Lecture 4-214.ppt
advertisement

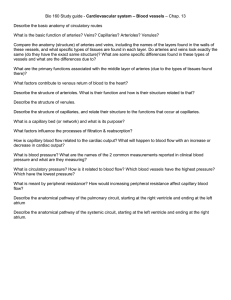
Cardiovascular System Blood Vessels Anatomy of Blood Vessels Arteries carry blood from the heart to the tissues Anatomy of Blood Vessels Arterioles are small arteries that connect to capillaries Anatomy of Blood Vessels Capillaries are the site of substance exchange between the blood and body tissues Anatomy of Blood Vessels Venules connect capillaries to larger veins Anatomy of Blood Vessels Veins convey blood from the tissues back to the heart. Arteries 1. 2. 3. Tunica interna (intima) – innermost Tunica media – middle layer Tunica externa – outer layer Tunica Intima 1. 2. Composed of; simple squamous epithelium (endothelium) Internal elastic membrane Tunica Media Rich in smooth muscle and elastic fibers Tunica Media Maintains elasticity and contractility Tunica Externa Rich in elastic and collagen fibers Functional Properties of Arteries 1. 2. Elasticity Contractility Elasticity Due to the elastic tissue in the tunica intima and media Elasticity Allows arteries to accept blood under great pressure from the contraction of the ventricles Contractility Due to the smooth muscle in the tunica media Contractility Allows arteries to increase or decrease lumen size Contractility Sympathetic stimulation of alpha 1 receptors on cutaneous arteries causes vasoconstriction Contractility Sympathetic stimulation of beta 2 receptors on arteries supplying skeletal muscle causes vasodilation Elastic Arteries Elastic Arteries – Large arteries with more elastic fibers and less smooth muscle Elastic Arteries Example: aorta, sublcavian, and pulmonary arteries Elastic Arteries Also called conducting arteries because they conduct blood from the heart to medium sized arteries Muscular or distributing arteries Medium sized and have a large amount of smooth muscle and distribute blood to various parts of the body Muscular or distributing arteries Examples: brachial, femoral, and popliteal arteries Arterioles Very small arteries that deliver blood to capillaries Capillaries Connect arterioles and venules Capillaries Microcirculation – flow of blood through the capillaries Capillaries Capillaries are found near almost every cell in the body Capillaries Function – Permit the exchange of nutrients and wastes between the blood and tissue cells Capillaries Composed of a single layer of cells (endothelium) and a basement membrane Capillaries 1. 2. Two types; Continuous Fenestrated Capillaries Continuous – composed of endothelial cells that form a continuous tube that contains gaps between cells called intercellular clefts Capillaries Fenestrated capillaries – plasma membrane contains small pores Capillaries Materials can cross the blood capillary walls in four ways Capillaries Four Ways; 1. Intercellular clefts 2. Trancytosis using pinocytic vesicles 3. Diffusion 4. Fenestrations Intercellular clefts Open in response to histamine (released during inflamation) making capillaries more leaky Intercellular clefts This allows fluid and wbc, and antibodies to go from the bloodstream to the site of infection Pinocytosis Large fats cross via pinocytosis Diffusion Water, CO2, and O2 cross capillaries by diffusion Fenestrations Allow small molecules such as water and electrolytes to get into the urine Fenestrations Prevent large proteins and red cells from getting into the urine Sinusoids Discontinuous capillaries Sinusoids Present in the liver Sinusoids Allow large molecules such as protein and bilirubin to get from the bloodstream into hepatocytes Venules They are small vessels that are formed from the union of several capillaries Venules Merges to form veins Venules Drain blood from capillaries into veins Veins Contain 60% of our blood volume Veins Consist of the same three tunics as arteries Veins Have a thinner tunica intima and media Veins Thicker tunica externa Veins Thinner walled than arteries due to less elastic tissue and smooth muscle Veins Low pressure systems Veins Contain valves to prevent backflow Veins Squeezing of the veins by muscles and inspiration promote venous return Venous Return The volume of blood returning back to the heart from the systemic veins Veins Vascular sinuses – veins with very thin walls with no smooth muscle to alter their diameter Example: Coronary sinus Anastomoses Union of the branches of two or more arteries supplying the same region Anastomoses Provide alternate routes for blood to reach