Developmental Disorders: What they are; why test, what to test for Isabelle Rapin
advertisement

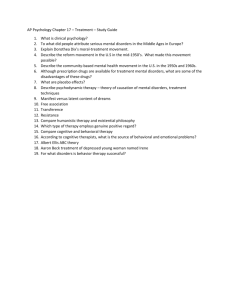
Developmental Disorders: What they are; why test, what to test for Isabelle Rapin Child Neurology, Sept. 11, 2013 No conflict of interest AIM OF THE SEMINARS Prevalent reason for child neurology office consult → deepen your knowledge beyond pushing pills (boring !) Showcase their neural basis Help you interpret test & other reports Prepare you to inform/educate parents and therapists Make the consult more effective 1 2 What are developmental disorders ? Unexpected deficits in the acquisition of specific learned skills Reflect atypical development of some but not all circuitry in the immature brain uneven skills Prevalent, with major impacts on children’s and their families’ lives and society 1 3 Examples of developmental disorders Developmental language disorders Dyslexia, problems with other academic skills Attention deficit disorders with/without hyperactivity Autism spectrum disorders Inept acquisition of motor skills Tone deafness Etc… 1 4 Develomental disorders: Conventional Clinical Diagnostic Criteria Not due to *major brain malformation, disease, trauma, epilepsy, identified genetic disorder, etc. lack of opportunity, e.g., environmental or social deprivation, poor teaching global intellectual disability medication effect etc. *Controversial view ! Stay tuned… 1 5 Nature of DSM behavioral “diagnoses” • They are behavioral syndromes Defined by clusters of behaviors/symptoms • Behavioral DSM “diagnoses” are pseudo- dichotomous, but needed ! • Keep this in mind when speaking with biologic investigators researching their causes and pathophysiologies • But the real world requires dichotomies for resource allocation, school placement, etc. !! 1 6 Genes to behavior 1. BEHAVIORAL DOMAIN/LEVEL ― - descriptive, observational continuous range of severity, i.e., distance from a population norm 2. BIOLOGIC DOMAIN/LEVEL ― dichotomous, discrete, yes/no (despite some gene mutations having dimensional effects) 1 7 Diagnosis: Fundamental classification issues 2 distinct domains → 1. behavior, 2. biology 3 distinct levels → A. Behavior = classification B. Pathophysiology = mechanisms C. Etiologies = classification 1 8 Hierarchies: genes to behavior A. BEHAVIOR – COMPLEX, MAINLY DESCRIPTIVE Living, behaving whole person – many behaviors B. PATHOPHYSIOLOGY, BIOLOGIC MECHANISMS 1. Brain – molecules, cells, networks 2. Cells – molecules, networks 3. Molecules - networks C. ETIOLOGY, BIOLOGIC CAUSES 1. Genetics 2. Environment 3. Both (incl. epigenetics) 1 9 Endophenotypes Specific components of complex behaviors/ observations Examples: perfect pitch, atypical head growth, hand stereotypies, shyness, etc. May run in “unaffected” family members → suggest an underlying gene(s)/CNV* Correlated gene/CNV does not “cause” a behavioral trait, much less clinical diagnosis ! *CNV=copy number variation, i.e., dup or del of numbers of bases 1 10 Genes Genes do not program behaviors ! Cellular metabolic microcircuitry Brain Brain networks program behaviors Anatomo-physiologic networks Behaviors CAVEAT ! 1 11 Contentious issues • Do specific etiologies, e.g., Down syndrome, previous meningitis, Fra-X, etc. exclude the diagnosis of autism, or dyslexia ? • Is it likely that “idiopathic” XYZ is “pure” ? • What do we mean by co-morbidity ? What do multiple “diagnoses” imply ? Does ADHD exclude an ASD diagnosis ? 1 12 Level A - Behavioral “Diagnoses” (data on behaving persons) Clinical observations (written reports) - behavioral observations, scales, etc. Standardized (quantitative) tests of function - questionnaires (history, observations) - psychologic/neuropsychologic tests - language, standardized observations, etc. Computerized tests (ADHD, faces, etc.) Photos, videos, recordings Etc. 1 13 Level A “diagnoses” = behavioral syndromes Dimensional, not yes/no binary Bell-shaped distribution of scores Fuzzy overlapping margins • Between syndromes • Between syndromes and “normality” 1 14 Overlapping behaviorally defined syndromes One brain ! Etc. OCD Autism Tourette MR ADHD Learning disability, dysphasia, dyslexia, etc. 1 15 Level B – Pathophysiology = hierarchy of mechanisms 1. 