Sutures, Needles, and Wound Care Techniques Lisa M. Campeau, M.D.
advertisement

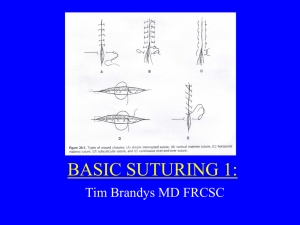
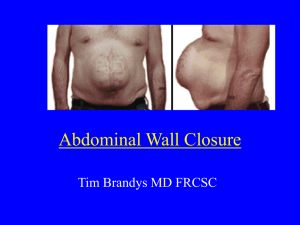
Sutures, Needles, and Wound Care Techniques Lisa M. Campeau, M.D. LSU School of Medicine Critical Concepts 2014-2015 Wound Care Intro ● Goals of Wound Closure – Obliterate dead space ie subcutaneous closure – Even distribution of tension along deep suture lines – Maintain tensile strength across the wound until tissue strength is adequate – Approximate and evert epithelium – Maximize cosmetic results!!! This is often the most important factor to the patient. Symmetry is the key to cosmesis Potential Complications ● Hypertrophic scar ● Wide or deep scar ● ● ● Keloid – more a patient factor than a closure factor Wound dehiscence Infection – important to use sterile field and aseptic technique due to the fact that you are actually implanting a foreign body ie suture Factors Contributing to Complications ● ● ● Patient Factors – Poor nutritional status – Diabetes – Poor skin quality High Tension Across Wound – Inadequate subcutaneous closure – Poor suturing technique Poor Suture Selection – Too small to support tension across wound Sutures ● 3 Basic Classes – Collagen – Absorbable – natural or synthetic, monofilament or braided – Non-absorbable – natural or synthetic, monofilament or braided Collagen Sutures ● Gut Sutures– Plain and Chromic – Plain gut has adequate tensile strength for 710 days and is gone in 70 days – Chromic gut maintains strength for 10-14 days and is resorbed in 90 days – May be used for repair around lips when rapid dissolution and no suture removal is preferred Absorbable Sutures ● ● Naturals – Degraded by enzymatic reaction of tissue resulting in moderate tissue reaction to presence of suture – gut sutures=collagen sutures Synthetics – Degraded by hydrolysis resulting in significantly less tissue reaction – Vicryl (braided), PDS, Maxon, Dexon, Monocryl (all 4 monofilaments) Non-absorbable Sutures ● ● Naturals – Moderate tissue reaction results in encapsulation – Silk & Cotton (braided), Stainless Steel (monofilament) Synthetics – Minimal tissue reaction in the skin over the sort term – Nylon & Prolene (monofilament), Ethibond (braided) Monofilament versus Braided ● ● Monofilament ie Nylon & Prolene (syn/nonabs), Steel (natl/nonabs), PDS, Maxon, Dexon, Monocryl (syn/abs), Gut (natl abs) – Decreased bacterial penetration – Low resistance through tissue – Will crush and fracture if clamped Braided ie Silk & Steel (natl nonabs), Ethibond (syn nonabs), Vicryl (syn/abs) – Increased tensile Strength – Pliable and flexible – Absorbs fluid and bacteria more Suture Sizes ● Size is a matter of diameter and is denoted in zeroes ● The more zeroes, the smaller the diameter ● #1>0>2-0>3-0>4-0>5-0>6-0>7-0 ● Size is directly related to tensile strength so use larger suture for wounds requiring more tension to close (If you have to pull really hard, you’re likely to break your suture. Get a bigger one and consider changing your closure technique!) Suture Selection ● Smallest to “Git ‘er done!” – which means to accomplish a tension-free closure – What tensile strength is required? – Suture caliber that is too small for the job can cut through skin, cause the wound to dehisce, or result in a wide scar Special Considerations ● Mobility – ● Skin Thickness – ● Thinner needs smaller caliber but be careful in thin elderly skin Cosmesis – ● Will require more tensile strength Smaller caliber suture/smaller diameter needle Risk of Infection – Use a monofilament and minimize tension Alternate Closure Techniques ● Staples ● Steristrips –especially with an adhesive ie mastisol or benzoin ● Dermabond – strength is equivalent to 5-0 mylon – Limited to 4-5 cm incisions – Can not get in the wound – Not for wounds with high infection risks, stellate margins, muco-cutaneous borders, or high tension Intro to Needles ● ● ● ● ● Needles are stainless steel alloys Wound closure and healing are affected by the initial tissue injury caused by needle penetration and suture passage Want smallest diameter needle to pass suture through the tissue Stable in