East Tennessee State University Quillen College of Medicine Kanishka Chakraborty, MD Assistant Professor
advertisement

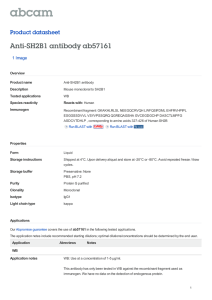
East Tennessee State University Quillen College of Medicine An Organ, A Disease and A Few Facts About Treatment Kanishka Chakraborty, MD Assistant Professor Department of Internal Medicine Division of Medical Oncology/Hematology References in slide 61 “Hallmark of this organ’s absence will be seen in our blood” Howell-Jolly bodies are round, purple staining nuclear fragments of DNA in the red blood cell. Etiologies of Splenomegaly Congestive: Cirrhosis, CHF and Thrombosis of portal, hepatic and splenic veins. Malignancy: Lymphoma, Chronic Myeloid Leukemia, Essential Thrombocytosis, Polycythemia Vera, Primary Myelofibrosis, Metastatic tumors. Infection: Infectious Mononucleosis, CMV, Hepatitis, Brucellosis, Tuberculosis, Malaria, Leishmaniasis and Infective Endocarditis. Inflammation: SLE, Sarcoid and Felty syndrome Infiltrative: Gaucher, Neimann-Pick, Glycogen storage disease and Amyloid Hematological: -Hemolytic anemia, Sickle cell disease and Use of G-CSF PMF or post PV/ET MF Differential diagnosis of PMF: -Metastatic cancer -Lymphoid malignancy -CML -MDS -CMML -AML Presence of +9 or 13qfavors PMF Presence of monocytosis >1 x109 /L directs toward CMML and Acute Megakaryoblastic leukemia can mimic PMF presentation Presence of JAK2 or MPL AND Absence of BCR-ABL1 Historical Perspective Galen (129-200 AD) Recognized blood as one of the four 'humors' (the other three being phlegm, black and yellow bile). Recognized plethora as an imbalance of the humors, where blood dominated over the others. Phlebotomy was practiced to maintain humoral equilibrium and became a universal treatment for a variety of unrelated conditions till the 19th century. Aggressive phlebotomy is believed to have contributed to the death of George Washington. In 1628, William Harvey (1578-1657), Demonstrated the circulatory nature of blood. Disproved many of Galen's fallacies including the belief that blood stagnation causes illness. This was the beginning of the end of phlebotomy as a remedy for all diseases. Historical Perspective 1845: First report of CML entitled : 'Case of hypertrophy of the spleen and liver in which death took place from suppuration of the blood'. John Hughes Bennett The clinical description of the patient was similar to other case by Rudolph Virchow. 1879: 1st description of primary myelofibrosis: “Two cases of leukemia with peculiar blood and bone marrow findings”. Described two young patients with massive splenomegaly, circulating nucleated red blood cells, and increased number of morphologically abnormal leukocytes. ‘Splenicmedullary leukemia' and 'pure splenic leukemia’. Different from CML because of the presence of marrow fibrosis and extensive extramedullary hematopoiesis. Gustav Heuck (1854-1940) William Dameshek (1900-1969) Founder of Blood, the prime core clinical journal of hematology, in 1946. He is also credited with describing the concept of myeloproliferative diseases in 1951. -PV, ET, PMF and CML described by Dr. Dameshek as classic MPN -PV, ET and PMF known as bcr-abl negative MPN. He participated in the first studies of nitrogen mustard in various hematological malignancies, widely considered the first uses of chemotherapy in malignant diseases. Dr. Dameshek was also the first one who described chronic lymphocytic leukemia (CLL), a common form of leukemia in adults. xx Incidence: PMF is least common among chronic Myeloproliferative disorders. One study reported an estimated incidence of 1.5 per 100,000 per year in Olmsted County, Minnesota. Occurs mainly in middle aged and elderly patients. Median age at presentation is 67 years. Approximately 5 and 17 percent of the patients are diagnosed before the age of 40 and 50 years Clinical Presentation: Most common presentation is with severe fatigue, 50 to 70 percent of patients. 