cation in the extracellular fluid, K+ is the predominant cation in the intracellular fluid ELECTROLYTES • • • • The balance of body fluids and the amount of electrolytes are controlled precisely In an electrolyte solution, the amount of + charges always equals the amount of negative charges Whenever Na+ leaves a cell, other +ions enter (like K+) Whenever electrolytes move across the cell membrane, water follows WATER EXCRETION • • • • Our body loses water through: the skin, lungs, feces (very little), urine Depending upon the amount of protein, water, and sodium consumed, we lose 1-2L each day through the urine Insensible water loss accounts for ~ ¼ to ½ of daily fluid loss Losses increase in: exercise, high altitude, low humidity, high temperatures, illness (coughing, fever, rapid breathing, and watery nasal secretions) Regulation of Fluid Excretion • • • • The kidneys adjust the amount and concentration of urine in response to the body’s hydration status Low water intake = low volume of concentrated urine High water intake = high volume of diluted urine Osmoreceptors and antidiuretic hormone (ADH) work together to regulate water excretion THIRST • • • Thirst is not always a reliable guide to avoiding dehydration Athletes, elderly people, and infants are vulnerable to dehydration How can we avoid dehydration? From the International Journal of Sports Nutrition • • Researchers concluded that “urine color may be used in athletic/industrial settings to determine whether a subject is adequately hydrated” Suggested that athletes (and others) should seek to produce urine that is “very pale yellow” or “straw-colored” WATER INTAKE RECOMMENDATIONS • • • There is no RDA for water General recommendation: 1 to 1.5 mL per kcals expended (2400 kcal = 2400 mL or 2.4 litres) Equals ~ 9.6 cups of water per day WATER SOURCES • • • Hydrating beverages: water, milk, fruit juice, herbal tea, most foods (especially fruits and vegetables) Dehydrating beverages: alcohol, caffeinated beverages (coffee, tea, some soft drinks) Are Americans chronically dehydrated? Per capita median intake of water 672 ml (2.8 cups) Per capita milk intake 312 ml (1.3 cups) Per capita coffee and tea intake 360 ml (1.5 cups) Per capita soft drink intake 420 ml (1.75 cups) Total per capita fluid comsumption 1764 ml (7.35 cups) What are the effects of chronic dehydration? • • • • Diminished physical performance Diminished mental performance Diminished salivary gland function Increased risk of urinary tract, colon, and breast cancer* • Is it possible to take in too much water? HYPONATREMIA: Low concentration of sodium in the blood • Symptoms: can range from mild to severe and can include nausea, muscle cramps, disorientation, slurred speech, confusion, and inappropriate behavior • Seizures or coma, and death can occur Do we need to replace electrolytes during exercise? Plus approximately 30mg potassium DIURETICS • • A diuretic is any substance that increases fluid loss through increased urination Alcohol and caffeine act as diuretics by inhibiting ADH activity MAJOR MINERALS: Sodium • • Sodium acts in concert with potassium and chloride to maintain proper body water distribution and blood pressure Sodium also helps to maintain acidbase balance, nerve transmission, muscle function, and absorption of nutrients such as glucose SODIUM: Sources • • Most of the sodium in our diet comes from processed foods (75%) The other sources are natural sodium in foods (10%) and salt added during cooking and eating (15%) SODIUM: Requirements Estimated minimum requirement for sodium: 500 mg/day Recommended maximum intake of salt: 6 g/day (2400 mg sodium). – 5 g salt = about 2 g sodium – 3 g salt = 1.2 tsp HYPERTENSION Chronic High Blood Pressure • • • • Hypertension injures the artery linings and accelerates plaque formation Plaques and reduced blood flow induce a further rise in blood pressure, and HTN and atherosclerosis become mutually aggravating conditions Diagnosis: diastolic pressure >90mmHg and/or systolic pressure >140mmHg (men) and >160mmHg (women) These values are associated with an increase in mortality of over 50% SODIUM and HYPERTENSION • • • Our bodies are poorly adapted to handle our modern high sodium, low potassium diets. (The diet of our ancestors is estimated to have contained 16 times more potassium than sodium.) About 10-15% of people with hypertension are “salt-sensitive”. If these people decrease their sodium intake, their BP decreases For non “salt-sensitive” people, reducing salt intake has a minimal effect on BP HYPERTENSION Other Dietary Factors: • Excess weight tends to raise BP, exercise and weight loss help to reduce it • Alcohol consumption can increase BP • Diets rich in calcium, magnesium, and potassium help to reduce BP POTASSIUM • Like sodium, potassium is important in regulation of blood pressure, nerve transmission, muscle contractions, electrolyte balance, and cell integrity POTASSIUM: Sources • • Good sources include fresh fruits and vegetables, especially bananas, potatoes, spinach, legumes, squash, and melons Fresh meat, milk and yogurt, coffee and tea are other good sources FUNCTIONS of IRON OXYGEN TRANSPORT • Most of the body’s iron is found in two proteins: hemoglobin and myoglobin • In both, iron helps to accept, carry, and then release oxygen • Hemoglobin in RBCs transports oxygen to the blood • Myoglobin facilitates the movement of oxygen into muscle cells FUNCTIONS of IRON ENZYMES • Iron is a component of enzymes involved in energy metabolism (cytochromes are hemecontaining compounds in the ETC) • Iron is also required by enzymes involved in the making of amino acids, collagen, hormones, and neurotransmitters • It is also a cofactor for antioxidant enzymes FUNCTIONS of IRON IMMUNE FUNCTION • Iron is necessary for optimal immune function • Iron deficiency decreases concentrations of lymphocytes, natural killer cells, and other immune factors • Iron overload can worsen an infection