Wernicke-Korsakoff Syndrome: Neurological Effects of Chronic Alcohol Dependence Patrick J. Macmillan, M.D.
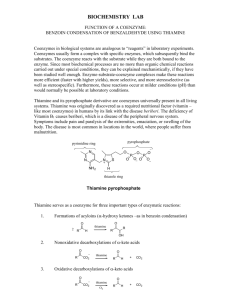
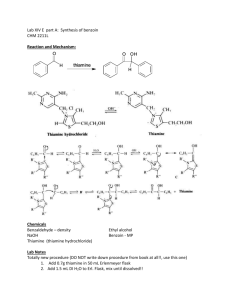
advertisement

Wernicke-Korsakoff Syndrome: Neurological Effects of Chronic Alcohol Dependence Patrick J. Macmillan, M.D. Assistant Professor James H. Quillen College of Medicine East Tennessee State University HPI 62 year old WM, divorced veteran brought to ER by his brother after falling; Reported to have been drinking alcohol; History of Etoh abuse per chart. brother found him conscious on the floor. Has been urinating on self. Patient denies drinking since 1984 and reports being brought here by taxi. Poor historian; unknown if patient has history of DT’s or Seizures The power of denial PMH COPD (by history) HTN Alcohol Abuse SurgHx Fx left clavicle repair FH Parents Deceased: Father: MI; Mom CA Uncle: alcoholic Psychosocial Hx Lived with both parents; finished 8th grade Receives SSI check Hx of Alcohol Abuse 40+ years(several detox admissions) +Tobacco 75 pack years + h/o suicidal acts: OD/cut wrists 25 yrs ago Worked in Cleveland, OH Ford Motor Company Hx of Incarceration: 2nd degree murder Medications Albuterol Inhaler Atenolol Naproxen Methocarbomol Allergies Quinine ROS Unable to obtain; patient poor historian; PE VS: T 99.3, BP 167/90, HR 93, RR 18, O2 92% GEN: A/A/OX1; looks older than stated age HEENT: NC/AT, Nystagmus, ophthalmoplegia; R pupil>L pupil (aniscoria); MMM CVS: RRR; NO M/R/G; +S1,S2 ABD: RUQ/LUQ pain; No organomegaly; rectal heme negative Ext: +Clubbing; No edema or cyanosis PE Mental Status: Patient thinks he is Akron, OH; says he is 38 y/o; knows the President., confabulates Neurologic: CN III, IV and VI deficit; hyperreflexic (+3 DTR); gait unsteady; +Romberg Labs Potassium: 3.4; glucose 128; NH3 18; MCV 98.7; ABG pH 7.49; WBC 11.6;Mg 2.3; BAL –tive; UDS –tive;RPR –tive; EKG unremarkable CT head –tive; CXR emphysematous changes Diagnosis Wernicke Korsikoff Syndrome Acute neurologic disorder caused by thiamine (Vitamin B1) deficiency Oliver Sacks book, The Man Who Mistook His Wife for a Hat: Sack’s pt. in 1975. This patient thought he was a young man. This man was stunned when he looked in a mirror - and saw a middle-aged man looking back! Patient thought it was 1945. He had been a sailor as a young man in World War II. He had lost his ability to build and store new memories, and he had lost all the intervening years of experience. Sig. H/o of Etoh abuse Poor Judgement More Poor Judgement Historical Background: In 1881, Carl Wernicke first described an illness that consisted of paralysis of eye movements, ataxia, and mental confusion in 3 patients. Wernicke detected punctate hemorrhages affecting the gray matter around the third and fourth ventricles and aqueduct of Sylvius. He felt these to be inflammatory and therefore named the disease polioencephalitis hemorrhagica superioris Historical S.S. Korsakoff, a Russian psychiatrist, described the disturbance of memory in the course of long-term alcoholism in a series of articles from 1887-1891. He termed this syndrome psychosis polyneuritica, believing that these typical memory deficits, in conjunction with polyneuropathy, represented different facets of the same disease. In 1897, Murawieff first postulated that a single etiology was responsible for both syndromes. Introduction The term Wernicke encephalopathy is used to describe the symptom complex of ophthalmoplegia, ataxia, and an acute confusional state. If persistent learning and memory deficits are present, the symptom complex is termed WernickeKorsakoff syndrome. Wernicke's encephalopathy (WE) is an acute syndrome requiring emergent treatment to prevent death and neurological morbidity. Korsakoff's amnestic syndrome (KS) refers to a chronic neurological condition that usually occurs as a consequence of WE. Epidemiology: WE 0.8 to 2.8% at autopsy in general population (typical brain lesions) Majority are alcoholics Women more susceptible Rate is higher in homeless and psychiatric inpatients Mortality/Morbidity: 10-20% (prognosis depends on stage of disease and promptness of Tx) Deficiency in alcohol abusers results