Chapter 26 Nontraumatic Musculoskeletal Disorders
advertisement

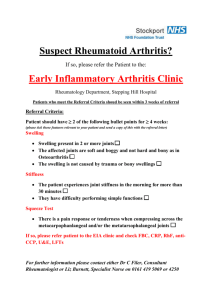
Chapter 26 Nontraumatic Musculoskeletal Disorders Copyright (c) The McGraw-Hill Companies, Inc. Permission required for reproduction or display. 26-1 Objectives 26-2 Review of the Musculoskeletal System 26-3 Anatomy and Physiology Review • Skeleton – Provides support for the body – Provides a frame for other parts of the musculoskeletal system to attach to 26-4 Anatomy and Physiology Review • Bones are living tissue – Collagen – Calcium 26-5 Anatomy and Physiology Review • Skeletal muscles – Move the skeleton – Produce the heat that helps maintain a constant body temperature – Maintain posture • Tendons • Ligaments 26-6 Anatomy and Physiology Review • Joints – Immovable (fibrous) joints – Cartilaginous joints – Synovial joints 26-7 Nontraumatic Musculoskeletal Conditions 26-8 Arthritis • Osteoarthritis – A chronic condition characterized by the breakdown of the joint’s cartilage – Commonly affects the hands, wrists, elbows, shoulders, spine, hips, knees, and ankles 26-9 Arthritis • Types of osteoarthritis – Primary osteoarthritis • Associated with aging • Cause is unknown – Secondary osteoarthritis • Caused by another disease or condition 26-10 Arthritis • Rheumatoid arthritis – Lining of the joints is inflamed – Initially • Pain, warmth, stiffness, redness, and swelling around the joint – In later stages of the disease • Affected joint becomes misaligned and loses its shape, limiting joint movement 26-11 Osteoporosis • Disease of progressive bone loss • Bones become weak and brittle due to loss of minerals in the bones • Common cause of fractures in women after menopause and older adults – Fracture = a break in a bone 26-12 Fibromyalgia • A disorder characterized by general fatigue and widespread musculoskeletal pain and stiffness • Most often develops during early and middle adulthood • Women are affected more often than men are. • Cause is not known 26-13 Fibromyalgia • Common assessment findings and symptoms – Musculoskeletal aches, – Bladder irritability pain and stiffness and spasms – Soft tissue tenderness – Painful menstruation – Depression and anxiety – General fatigue – Impaired concentration – Sleep disturbances – Problems with short and – Sensitivity to odors, long-term memory noises, bright lights, and touch – Headaches 26-14 Overuse Syndromes • Overuse syndromes are a group of conditions in which a part of the body is injured from repeated motions performed in the course of normal work or daily activities. 26-15 Overuse Syndromes • Common assessment findings and symptoms – Numbness – Decreased joint motion – Swelling – Burning – Pain – Aching – – – – – Redness Weakness Tingling Clumsiness Cracking or popping of joints 26-16 Carpal Tunnel Syndrome • Carpal tunnel • Median nerve compression – Pain, burning, tingling, weakness, or numbness 26-17 Wrist Tendonitis • Inflammation of one or more of the tendons around the wrist joint • Overuse can result in pain, tenderness, and swelling over the area of inflammation. 26-18 Tennis Elbow • Affects the tendons that attach to the bone on the lateral part of the elbow • Exact cause unknown • Overuse results in pain on the outside of the arm at the elbow joint 26-19 Golfer’s Elbow • Similar to tennis elbow but involves pain on the inside of the arm at the elbow joint • Pain is usually triggered when gripping an object 26-20 Snapping Hip Syndrome • Also called dancer’s hip • Audible noise and snapping sensation when the hip is moved from flexion to extension 26-21 Hip Bursitis • Pain and inflammation over the outside of the upper thigh • Usually occurs in middleaged or older adults • More common in women than men 26-22 Shin Splints • Medial tibial stress syndrome • Pain over the front of the tibia 26-23 Kneecap Bursitis • Swelling and pain on top of the kneecap • Limited motion of the knee 26-24 Achilles Tendonitis • Achilles tendon – Largest and strongest tendon in the body – Attaches muscles of the calf to heel bone – Used when walking, running, or jumping – Overuse typically results in pain over the back of the heel 26-25 Patient Assessment 26-26 Patient Assessment • Scene size-up and ensure your safety. • Perform a primary survey • Take the patient’s vital signs and gather the patient’s medical history. – Use OPQRST to identify the type and location of the patient’s pain. 26-27 Physical Examination • Use DCAP-BTLS to recall what to look and feel for during the physical exam: – Deformities – Contusions (bruises) – Abrasions (scrapes) – Punctures/penetrations – Burns – Tenderness – Lacerations (cuts) – Swelling 26-28 Physical Examination • Feel for deformities, tenderness, and swelling. • Feel and listen for crepitus. • Check the pulse, movement, and sensation in each extremity (PMS). – Assess the dorsalis pedis pulse (on top of the foot) in each lower extremity. – Assess the radial pulse in each upper extremity. – During your bilateral assessment, compare PMS findings (left vs right) 26-29 Physical Examination • Assess movement – Lower extremities – Upper extremities • Assess sensation – Lower extremities – Upper extremities 26-30 Emergency Care • In general, emergency care is supportive. • Take appropriate standard precautions. • Provide specific treatment based on the patient’s signs and symptoms. • Allow the patient to assume a position of comfort. • Maintain an open airway. Give oxygen if indicated. • Applying a splint may be indicated. • Transport and reassess as often as indicated. 26-31 Questions? 26-32