25 to 50 percent of patients present with Splenomegaly. Weight loss . Low-grade fever. Night sweats. Approximately 15 to 30 percent are asymptomatic and diagnosis is made during investigation for hepato-splenomegaly and/or abnormal blood indices. Disease Features: Pruritus, not correlated with overall survival, karyotype, risk category and plasma level of cytokines. Splenomegaly. Hepatomegaly. Pulmonary hypertension, associated with reduced overall survival. Thrombotic events: Both arterial and venous thrombosis happen. Incidence is similar to Essential thrombosis (ET) but lower than Polycythemia Vera (PV). Portal vein thrombosis is a well recognized complication. Extramedullary Hematopoiesis: Beside Liver and Spleen, other common sites are thoracic vertebral column, Lymph node, retroperitoneum, Lungs, GI, skin and other sites. (Post Splenectomy, other EMH sites can enlarge, this may be particularly challenging in patients developing liver failure). Bone and Joint involvement. PMF, post-PV and post-ET MF include following laboratory features: Anemia, 28% cases of PMF. Leuko-erythroblastosis. Dacrocytosis. Leukocytosis/thrombocytosis. Elevated LDH. Increased blasts or CD34+. Bone marrow fibrosis. Osteosclerosis. Angiogenesis. Anemia: 50 percent of patients will have Hgb of <10.0 -Decreased in medullary hematopoietic sites. -Ineffective hematopoiesis in EMH sites. -Splenic sequestration. -Blood loss. -Autoimmune Hemolysis. -Dilutional. -MPL mutation. -PBS features (Anisocytosis, Polikilocytosis, Tear drop cells, nucleated red blood cell and Polychromasia). Platelet and WBC: Variable abnormalities on presentation. 11-13 patients present with increased count and 8-26% with low count. CD34+ cells: An Italian study showed 400 times increase compared to normal healthy subjects with an average of 92 CD34 cells/microL in PMF. Other abnormal blood parameters: Elevated LDH, Uric acid, Leucocyte alkaline phosphatase, Alkaline phosphatase and B12. Bone marrow aspiration and Biopsy: -“Dry" tap. -Neutrophilic and megakaryocytic hyperplasia. -Granulocytes with hyperlobulation -Erythroid precursors may be normal or increased. Biopsy shows: -Bone marrow sinusoids are expanded and shows presence of intravascular hematopoiesis. -Fibrosis is typically extensive and visualized better with a silver stain (reticulin) or a trichrome stain (mature collagen) “Classic ph -” MPN Common Characteristics: Despite differentiation / maturation; they originate from a single progenitor cell. Normal cellular maturation. Striking overlap in clinical presentation. Propensity to evolve into post PV or post ET MF. Possibility to transform into AML. PV,ET relatively indolent. Modest reduction of lifespan. PMF has a severe course in most cases. Survival significantly affected. PMF: (Pathogenesis) Clonal myelo-proliferation (Chromosomal abnormality and JAK2/STAT pathway deregulation) and secondary inflammation. Myeloid cell derived transforming growth factor-beta, PDGF, FGF-beta, VEGF mediate BM fibrosis, osteosclerosis and angiogenesis. Abnormal cell-cell interaction leads to -Abnormal release of cytokines, chemokines and extracellular matrix metalloproteinase. -Also contributes to release of CD34 myeloid progenitors in peripheral circulation. Elevated level of IL8, IL10, IL15 and IL2 associated with constitutional symptoms, cachexia, inferior overall survival and poor leukemia free survival Molecular Basis of MPN CML : BCR/ABL rearrangement. Systemic Mastocytosis : kit mutations. Information concerning molecular abnormalities of CLASSIC ph- MPN has been scanty until 2005. In 2005 several independent groups used different approaches to identify a recurrent mutation in most MPN patients. MPN, stem cell derived monoclonal or polyclonal hematological malignancies may have a genetic predisposition Major mutation is JAK2V617F, other mutations are MPL, LNK, CBL, TET2, ASXL1, IDH, IKZF1 and EZH2 Disease initiating mutation in MF is not known; also they are not disease specific and also can appear as secondary events xx xx Molecular Basis Of MPN Mutation Disorder Frequency Polycythemia vera >95% Essential thrombocythemia 60% Primary myelofibrosis 60% MPN, unclassifiable 20% JAK2V617F Refractory anemia with sideroblasts and 50% thrombocytosis (RARS-T) JAK2 exon 12 Polycythemia vera 2% Primary myelofibrosis 8% Essential thrombocythemia 8%† MPLW515L/K JAK Family • One of 10 recognized families of non-receptor tyrosine kinases. • Mammals have four members of this family, JAK1, JAK2, JAK3 and Tyrosine Kinase 2 (TYK2) Proc Natl Acad Sci U S A. 1989 March; 86(5): 1603–1607. • Initially called Just Another Kinase, final publication used the term JAnus Kinase. JAK Family • JANUS: Roman god with two faces, meaning ending and beginning, because they contain two symmetrical kinase-like domains. JAK Family