Automated Reticulocyte Analysis
advertisement

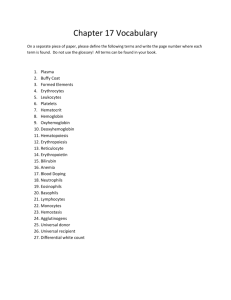
Automated Reticulocyte Analysis: New Parameters for Anemia Diagnosis and Therapeutic Monitoring & Improved Precision & Laboratory Efficiency Bruce H. Davis, M.D. William Beaumont Hospital Royal Oak, Michigan Automated Hematology: Desirable New Parameters • CD4 and CD8 Lymphocyte Subsets • Reticulocytes with immature reticulocyte maturation (IRF) - alias RMI • Neutrophil activation marker, such as quantitative PMN CD64 expression • reticulated platelets • Platelet activation markers (eg. CD62 or CD41 expression) • Hb F containing RBC enumeration (Kleihauer-Bettke) • Immune activation profile (cytokine/chemokine Rs) • CD5+ B Cells or light chain+ B cells (CLL, etc.)) • Stem Cell enumeration (CD34+ cells) History of Automated Reticulocyte Counting • 1980-90 Flow cytometric methods – – – – Tanke: Pyronin Y - Jacobberger: DiOC(3) Ortho: Acridine Orange - Others: PI, ethidium Br Metzger, Corash: Thioflavin T Lee (BDIS), Davis & Bigelow: Thiazole Orange • 1990: TOA Sysmex R instruments: Auramine O • 1992-96: Hematology instruments light scatter – Technicon - H3: Oxazine 750 – Coulter Gen-S, STKS & MAXM: NMB – Abbott Cell Dyn 3500: NMB • 1996: Hematology instruments - fluorescence – Abbott Cell Dyn 4000: thiazole-like dye – Coulter Gen-S: CPO dye Automated Reticulocyte Counting: Methods Available - 1997 Fluoresence Methods Light Scatter Methods • Thiazole Orange (BD) by Flow Cytometry • CPO dye (Coulter) by flow cytometry • TOA Sysmex R series and SE-Avante by Auramine O • Abbott Cell-Dyn 4000 by CD4K530 • ABX Vega by thiazole orange • Bayer Technicon H3, Advia by oxazine dye • Coulter STKS/MAXM and Gen-S with new methylene blue (NMB) • Abbott Cell-Dyn 3500 with NMB Advantages of Automated Reticulocyte Analysis •Amenable to labor efficiencies or robotics –faster analysis per sample –allows for batch analysis or random access •Improved precision of retic counting –superior to visual microscopic counts –greater objectivity •New parameters of erythropoiesis –Immature Reticulocyte Fraction (IRF) –Reticulocyte hemoglobin content New Parameters with Automated Reticulocyte Analysis •Immature Reticulocyte Fraction (IRF) •Reflects rate of erythropoietic activity •Available on many instruments, methods •Formerly termed reticulocyte maturity index (RMI) •Replaces need for “corrected” reticulocyte count •Reticulocyte MCHC (hypochromic Retics) •Detects early functional iron deficiency in Epo Studies by Brugnaro, d’Onofrio •Available only on Technicon H3 to date Reticulocyte Enumeration with Immature Reticulocyte Fraction (IRF) • IRF measured as fraction (0.00 - 1.00 range) • Sysmex R: IRF = HFR + MFR (Ref Range: 0.05-0.20) • Thiazole Orange: Cursor at 95% interval (Ref Range: 0.2-0.5) • Report with reticulocyte % and absolute count • Graphic display of retic count vs. IRF • Superimpose refernce ranges for anemia classification • Plotting sequential samples shows erythroid response • Report results with other CBC parameters • Flags for increased reticulocytosis and hypoproliferative response • Automated, random access, discrete testing 4 Immature Reticulocyte Fraction (IRF) Thiazole Orange by Flow Cytometry Reticulocytes RBCs IRF – exclude nucleated cells (nRBCs, PMNS, lymphs) – exclude platelets – define IRF region – define retics 10 2 FSC-Height --> 10 3 10 • IRF = #HFR/#Retics • Data Analysis Nucleated Cells 10 1 Platelets 