the needle driver/holder Sharp enough to penetrate tissue with minimal resistance Anatomy of a Needle ● ● ● ● Point – From the tip to the max cross-section of the body Body – Interacts with driver, transmits penetrating force to the point Swage – Allows continuous unit with suture. May allow “pop-off” effect. Is thickest part of the needle Needle Coating -- Silicon Point Types ● Taper – Round point which passes by stretch rather than cutting tissue ● Conventional cutting –Point is triangular. Apex engages tissue first. ● Reverse cutting -- Triangular point but base engages tissue first. ● Beveled – Angle of cutting edge is decreased resulting in sharper point ● Blunt – Rounded point to dissect through friable tissue by pressure Needle Holders ● ● ● Stability in the holder affects performance of the needle Jaws must be right size to hold needle securely and prevent rocking/twisting/turning without affecting needle curvature Handle must be right for the depth of the job to be done Loading the Holder ● ● ● ● Important for the function of the needle and the driver Grasp needle ½ to ¾ of the way from its tip Angle needle 30 degrees toward tip of driver to allow full 360 degrees of needle tip movement Tighten driver to first ratchet – more only if necessary Improper Needle Placement ● Can Result In – Bent needle – Difficult skin penetration – Poor angle of tissue entry – Unpredictable path of needle thru tissue – Increased tissue trauma – Tissue loss from cutting needles – Suture pull-through – Asymmetric wound closure Instrument Use ● Ring finger and thumb in the holes ● Stabilize with the index finger ● ● ● Pick the right forceps to minimize tissue trauma and grasp to the needle Toothed forceps cause less tissue crush ie Adsons Un-toothed forceps may grasp the needle better ie Browns Skin And Its Tension Lines ● ● ● The majority of wound closure occurs in or just below the dermis You may have to close layers starting at the fascial level to eliminate dead space and minimize tension Don't forget the check skin tension lines in the area of interest Facial Lacerations ● VERY IMPORTANT TO REVIEW TENSION LINES TO INSURE MOST COSMETIC CLOSURE Lips ● Line up the mucocutaneous border as well as the wet-dry mucosal border Eyebrows ● ● Another critical area to line up borders Be very cautious of using epinephrine in your local anesthetic in the setting of: – Wound flaps – Thin skin – Fingers and toes Suturing Techniques ● Simple Interrupted ● Simple Running aka Whip stitch ● Locking Running aka Baseball ● Vertical Mattress – interrupted only ● ● Horizontal Mattress – interrupted or running Running Subcuticular Simple Interrupted Disadvantages ● Traverses full thickness of dermis ● Sides symmetric in depth, width, spacing – Requires more time to close ● Easy to place – ● Greater tensile strength Cross-hatching so remove sutures as early as possible ● Low wound edema so less impaired microcirculation ● Easier to adjust wound ● ● Ideally wider at base than apex to compress tissue upward which promotes edge eversion and limits risk of depressed scar Simple Interrupted ● ● ● ● ● Can adjust asymmetry in wound by varying distance of needle insertion and depth of bite Large bites decrease tension Small bites coapt precisely Close subcutaneous layers to obliterate dead space and decrease tension Invert knots if close to the surface Simple Running Closure ● Needs to be even in spacing and tension ● Knots only at either end min scar ● Can close long wounds quickly after easing tension with deep sutures ● Less scarring – good for loose skin ● Can use spaced simple interrupted stitches to off-set tension at the surface level Risks of simple running closure Dehiscence of wound if suture ruptures Puckering of thin skin and hypertrophic scarring Difficulty in fine adjustments to wound Locking Running Suture ● Accomplished by passing needle through suture loop at each pass ● Increased tensile strength ● ● Minimizes wound oozing but impairs microcirculation so can cause wound edge strangulation Good for the scalp which tends to bleed Vertical Mattress Closure ● ● ● Variation on simple interrupted 1 throw wide and