JAK1: mediating the signaling of pro-inflammatory cytokines. JAK1 defective mice have defective lymphoid development and function. JAK2 : JAK2 helps in transducing signals from several class I cytokine receptor (TpoR, EpoR and G-CSFR). Deficiency results in embryonic lethality at day 12 as a result of a failure in definitive erythropoiesis. JAK3: Transmitting IL-2 signals. Defective mice have SCID TYK2 : signaling of cytokines such as IL-12 and IL-23 In normal unstimulated situation JAK2 is noncovalently bound to class I receptors via N terminal FERM domain but it is in an inactive form. Binding of specific ligand like EPO to EpoR activates JAK2 signaling. BCR-ABL negative MPN: Direct or indirect dysregulation JAK2 by somatic acquired mutation. -Binding relieves negative regulation of catalytic activity imposed by JH2 domain -Activated JAK2 phosphorylates tyrosine residue on itself -This phosphorylated tyrosine residue works as a docking site for the recruitment and assembly of downstream signaling. -It results in activation of MAPK, PI3K and STAT proteins. xx xx Protein tyrosine phosphatases, suppressors of cytokine signaling (SOCS), CBL (Casitas B lineage lymphoma) protein inhibitors of activated STATs (Signal Transducer and activator) etc provide negative feedback to this signaling. Mutation that activates JAK2: GT change in exon 14, that results in substitution of normal valine residue at position 617 by phenylalanine. Mutation happens in JAK2 exon 12 too. Constitutive activation of JAK2 in the absence of class I receptor stimulation. Mutation takes of negative regulation imposed by JH2 domain. Indirect mutation can happen due to activating mutation of MPL gene (It encodes TpoR) (Present in ET and MF but not in PV). WHAT HAPPENS WITH JAK2 MUTATION: Mutated JAK2 escapes negative regulation by SOCS3; even more it exploits SOCS3 to help in myeloproliferative activity. SOCS3 is a strong negative regulator of EPO. Mutated JAK2 hyperphosphorylates SOCS3 and stabilizes it. Mutated JAK2 phosphorylates protein arginine methyltransferase 5 (PRMT5). Leading to inhibition of PRMT. Promoting increased colony formation and leading to important contribution to the MPN phenotype. Epigenetic Mutations: TET2, IDH1, IDH2, ASXL1, EZH2. Cytogenetic mutation: Gain of chromosome 9, deletions of 13q and 20q, trisomy 8 and partial trisomy of 1q Genetic Instability: In Treated CML patients with residual ET found to have both JAK2V617F and BCR-ABL mutation. Co-presence of JAK2 V617F mutation along with MPL W515, KIT D816V and JAK2 exon 12 mutation V617F positive MPN may transform to V617F negative AML, suggesting transformation of stem cell that has not acquired JAK2 mutation proving in favor of genetic instability. Presence of two different mutations in two different clones also suggest genetic instability. xx xx xx xx ‘Bird’s eye view of PMF prognostic factors” Unfavorable karyotype includes complex karyotype or trisomy 8, -7/7q-, i(17)q, -5/-5q, 12p- 0r 11q23 rearrangement. Leukemic transformation is predicted by the presence of unfavorable karyotype or Platelet count <100x109 /L. Presence or absence of JAK2. Ten-Elevation Translocation-2 (TET2) Isocitrate Dehydrogenase (IDH) Nullizygosity for JAK2 46/1 haplotype Low JAK2V617F Increased plasma IL8, IL10, IL15 and IL2R No affect on survival or leukemic transformation in PMF Poor survival xx xx xx xx xx Treatment Options -Erythropoiesis stimulating agents -Corticosteroids -Androgen -Danazol -Thalidomide -Lenalidomide -Hydroxyurea -Cladribine -Splenectomy -Radiotherapy -Allogeneic SCT -Ruxolitinib -Pomalidomide -Other investigations agents (ATP mimetics, histone deacetylase inhibitors, hypomethylating agents, bevacizumab) JAK Inhibitors/Phase I INCB018424 was associated with clinical benefits in patients with advanced myelofibrosis. A starting dose of 15 mg twice daily with individualized dose adjustment was found to be the most effective and safest dose . These durable improvements (median follow-up, >1 year) were independent of JAK2 mutational status or the cause of disease. The reduction in splenomegaly observed in most patients was not predicted, and it occurred without deterioration in hematologic variables or tumor-cell lysis Phase III/ Ruxolitinib Controlled Myelofibrosis Study With Oral JAK Inhibitor Treatment I COMFORT I COMFORT I Randomized, double-blind, placebo-controlled Phase III study in patients with MF. 9/09- 4/10. 