2. 3. Brain networks, connectivity between many participant cortical/subcortical neuronal nodes Cellular networks, e.g., glial/neuronal, excitatory/inhibitory, etc Molecular networks, gene products within/between cells 1 16 Differentially methylated RORA & other genes (blue) affecting processes/disorders differentially expressed by DNA micro-arrays (yellow) (Courtesy V.W. Hu, 2011) RORA = retinoic acid-related orphan receptor-alpha 1 17 Overlaps of genes in pathways controlling CNS development or function and other signaling pathways (Courtesy V.W. Hu 2010) 1 18 Level B clinical tests – Goal: document pathophysiology (not etiology) of behavioral diagnosis 1. 2. 3. 4. 5. Brain imaging (morphometry, fMRI, PET, etc.) EEG, other electrophysiologic tests Blood and urine tests Neurotransmitter, metabolite levels; other cellular gene products/correlates Etc. 1 19 Level C - ETIOLOGIES GENETICS (nuclear, mitochondrial – inherited, de novo* ) ENVIRONMENT (e.g., infection, intoxication…) GENETICS + ENVIRONMENT (epigenetic) UNKNOWN – true of most cases today *parents not arriers, but affected proband transmits if reproduces ! 1 20 Epigenetics Heritable changes in gene activation without alteration of its DNA sequence Modification of histone shape Cytosine methylation (CpG sites) Role in development & life-long (MZ twins) Environmentally influenced, e.g., Toxins, cancer… 1 21 Level C - GENETIC TESTS (discrete etiologies !) Genetic loci (identified in family trees) Chromosomal anomalies – number, cytogenetics: deletions, duplications, translocations, copy number variations (CNVs), etc. Single gene mutations, deletions, trinucleotide repeats, etc. with major/minor effects – GWAS (genome-wide association studies) Gene sequencing – identify specific mutation Epigenetic effects (± environmental) 1 22 Level C - GENETIC ETIOLOGIES Clinical tests Genetic tests (including microarrays [GWAS*, chips] CNVs, genes) Molecular gene products (~ proteins, enzymes, receptors, etc.) Etc. Indications: see Michelson et al report – Neurology 2011; 77:1629. *GWAS=genome-wide association study=micro-array 1 23 Goals of neurologic evaluation Role of the child neurologist 1 24 Neurologist’s responsibility Determine whether an actual disorder is likely What kind? What probable cause? What to do about it • Systemic, overtly neurologic? Needs medical Rx? • Behavioral/developmental/psychiatric? • What tests may be needed? Referrals needed? • Problem not significant. Advise how to handle • Likely to be biologically treatable? • Requires behavioral/educational intervention? 1 25 Office visit Watch child play with appropriate toys while… (advantage: warm up) History/family history/review records Screening mental status Screening neurologic exam Undressed screening general physical Preliminary impression 1 26 Decide on need for tests Hard core disease/lesion likely? Epilepsy? work-up accordingly Learning disability? Need further evaluation/management? Behavioral issues? Need further evaluation/management, medication? Need to determine biologic etiology? 1 27 Goals of tests in the clinic - 1 Targeted: no algorithm applies to all ! 1. Clinical & behavioral (neuropsychologic) tests For clinical diagnosis of the disorder To plan specific educational remediation To guesstimate prognosis For formal funded research 1 28 Goals of tests in the clinic - 2 Targeted: no algorithm applies to all ! 