10 1 10 2 10 Thiazole Orange --> 3 10 4 Evidence for Pathophysiologic Relevance of Immature Reticulocyte Fraction (IRF) • Erythropoietin therapeutic effect: IRF 1- 3 days – CD71 vs TO studies – BJH study, Major et al. • Animal models – in vivo biotinylation studies – CD71 vs. TO studies • BMT recovery – IRF earliest parameter of engraftment – various methods with demonstrated efficacy 1 Erythroid Maturation 0.9 0.8 Normal Erythopoiesis 0.7 0.6 Nucleated 0.5 Glycophorin 0.4 CD71 (TfR) 0.3 RNA Hemoglobin 0.2 Erythrocyte Reticulocyte, late Reticulocyte, IRF Normoblast, late Erythroblast 0 Normoblast, early 0.1 • Maturational continuum • EPO effect • blood retic populations – IRF retics (CD71+) – late retics – stress retics 10 4 10 4 Reticulocyte Maturation: in vivo biotinylation (K. Ault) 10 3 10 2 10 1 10 2 BIOTIN LEVEL --> 10 3 6 hours 10 1 BIOTIN LEVEL --> pre-biotinylation 10 1 10 2 10 3 10 1 10 4 10 2 3 10 4 10 4 10 4 10 4 THIAZOLE ORANGE --> 10 2 BIOTIN LEVEL --> 10 1 10 1 10 2 10 3 72 hours 10 3 24 hours BIOTIN LEVEL --> 10 THIAZOLE ORANGE --> 10 1 10 2 10 3 THIAZOLE ORANGE --> 10 4 10 1 10 2 10 3 THIAZOLE ORANGE --> Bone Marrow Regeneration Response: Consistent Pattern 0.5 Late Post Transplant Period Immature Reticulocyte Fraction 0.4 0.3 Early Period of Bone Marrow Recovery 0.2 Prior to Transplant 0.1 Ablation Period 0.0 0 20 40 60 80 Absolute Reticulocyte Count (10^9/L) 10 0 12 0 Erythroid Parameters with Erythropoietic Response Changes in Blood with Stimulated Erythropoiesis Hemoglobin Retic Count IRF 14 0.6 12 0.5 10 0.4 8 0.3 6 0.2 4 2 0.1 0 0 0 1 2 3 5 7 10 TIME (days) 14 21 30 45 Evaluation of Erythropoiesis: Bivariate IRF and Retic Count Display 0.8 Immature Reticulocyte Fraction (IRF) 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0.0 0 10 0 20 0 30 0 40 0 50 0 60 0 70 0 Absolute Reticulocyte Count (10^9/L) 80 0 90 0 10 00 Immature Reticulocyte Fraction (IRF): Clinical Utility in Medical Practice • Monitor BM or Stem Cell Regeneration post-BMT or ChemoRx • Monitor Renal Transplant Engraftment (Epo production) • Monitor Neonatal Transfusion Needs • Monitor Anemia Therapy • Monitor EPO Therapy: Renal Failure, AIDS, Infants, MDS • Monitor Bone Marrow Toxic Insults from drugs (eg. AZT) • Prognostic in Anemia of AIDS and Prematurity • Timing for Stem Cell Harvests following Growth Factor or Cytotoxic Drug Therapy • Detection of Aplastic Crisis in Hemolytic Anemias • Diagnosis and monitoring of aplastic anemia • Evaluate Normochromic Anemias of Various Etiologies • Detection of Occult or Compensated Hemorrhage or Hemolysis • Classification of Anemias Patterns of IRF and Retic counts in Anemia • • • • • • • • • • Clinical Condition Retic Ct IRF Aplastic anemia/crisis hypoplastic anemia BM regeneration Chronic disease Iron deficiency Thalassemia Folate/B12 deficiency Myelodysplasia Hemolytic anemia Blood loss/anoxia Low Low Low Low/WNL Low/WNL WNL/high Low/WNL Any level High WNL/high Low Low High/WNL WNL High WNL/high High WNL/high High High Intermethod Correlation Studies • Single site studies: multiple published – improved precision - CVs <15% – intermethod bias, but “clinically insignificant” • Davis et al: AJCP 102:468, 1994 – 8 sites, 11 instruments, 310 blood samples – IRF and Retic counts compared • College of American Pathologists’ Reticulocyte RT Survey 1994-96 – >2,600 participants – surrogate blood material – Retic % only reported Retic Counts: Inter-method Correlation