89 sites in US, Australia and Canada. Adults with PMF, post PV myelofibrosis, post ET myelofibrosis. Intermediate -2 or high risk. ECOG 3 or less. <10% peripheral blasts. Palpable spleen. Refractory, non-candidate or intolerant to available therapies. 309 patients: 155 assigned to ruxolitinib (15 mg BID if PLT<200 or 20 mg BID if PLT>200). 154 received placebo. Median follow-up 48 weeks. COMFORT I Primary endpoint Proportion of subjects achieving >35% reduction in spleen volume from baseline to Week 24 as measured by MRI or CT Secondary endpoints Duration of the reduction from baseline in spleen volume. Proportion of subjects with >50% reduction in total symptom score from baseline to Week 24 as measured by the modified MFSAF. Overall survival. COMFORT I Results: The primary endpoint response rate was 41.9% vs 0.7% ( p<0.0001). Mean reduction in spleen volume was 31.6% (8.1% increase in placebo). In 67% of those achieving at least 35% decrease in size, this was maintained into for 48 weeks or more. At least 50%symptom improvement at 24 weeks: 45.9% vs 5.3%. (mean improvement with ruxolitinib was 46.1% compared to mean worsening of 41.8%). 13 deaths in ruxolitinib group (8.4%)vs 24 in placebo (15.6%) HR 0.5 COMFORT I COMFORT I COMFORT I JAK2 V617F +ve JAK2 V617F –ve Mean change in spleen volume -34.6% -23.8 Change in symptom score -52.6% -28.1% COMFORT I Other facts: Among patients in whom the study drug was interrupted, symptoms returned to baseline over about a week. 2 patients in ruxolitinib group developed AML. Reduction of JAK2V617F allele burden: 10.9% at week 24 and 21.5% at week 48. Reduction in plasma levels of CRP and proinflammatory cytokines (TNFα and IL-6) COMFORT II COMFORT II • 219 patients. Randomized, open-label Phase III study of ruxolitinib vs best available therapy in patients with MF. Primary endpoint: Proportion of subjects achieving >35% reduction in spleen volume from baseline to Week 48 as measured by MRI Secondary endpoints : Leukemia-free survival Overall survival Progression-free survival Proportion of subjects achieving a >35% reduction of spleen volume from baseline to Week 24 as measured by MRI Duration of maintenance of a >35% reduction from baseline in spleen volume . Change in bone marrow histomorphology COMFORT II The wk 24 response rate was 31.9% vs 0% (P < .0001). The wk 48 response rate was 28.5% vs 0% (P < .0001). Median duration of response to ruxolitinib was 48 wks. No histopathologic change. No change in survival. The most common (> 20%) adverse events (AEs) of any grade : – thrombocytopenia (44.5% vs 9.6%) – anemia (40.4% vs 12.3%) – diarrhea (24.0% vs 11.0%) – peripheral edema (21.9% vs 26.0%). JAK inhibitors V617F located outside the ATP-binding pocket of JAK2 enzyme. – JAK inhibitors are not likely to distinguish between wild-type and mutant JAK2 enzymes. – Myelosuppression is an expected side effect if administered at doses that aim to completely inhibit the mutant JAK2 enzyme. Control proliferation Not elimination of mutant clones. JAK3 inhibition need to be minimized, as that will result in severe immune suppression Clinical trials are focused on patients with MF Comments The drug was originally designed to be a selective anticlonal effect but turned out, in an unexpected way, to be primarily an anticytokine drug. The drug didn’t show histopathologic, cytogenic, or molecular remissions. it will never be curative and can only be palliative. No evidence of survival over best available therapy (COMFORT II). The survival advantage over placebo (COMFORT I) could be due to withholding best available therapy. This remains to be seen in longer follow ups and further studies. JAK2 Take Home points JAKs are non-receptor protein tyrosine kinases that mediate signal transduction in pathways that regulate cell growth and cell survival. Myelofibrosis is associated with deregulated JAK signaling, via JAK2 mutations Receptor mutations (eg, MPL mutations) Increased JAK1 signaling Excess cytokines Damaged intracellular signaling mechanisms (those involving SOCS) Patients with myelofibrosis have deregulated JAK signaling regardless of JAK2 V617F mutational status. -JAK2 V617F is present in 50% to 60% of myelofibrosis patients. Ruxolitinib: Adverse events included: -Thrombocytopenia. -Anemia. -A “cytokine rebound reaction” on drug