2. Biologic tests (genetic, imaging, EEG, etc.) Not for “diagnosis” of the clinical disorder, e.g., ADHD, ASD To discover the biologic etiology and pathophysiology Perhaps provide genetic counseling, etc. For formal funded research 1 29 Neurologic tests Imaging and electrophysiology: not indicated if no suspicion of a hard core neurologic condition/lesion, e.g., epilepsy Uninformative in isolated developmental disorders Not diagnostic of developmental disorders Expensive, stressful 1 30 Referral for etiologic/biologic/ genetic testing Indicated if + FH or exam or severe case What is the goal of the test if not? • Direct benefit to child – very rarely • Benefit to family – genetic counseling ?? psychologic, financial? To physician/geneticist – curiosity, career advancement, etc. • Research? 1 31 Benefits for research BE CLEAR ABOUT GOAL AND WHO PAYS ! • If more testing than clinically indicated, must be paid for by research funds • Not fair to charge to family, clinical insurance, Medicaid, etc. • Engage family as collaborators in research • Special IRB permission required for research. Discuss goals, that specimens, videos (special permission needed for teaching, publishing), that biologic specimens and test results, etc. will be anonymized and retained for later research 32 1 Problems with micro-arrays (gwas) Widely desired & recommended, but… Data ~ not interpretable more testing False positives/negatives Child not consulted, e.g., Huntington May discover non-paternity, adoption etc. Relatives not consulted, e.g. re cancer risk Who pays? Money better spent otherwise? 1 33 Targeted mental status screen: Goal: need for referral ? After warm-up, how does child respond to parent, to you? Able to talk on a topic? What does he/she do? need for ageappropriate toys, books, etc. in the office ! Level of activity, anxiety, compliance At preschool: 1 inch blocks, drawing, counting, naming colors, etc. At schoolage: reading, writing, simple math Mood, inappropriate behaviors or speech? 1 34 Goals of Behavioral Testing Provide a clinical diagnosis services Assess overall competence (IQ as surrogate for severity of the brain dysfunction) Identify specific deficit(s) to be addressed educationally 1 35 Referral for behavior/psychologic testing Omnibus IQ needed, but not predictive < age 10 yrs; surrogate for overall severity of brain dysfunction Test hearing & language when speech unclear/absent/bizarre, or comprehension poor Neuropsychologic testing: very useful for planning remediation in complex cases, but expensive and not universally needed Consider autism spectrum disorder when atypical behaviors, language, repetitive behaviors, etc. 1 36 Management Child neurologist’s responsibility 1 37 Summarize consult Severity/type of problem Findings, test results Lack of evidence for “disease” Developmental, likely genetic cause Probable outcome What to do/not to do, guidance on child rearing Consider whether medication needed Schedule follow-up visit to review Send written report to parents 1 38 Goals of management Accomodation, not cure Acceptance by self, family, peers Adequate function within limitations Avoidance of detrimental secondary “ “ consequences for child of parental guilt of shopping for ineffective Rx 1 39 Focused psychotropic medications Symptomatic, not curative Focus on most troublesome behavior/symptom, e.g, sleep, epilepsy, self-injury, aggressiveness, etc. First: adequate trial of behavioral treatments Stimulants (methylphenidate) may be very helpful in ADHD, even when cause known Risperidone: approved for ASD to mitigate aggressiveness and irritability. Potential permanent side-effects Too many psychotropic drugs prescribed Avoid medication cocktails 1 40 Summary Main etiology: genetics (+ environment) Diagnosis: behavioral, not biologic No direct jump from genetics to behavior No routine biologic testing, including micro-arrays Be honest about purpose of tests (clinical vs. research vs. looking good on rounds, etc.) Most effective intervention is targeted education, not pills 1 41 Flies in the ointment Too much to do in one hour ! Many insurances don’t pay child neurologists (but do developmental pediatricians…) Don’t know as much about interventions as developmental pediatricians Yet can often wrap up the most comprehensive consult, including genetics, need/no need for tests, brain basis, etc. 1 42