a tissue or organ Anastomoses Collateral circulation is the alternate flow of blood to a body part through an anastomosis Anastomoses What is the importance of arteries that anastomose? Anastomoses Occlusion of an end artery interrupts the blood supply to a whole segment of an organ, producing necrosis of that segment Blood Pressure Pressure exerted on the walls of a blood vessel Blood Pressure In a clinical sense, it refers to pressure in arteries Blood Pressure BP=CO X TPR Blood Pressure Systolic and Diastolic fluctuations in the pressure are only seen in the arteries and arterioles Systolic Pressure Peak pressure in the arteries with each cardiac cycle during ventricular contraction Systolic Pressure Due to the stroke volume being ejected into the aorta Diastolic Pressure Lowest pressure in the arteries with each cardiac cycle Diastolic Pressure Force of blood recorded during ventricular relaxation Blood Pressure Young adult male = 120/80 mm Hg (8-10 mm Hg less in a young adult female) Resistance 1. 2. 3. Depends on three variables; Blood viscosity Vessel length Blood Vessel Radius Blood Viscosity Increased viscosity increases resistance Vessel length Increased length increases resistance Blood Vessel Radius Increased radius decreases resistance Systemic vascular resistance Total peripheral resistance (TPR) Systemic vascular resistance All of the vascular resistance offered by systemic blood vessels Mean Arterial Pressure MAP = Diastolic Pressure X 1/3(systolic pressure – diastolic pressure) Mean Arterial Pressure MAP = CO X TPR Mean Arterial Pressure Factors that increase BP increase SV increase HR constrict the blood vessels (increases resistance) Mean Arterial Pressure Factors that decrease BP Decrease CO Dilate the arteries Cardiovascular Center A group of neurons in the medulla that regulate heart rate, contractility, and blood vessel diameter Cardiovascular Center CV receives input from higher brain regions and sensory receptors (baroreceptors and chemoreceptors) Cardiovascular Center Sympathetic impulses along cardioaccelerator nerves increase heart rate and contractility Cardiovascular Center Parasympathetic impulse along vagus nerves decrease heart rate Cardiovascular Center The sympathetic division also continually sends impulses to smooth muscle in blood vessel walls via vasomoter nerves resulting in a moderate state of tonic vasoconstriction Neural Regulation of Blood Pressure Baroreceptors Chemoreceptors Baroreceptors Pressure-sensitive sensory neurons that monitor stretching of the walls of blood vessels Baroreceptors If blood pressure falls, the baroreceptor reflexes; accelerate heart rate increase force of contraction promote vasoconstriction Baroreceptors If pressure increases above normal, the reflexes cause; decrease in sympathetic tone increase in parasympathetic tone Hormonal Regulation Renin leads to the formation of angiotensin II Hormonal Regulation 1. 2. Angiotensin II causes; Vasoconstriction Secretion of aldosterone, which leads to sodium and water retention Hormonal Regulation Epinephrine and norepinephrine increase CO and cause vasoconstriction Hormonal Regulation ADH causes water retention and a little vasoconstriction Hormonal Regulation Nitric oxide from the endothelial cells causes vasodilation Hormonal Regulation Cortisol keep our arteries sensitive to vasoconstricting hormones Shock Is an inadequate CO that results in failure of the CV system to deliver adequate amounts of O2 and nutrients to meet the metabolic needs of body cells Shock Could result in; dysfunction of cellular membranes abnormal cellular metabolism cellular death Types of Shock 5 main types Hypovolemic Shock Due to decreased blood volume Cardiogenic Shock Due to poor heart function Vascular Shock Due to inappropriate vasodilation Obstructive Shock Due to obstruction of blood flow Neurogenic shock Due to decreased sympathetic outflow Homeostatic Response Activation of renin-angiotensin-aldosterone system Homeostatic Response Secretion of ADH Homeostatic Response Activation of the sympathetic division of the ANS Circulatory Routes Systemic Pulmonary Hepatic Portal Fetal Hepatic Portal Circulation Collects blood from the veins of the pancreas, spleen, stomach, intestines and gallbladder and directs it into the hepatic portal vein of the liver before it returns to the heart Hepatic Portal Circulation Enables nutrient utilization and blood detoxification by the liver