Chapter 26 - Fluid and Electrolyte Balance
advertisement

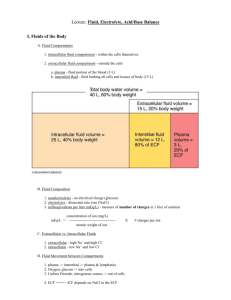
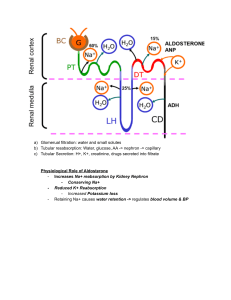
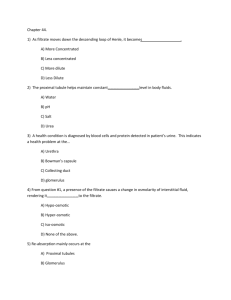
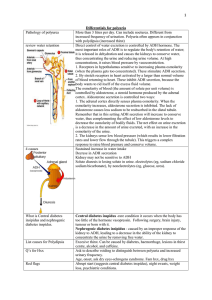
Lecture: Fluid, Electrolyte, Acid/Base Balance I. Fluids of the Body A. Fluid Compartments 1. intracellular fluid compartment - within the cells themselves 2. extracellular fluid compartment - outside the cells a. plasma - fluid portion of the blood (3 L) b. interstitial fluid - fluid bathing all cells and tissues of body (15 L) B. Fluid Composition 1. nonelectrolytes - no electrical charge (glucose) 2. electrolytes - dissociate into ions (NaCl) 3. milliequivalents per liter (mEq/L) - measure of number of charges in 1 liter of solution mEq/L = concentration of ion (mg/L) -------------------------------------atomic weight of ion C. Extracellular vs. Intracellular Fluids 1. extracellular - high Na+ and high Cl2. intracellular - low Na+ and low ClD. Fluid Movement between Compartments 1. plasma -> interstitial -> plasma & lymphatics 2. Oxygen, glucose -> into cells 3. Carbon Dioxide, nitrogenous wastes -> out of cells 4. ECF <===> ICF depends on NaCl in the ECF X # charges per ion II. Water Balance A. Overview of Water Balance 1. intake - 90% ingested water; 10% metabolic water 2. output - 60% urine; 28% lungs/skin; 12% sweat/feces 3. water need - trigger thirst & release of ADH B. The Thirst Mechanism decrease in plasma volume OR increase in osmolarity -----> excitation of hypothalamic thirst center -----> sensation of thirst C. Regulation of Water Output 1. obligatory water loss - lungs, sweat, feces 2. regulation of water - kidneys (ADH -> Na+) D. Disorders of Water Balance 1. dehydration - water loss > water intake a. bleeding, burns, sweating, diuretics 2. hypotonic hydration - too much water or Na+ 3. edema - accumulation of water in interstitial space III. Regulation of Sodium (Na+) Balance A. Sodium (Na+) - 90% of solutes in the ECF; most important and prevalent of all electrolytes B. Aldosterone - released by adrenal cortex (renin-angiotensin) 1. released in response to: a. decrease in blood pressure b. decreased osmolarity of filtrate c. sympathetic stimulation of juxtoglomerular cells 2. function - increase Na+ reabsorption at distal tubule a. water will follow if ADH makes the distal tubule permeable to water C. Baroreceptors 1. located in carotid arteries and aorta 2. respond to changes in stretch due to blood pressure a. blood pressure increases ------> hypothalamic stimulation ------> sympathetics to kidneys decrease ------> increased GFR (water removed) b. blood pressure decreases (same path as above) ----> ----> ----> lower GFR (water retained) D. Antidiuretic Hormone (ADH) 1. released from the posterior pituitary 2. responds to osmoreceptors in the hypothalamus a. decrease in osmo of ECF ------> decreased release of ADH ------> less permeability of distal tubule to water ------> more water released into urine b. increase in osmo of ECF ------> increased release of ADH ------> more permeability of distal tubule to water ------> less water released into urine E. Atrial Natriuretic Factor (ANF) 1. released by cell of heart atria under high B.P. 2. reduces blood pressure and blood volume by INHIBITING nearly all events that promote vasoconstriction and Na+/water retention." F. Steroid Hormones 1. estrogen - increases resorption of Na+ in distal convoluted tubule 2. glucocorticoids (cortisol) - increases resorption of Na+ in the distal tubules IV. Regulation of Potassium (K+) Balance A. Importance of K+ 1. K+ is primary CATION (+) in within cells 2. K+ abnormalities cause changes in Resting Mem Pot (neurons, cardiac muscle especially) B. Renal Control of K+ Levels 1. 10-15% constantly lost in urine 2. most resorption occurs in Proximal Tubule 3. regulation - changing amount SECRETED into urine in the collecting tubules a. low K+ ----> less secretion (intercalated cells in collecting tube can reabsorb more) b. high K+ ----> more secretion C. Factors Controlling K+ Secretion 1. tubule cell intracellular K+ level - when low, secrete less; when high, secrete more 2. aldosterone level - K+ secreted: Na+ reabsorbed a. increase aldosterone -> more K+ secretion b. decrease aldosterone -> less K+ secretion 3. pH - K+ and H+ compete for antiport with Na+ a. lower pH (high H+) -> less K+ secretion b. higher pH (low H+) -> more K+ secretion V. Regulation of Calcium (Ca++) Balance A. Importance of Ca++ 1. bone is the "reservoir" of most Ca++ in the form of Calcium Phosphate (Ca++ with PO4-2) 2. primary physiological roles (already covered): a. at the muscle and neuron synapse b. essential for blood clotting process c. very critical in heart rhythms B. Ca++ Regulation: Parathyroid Hormone (PTH) & Calcitonin 1. parathyroid hormone (PTH) – is secreted when Ca++ levels in blood get low a. bones - Ca++ and PO4-2 release to blood b. small intestine - activates Vitamin D which is essential for Ca++ resorption c. kidneys - Ca++ reabsorbed (but PO4-2 excreted) 2. calcitonin (thyroid gland) - released when Ca++ begins the INCREASE too high a. inhibits Ca++ release from bone, increases actual formation of Calcium Phosphate in bone