discontinuation. Characterized by acute relapse of symptoms and splenomegaly, sometimes necessitating hospitalization. In a recent publication, 2 patients (1.3%) were reported to have experienced a systemic inflammatory response syndrome on drug discontinuation. Using a tapering schedule and using steroid helps patient to tolerate this rebound reaction. The drug’s effect on JAK2V617F allele burden or bone marrow pathology was negligible, but a major reduction in proinflammatory cytokines (eg, IL1RA, IL-6, tumor necrosis factor-alpha, macrophage-inflammatory protein1f3) was documented and coincided with improvement in constitutional symptoms. Revlimid: -For patients with del 5q -Can be used with or without Prednisone -Approximately 20% response rate in PMF associated anemia, thrombocytopenia and splenomegaly -Longer use develops Neuropathy Hydroxyurea: -Helps in decreasing size of PMF related in splenomegaly. -In patients with >10cm spleen size nearly 35% patients had approximately 25% reduction in size and 17% had 50% reduction in size. -JAK2V617F negative patients showed lower response rate. -Duration of response around 1 year -Common side effects included Xerodermia, myelosuppression and mucocutaneous ulcer Splenectomy Indications: >10cm in size and not responding to Hydrea >Needing frequent PRBC transfusion > Portal HTN > Severe low platelet count > Profound Cachexia Drawback: <Peri-operative mortality is 5-50% and morbidity 25% <Abdominal Vein thrombosis <Hepatic enzyme elevation and hepatic failure as splenectomy removes major site of EMH. Using Hydrea to decrease platelet count <200,000 before splenectomy to reduce chance of thrombosis. Needs anticoagulation 1 month post-op. No evidence based literature to support laparoscopic total or sub-total splenectomy and splenic artery embolization. Radiotherapy: Most helpful in non-hepatosplenic EMH, especially -To control pulmonary hypertension -Lower and upper extremity pain Allogeneic SCT: Only treatment option in PMF that can induce complete hematologic, cytogenetic and molecular remission (except patients with del 5q treated with revlimid) UK study (Three-year OS 44% for CIC transplantation and 31% for RIC transplantation; relapse rates were 15% and 46%, non-relapse mortality rates were 41% and 32%, and extensive chronic GVHD rates were 30% and 35%) Not justified in patients with DIPPS score low or intermediate 1 category considering mortality and morbidity involved Even RIC (reduced intensity conditioning) transplantation does not significantly change mortality and morbidity compared to CIC (conventional intensity conditioning) CIC is preferred if patient’s age <40-50 and with high and intermediate risk 2 categories Immune-modulators: -Thalidomide, Lenalidomide and Pomalidomide -Antagonize angiogenesis, TNF alpha and IL6 -Facilitate production of IL2 and IFN gamma -Induce T cell and natural killer cell proliferation and activity -Decrease cytokine If del 5q Positive Negative Use Lenalidomide Jak2 +/+ and no splenomegaly Pomalidomide Negative, Thal/Pred References: How I treat myelofibrosis, Ayalew Tefferi. Division of Hematology, Department of Medicine, Mayo Clinic, Rochester, MN, Prepublished online January 3, 2011 doi:10.1182/blood-2010-11-315614 Management of Myelofibrosis, Alessandro M. Vannucchi, Section of Hematology, University of Florence, Italy Janus Reveals Another Face: The Biologic Rationale for Targeting Janus Kinase 2 in Lymphoma, Ann Mullally and Benjamin L. Ebert, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA JAK inhibitors for myeloproliferative neoplasms: clarifying facts from myths, Ayalew Tefferi, Division of Hematology, Department of Medicine, Mayo Clinic, Rochester, MN, (Blood. 2012;119(12):2721-2730) New prognostic scoring system for primary myelofibrosis based on a study of the InternationalWorking Group for Myelofibrosis Research and Treatment Francisco Cervantes et al, (Blood. 2009;113: 2895-2901) Genetic and Epigenetic Complexity in Myeloproliferative Neoplasms, Nicholas C. P. Cross, Faculty of Medicine, University of Southampton, and Wessex Regional Genetics Laboratory, Salisbury, United Kingdom. A Double-Blind, Placebo-Controlled Trial of Ruxolitinib for Myelofibrosis, Srdan Verstovsek, M.D., Ph.D et al, N Engl J Med 2012; 366:799-807. Uptodate Other materials: Images from JCO, Blood and open access web materials. Thank You, Questions?