from a combination of inadequate dietary intake, reduced gastrointestinal absorption, decreased hepatic storage, and impaired utilization. Only a subset of thiamine-deficient alcohol abusers develop WE. identical twins> fraternal twins suggests a genetic predisposition Pathophysiology Thiamine deficiency in alcohol abusers Evidence: thiamine antagonist pyrithiamine causes experimental thiamine deficiency in rats, resulting in a sequence of ataxia, loss of the righting reflex, and convulsions. low levels of magnesium may also play role. Inherited or acquired abnormality of transketolase:This Causes for brain lesions unclear but possible NMDA receptor excitotoxicity and increased reactive oxygen species (free radicals) enzyme, together with transaldolase, provides a link between the glycolytic and pentose-phosphate pathways. (possibly alters affinity for thiamine) Basic Science Quiz Major disease a/w lung cancer? BSQ Premature death BSQ What is artificial insemination? BSQ When the farmer does it to the bull instead of the cow Pathophysiology Thiamine: cofactor of several enzymes, including Transketolase, alpha ketogluterate dehydrogenase, and pyruvate dehydrogenase Thiamine plays important role in cerebral energy utilization Deficiency initiates neuronal injury by inhibiting metabolism Krebs cycle Pentose Phosphate Pathway Pathophysiology Excitotoxicity may be final pathway Extracellular glutamate increases following seizure in thiamine deficient rats NMDA receptor antagonists reduce neurologic signs and severity of extent of lesions Pathology Lesions in area of Third ventricle, aqueduct and fourth ventricle Mamillary bodies: a/w memory access functions, particularly accessing stored knowledge to interpret sensory input. When damaged, memory loss or amnesia of specific areas of knowledge can result. Acute WE lesions characterized by vascular congestion, microglial proliferation, and petechial hemorrhages. In chronic cases, there is demyelination, gliosis, with relative preservation of neurons. Neuronal loss is most prominent in the relatively unmyelinated medial thalamus Pathology Cerebellar pathology is generally restricted to the anterior and superior vermis; thus, ataxia of the legs or arms and dysarthria or scanning speech are uncommon. Vestibular dysfunction may be the major cause of acute gait ataxia in WE. Anatomy Anatomy Anatomy:Coronal Section BSQ How are the main parts of the body categorized? (e.g., abdomen). BSQ The body is consisted into three parts the brainium, the borax and the abdominal cavity. The brainium contains the brain, the borax contains the heart and lungs, and the abdominal cavity contains the five bowels, A,E,I,O and U. BSQ Give the meaning of the term "Caesarean Section" BSQ The Caesarean Section is a district in Rome Clinical Encephalopathy, Oculomotor dysfunction, gait ataxia Encephalopathy: profound disorientation Oculomotor: nystagmus (usu horizontal), lateral rectus palsey, conjugate gaze palsey (usu. Occur in combination) Clinical Gait Ataxia: due to polyneuropathy, cerebellar involvement and vestibular peresis Stance and gait impairment May only be appreciated on tandem gait Features of triad only present in 1/3rd of pts in one study. Clinical Confusion is most common presenting symptom Malnourishment Vestibular dysfunction (w/o hearing loss) Peripheral neuropathy Korsakoff’s amnestic syndrome (80% of WE) Confabulation Diagnosis treatment takes priority over diagnosis, and response to treatment may be diagnostic There are no laboratory studies that are diagnostic of WE erythrocyte thiamine transketolase (ETKA) Diagnosis A serum thiamine or thiamine pyrophosphate level in serum or whole blood can also be measured by chromatography Imaging studies are not necessary in all patients with suspected WE and should not delay treatment. Diagnosis: Imaging Abnormalities in CT and MRI have been reported in a small numbers of patients with acute WE CT may show symmetric, low density abnormalities in the diencephalon, midbrain, and periventricular regions that enhance after the injection of contrast. Gross hemorrhages are uncommon in acute WE, but they have also been detected by CT. These findings are