deep/1 throw shallow and narrow Change the width based on the wound tension ● Maximal wound eversion ● Decreases dead space ● Decreases tension across wound Vertical Mattress Closure ● Tends to cross-hatch so remove sutures as early as possible ● Can decrease cross-hatching with bolsters between suture and skin ● Other versions include pulley stitch and far-near, near-far in high tension areas for tissue expansion Horizontal Mattress Closure ● For high tension areas to get maximal eversion ● Can be used to augment other closure ie simple running ● Likely to leave suture mark scars ● Can be placed prior to an excision to facilitate skin expansion ● Risk of strangulation if tied too tight ● Half-buried version possible The Corner Stitch ● A suture directly at the tip can cause ischemia and necrosis ● The corner stitch passes horizontally in the dermis or subq of the tip ● Allows advancement of the flap then the legs of the laceration are closed in any fashion Running Mattress Closures ● ● The horizontal mattress closure may be used in a running fashion if tension is not too high across the wound This allows for a faster, well everted closure but does limit ability to adjust the wound Running Subcuticular Closure ● Can use nonabsorbable or absorbable suture ● Removal of nonabs can be uncomfortable ● Best cosmetic results ● Wound needs to have minimal tension prior to epidermal closure ● Most commonly used closure in uncontaminated wounds Knot Tying ● – Instrument Ties – Used in cutaneous work – 2 turns on first pass is a Surgeon’s Knot – To square properly must be laid down perfectly parallel to previous throw or knot will slip – May help to leave small loop after 2nd throw to avoid strangulation One-handed Ties/Two-handed Ties The “Aberdeen Hitch” Method for tying a running surface stitch Involves sliding the held free end of the suture thru a loop twice then pulling it all the way thru the loop The knot can then be inverted on an intact suture Suture Removal ● ● ● ● ● Timing depends on anatomic location of wound closure Can range from 3 days to 2-3 weeks Too early – wide scars and wound dehiscence Too late – suture scars, infection, tissue reaction, difficult suture removal Augmented by use of steri-strips after suture removal Suture Removal Technique ● Elevate the knot and cut on the side that was buried ● Pull suture out toward the wound to avoid spreading immature scar ● Try to pull minimal contaminated suture through the skin ● Consider adhesive and steri-strips especially if removing suture early to minimize scarring Special Considerations ● ● Approaching the wounded patient Stop the bleeding with direct pressure if possible ● ● ● ● ● Provide pain relief as soon as appropriate H & P– rapid survey – Allergies to local anesthetics – Tetanus recently – Detailed exam of injured area ● ● Is the patient in the “golden period” for wound closure? What is the “golden period”? Does the pt require general anesthesia for wound treatment? Will extensive irrigation (pulsevac) or debridement be required? Will the area be difficult to numb? The Procedure ● ● Sterile field and aseptic technique are critical Irrigate wound with syringe and catheter to provide some pressure ● Consider dilute iodine or hibiclens ● Beware the vasovagal response!!! ● Line up landmarks first Local Anesthetics ● Lidocaine ranges from 0.5%-2% with 500 mg max ● Bupivicaine (marcaine) max 300mg ● Mepivicaine (carbocaine) max 300mg ● Add NaHCO3 to lido to neutralize ph ● ● ● ● Add epinephrine to increase duration of action, hemostasis, and decrease systemic absorption Be careful with adding epi in cardiac pts Work as much thru the open wound as possible if not overly contaminated Work thru anesthetized field – start proximal Healing by Secondary Intention ● ● Reasons to leave a wound open – Necrosis or infection – Slow healing, granulation bed, pre-existing scar Other options – Skin grafting – Normal saline packing – Wound-vac therapy Wound heals slowly by granulation formation, wound contraction (which can be significant despite the size of the wound), and re-epithelialization. Any area that fails to epithelialize can be grafted.