because it serves a nutrient for bacteria FUNCTIONS of IRON OTHER • Iron is used by brain cells for normal function at all ages: in the synthesis of neurotransmitters, and possibly a role in myelinization • Synthesis of niacin from tryptophan, carnitine synthesis IRON IN THE BODY • • More than 80% of the body’s functional iron is found in the RBCs, and the rest is in myoglobin and enzymes The body regulates its iron status by balancing absorption, transport, storage, and losses IRON ABSORPTION • • • • • Iron absorption in the gastrointestinal tract is the primary regulator of iron levels It depends upon: Normal GI function The amount and kind of iron consumed Dietary factors that effect iron absorption IRON ABSORPTION • • • • Absorption can vary from less than 1% to greater than 50% depending upon: Body iron stores Certain conditions – pregnancy, blood loss, menstruation Gender – men absorb less than women IRON ABSORPTION • • • • • Foods contain two types of iron – heme and non-heme Heme iron is supplied by animal foods which also contain non-heme iron (~40% heme, 60% non-heme) Plant based foods contain only non-heme iron Heme iron is 2 to 3 times more absorbable than non-heme iron People with severe iron deficiency absorb both heme and non-heme iron more efficiently IRON ABSORPTION Dietary Factors • Organic acids (like Vitamin C) and meat boost absorption of non-heme iron • Phytates, polyphenols (found in tea and coffee), oxalates (spinach), calcium and phosphorus, EDTA (food additive), and fiber inhibit non-heme absorption IRON TURNOVER and LOSS • • • • The body recycles iron, and adjusts absorption and excretion as needed In adult men, the breakdown of older RBCs supplies ~95% of the iron required to produce new RBCs Adults lose ~1mg per day in the feces, intestinal cells, and skin Women require additional iron to compensate for blood loss during menstruation SOURCES of IRON • • • Good sources include beef, clams, oysters, tofu, legumes, and liver Fortified cereals provide iron in the American diet Foods cooked in iron cookware take up iron salts. The more acidic the food, and the longer it is cooked, the higher the iron content. However, the absorption may be poor IRON DEFICIENCY • • Stages of Iron Deficiency: depletion of iron stores – depletion of functional iron – iron deficiency anemia Iron-deficiency anemia is characterized by microcytic, hypochromic RBC IRON TOXICITY • • • • Iron poisoning is the leading cause of accidental death in small children In a condition called Hemochromatosis, a genetic defect causes excessive iron absorption. Iron builds up in many parts of the body, leading to severe organ damage and even death An intake in excess of the RDA by adult men and postmenopausal women may increase risk for heart disease and cancer Excessive iron helps to generate large amounts of free radicals that attack cellular molecules CALCIUM: Functions • • • Bone Structure: as bones begin to form, calcium salts form crystals called hydroxyapatite, on a matrix of collagen. During mineralization, as the crystals become denser, they give strength and rigidity to maturing bones The calcium in bones serves as a calcium “bank” Peak bone mass occurs at ~ 30 years of age CALCIUM: Functions • • • • Nerve function Blood clotting Muscle contraction Cellular metabolism CALCIUM: Sources • • • • • • Dairy products, blackstrap molasses, canned fish with bones, almonds, sesame seeds, some dark green leafy vegetables Depends on bioavailability: >50% absorbed – kale, mustard greens, bok choy, turnip greens, broccoli, calcium-fortified foods and beverages ~30% absorbed – dairy foods, calcium set tofu ~20% absorbed – almonds, sesame seeds, pinto beans <5% absorbed – swiss chard, spinach, rhubarb CALCIUM ABSORPTION • • • The body normally absorbs 25 to 75% of dietary calcium, depending upon Vitamin D, the body’s need, and calcium intake Calcium absorption is highest during pregnancy and infancy, lowest in old age Phytates, high levels of phosphorus and magnesium, and low estrogen levels can decrease absorption OSTEOPOROSIS • • Osteoporosis is one of the most prevalent disease of aging, affecting more than 25 million people in the US – most of them women The disease occurs when the bone mineral density becomes so low that the skeleton is unable to sustain ordinary strains, a condition marked by the occurrence of fractures BONE BUIDLING NUTRIENTS • • Calcium, phosphorus, fluoride, magnesium, potassium, Vitamin A, Vitamin D, Vitamin K Possibly iron, copper, zinc, manganese, and boron - function in bone metabolism, but their roles in preventing bone loss are not well established OSTEOPOROSIS Dietary Factors • Excessive dietary fiber may interfere with calcium absorption • Excessive animal protein consumption may lead to increased urinary calcium excretion • High sodium intakes, especially in association with low calcium intakes, can result in increased urinary calcium excretion • Caffeine can reduce calcium absorption and increase excretion rates • High phosphorus intake, in association with low calcium intake may increase bone loss PREVENTION of OSTEOPOROSIS • • • Increase intake of bone-building nutrients Reduce consumption of alcohol, tobacco, caffeine, sodium, and animal protein Engage in regular weight-bearing exercise OSTEOPOROSIS Risk Factors: • Aging, female sex, limited intake of bone building nutrients, excessive consumption of potentially damaging substances (alcohol, tobacco), sedentary lifestyle, lack of sunlight, decreased estrogen levels, genetics, and race REGULATION of BLOOD CALCIUM • • • • Vitamin D Parathyroid Hormone Calcitonin Figure 11.19 CALCIUM ABSORPTION • • • The body normally absorbs 25 to 75% of dietary calcium, depending upon Vitamin D, the body’s need, and calcium intake Calcium absorption is highest during pregnancy and infancy, lowest in old age Phytates, high levels of phosphorus and magnesium, and low estrogen levels can decrease absorption