uncommon in other disorders, and when present, should strongly suggest the diagnosis. However, CT is an insensitive test for WE; a normal CT scan does not rule out the diagnosis Diagnosis: Imaging MRI more sensitive than CT in detecting acute diencephalic and periventricular lesions . Typical findings include areas of increased T2 and decreased T1 signal surrounding the aqueduct and third ventricle and within the medial thalamus and mamillary bodies. Diffusion-weighted imaging (DWI) is abnormal in these areas as well. The distribution of these findings is consistent with the pathologic lesions. MRI Imaging Diagnosis: Imaging Mamillary body (diencephalon)atrophy is a relatively specific abnormality in patients with chronic lesions of WE. Large decrease in the volume of the mamillary bodies can be identified by MRI in approximately 80 percent of alcohol abusers with a history of classic WE, and it is not found in controls, patients with Alzheimer's disease (AD), or alcohol abusers without a history of WE. Mamillary body atrophy can be detected within one week of the onset of WE Treatment IV thiamine 100 mg (or IM) for 5 days; “Banana Bag.” Telemetry DT prophylaxis (Benzo taper) REMEMBER: never give glucose before thiamine Daily oral thiamine (100 mg) following discharge Referral for Drug/Alcohol Treatment Clinical Course/Prognosis Prompt administration of thiamine leads to improvement in ocular signs within hours to days Confusion subsides over days and weeks. Signal abnormality on MRI resolves with clinical improvement While gaze palsies recovered completely in most cases, 60 percent had permanent horizontal nystagmus. Clinical Course/Prognosis 40 percent recovered from ataxia; remaining deficits ranged from inability to walk at all to a wide-based slow shuffling gait. As the acute encephalopathy and confusion receded, deficits in learning and memory become more obvious; the latter recovered completely or substantively in only about 20 percent; the remainder had a permanent amnestic syndrome. Prevention WE may be iatrogenically precipitated by glucose loading in patients with unsuspected thiamine deficiency. standard practice in emergency departments to administer thiamine prior to or along with glucose infusion. The prevention of WE and KS might be possible through the widespread oral administration of thiamine to outpatients at risk. Enrichment of flour with thiamine decreased the autopsy prevalence of WE in Australia Prevention The low cost and safety of oral thiamine argues for widespread supplementation in alcohol abusers and others at risk for developing thiamine deficiency. Fortification of alcoholic beverages has also been proposed. Summary WE and Korsakoff's amnesic syndrome (KS) are, respectively, acute and chronic brain disorders that result from thiamine deficiency. WE is most often associated with alcoholism but can also occur in other situations including malnutrition from any cause (e.g dialysis). WE produces hemorrhagic necrosis in midline brain structures and corresponding deficits in mentation, oculomotor function, and gait ataxia. Only one-third of patients present with triad. Any one of these, but most often encephalopathy, may be seen in isolation. WE should be considered when one or more occur. Summary laboratory measurements and neuroimaging are often abnormal in WE, but the first imperative is to administer thiamine rather than confirm the diagnosis, whenever WE is considered. Untreated, WE leads to coma and death. Prognosis is improved by prompt administration of thiamine. WE may be precipitated by administration of intravenous glucose solutions to individuals with thiamine deficiency. Thiamine supplementation, along with other multivitamin supplementation, is recommended for patients at risk for thiamine deficiency. BSQ What does the word "benign" mean? BSQ Benign is what you will be after you be eight Future of Psychiatry References Up to Date http://www.emedicine.com/med/topic2405.html http://stilt.genetics.utah.edu/reference/pdf_templa te.php?tpl=remember_amnesia http://spinwarp.ucsd.edu/NeuroWeb/Text/br800epi.htm http://www.people.virginia.edu/~rjh9u/krebs.html The End Any questions/comments??????