Absolute Reticulocyte Count Absolute Reticulocyte Count 400 400 Sysmex R-3000 350 300 250 200 150 100 50 450 350 300 250 200 150 100 50 0 400 350 300 250 200 150 100 50 0 0 50 100 150 200 250 300 350 400 450 0 0 50 100 150 200 250 300 350 400 450 Abbott Cell Dyn 4000 0 Sysmex R-3000 Reticulocyte Percentage Reticulocyte Percentage 10 5 0 0 5 10 15 Abbott Cell Dyn 4000 20 20 Becton Dickinson FACScan Becton Dickinson FACScan 20 15 50 100 150 200 250 300 350 400 450 Abbott Cell Dyn 4000 Reticulocyte Percentage 20 Sysmex R-3000 Absolute Reticulocyte Count BD FACScan & Coulter STKS 450 BD FACScan &Coulter STKS 450 15 10 5 0 15 10 5 0 0 5 10 Sysm ex R-3000 15 20 0 5 Abbott Cell 10 Dyn 400015 20 IRF: Inter-method Correlation Immature Reticulocyte Fraction (IRF) 1 0.9 0.8 Sysmex R-3000 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0 0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 Abbott Cell Dyn 4000 0.8 0.9 1 Reticulocyte Proficiency Testing College of American Pathologists 1994-96 Program - surrogate blood material Methodologies Approved for Testing New Methylene Blue visual microscopy Sysmex R series (auramine O) Flow Cytometry - Thiazole Orange Flow Cytometry - Other dyes Coulter STKS/MAXM - NMB Miles Technicon H3 - Oxazine Flow Cytometry Sysmex R Miller Disc Technicon H-3 Manual STKS/MAXM NUMBER OF PARTICIPANTS CAP Survey 1995 RT-C: Distribution of Methods 12 50 10 00 75 0 50 0 25 0 0 1994-95 CAP RETICULOCYTE SURVEY 9 COULTE R X-L RE TI C% COULTE R EP I CSRETIC % 8 FAC SCANRET IC% M ILLERDI S C RE TI C% 7 STK S/ MAXM RET IC% SYS M EXR R ETI C% 6 TEC HNI C O NH- 3RETIC % 5 4 3 2 1 12 95RT-06 95RT-05 95RT-04 95RT-03 10 8 95RT-02 95RT-01 6 94RT-06 94RT-05 4 94RT-04 94RT-03 94RT-02 94RT-01 2 0 0 RETICULOCYTE PERCENT MA NUALRET IC% Coulter X-L Coulter Epics FACScan Manual Miller Disc STKS/MAXM Sysmex R Technicon H-3 1994-95 CAP RETICULOCYTE SURVEY Coulter X-L Coulter Epics FACScan Manual Miller Disc STKS/MAXM Sysmex R Technicon H-3 COULTE R EP I CSC. V. 40 COULTE R X-L C.V. FAC SCANC. V . MA NUALC. V . 35 M ILLERDI S C C.V. COEFFICIENT OF VARIATION STK S/ MAXM C. V . 30 SYS M EXR C . V. TEC HNI C O NH- 3C. V. 25 20 15 10 5 0 0 1 2 3 4 5 6 RETICULOCYTE PERCENT 7 8 9 CAP RT Survey Experience: No Bias with TO methods secondary to FCM instrument 11.0 R E T I C % A 11.0 10.0 10.0 9.0 9.0 8.0 8.0 7.0 5.0 R E T I C 4.0 % 6.0 7.0 6.0 5.0 4.0 3.0 3.0 2.0 2.0 R-1 1 R-2 2 R-3 3 R-4 4 R-6 5 R-5 6 Specimen SPECIMEN Number B A 6 6B KC KD Flow Cytometer INSTRUMENT PE PF Instrument G P Known or Potential Interferents •Cellular Elements –Platelet clumps or giant platelets –nucleated cells or fragments •RBC Inclusions –Howell-Jolly bodies –Heinz or Pappenheimer bodies –parasites (malaris, babesia) •Miscellaneous causes –Autoflourescence (drugs, porphyria) –RBC aggregation (paraproteins, cold agglutinins) –coincidence (eg. platelet and RBC) –abnormal RBCs, hemolysis Controls for Clinical Practice •Commericial Preparations –R&D Systems, Minneapolis, Mn –Streck Lab, Omaha, Ne –Instrument manufacturers •Refrigerated blood samples –short term QC by carry-over comparison –least expensive –will not detect long-term drift •Veterinary blood samples –rabbit –porcine Reasons for NOT utilizing automated reticulocyte counting • • • • • Volume does not exceed 3-5/day Physicians expect “stat” results Waiting for the “next generation” instrument “We’ve always done it this way” Technologists like doing manual counts