Sarcoidosis.ppt
advertisement

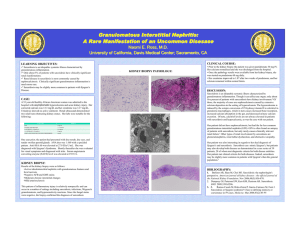
Sarcoidosis Dr.Adil Al Sulami KAUH Sarcoidosis is a multisystem inflammatory disease of unknown etiology that predominantly affects the lungs and intrathoracic lymph nodes. Sarcoidosis is manifested by the presence of noncaseating granulomas (NCGs) in affected organ tissues. The modern history of sarcoidosis In 1899, the pioneering Norwegian dermatologist Caesar Boeck describe skin nodules characterized by compact, sharply defined foci of "epithelioid cells with large pale nuclei and also a few giant cells . Thinking this resembled sarcoma, he called the condition "multiple benign sarcoid of the skin. Epidemiology All racial . All ethnic groups. All ages (with the incidence peaking at 20 to 39 years). M-F ratio 2:1. The incidence The highest annual incidence in northern European countries 5 - 40 / 100,000. In Japan, the annual incidence 1 - 2 / 100,000. Among black Americans is roughly 3 times that among white Americans (35.5 / 100,000, as compared with 10.9 / 100,000. Pathophysiology T cells play a central role in the development of sarcoidosis, as they likely propagate an excessive cellular immune reaction. The cause of sarcoidosis is unknown. Efforts to identify a possible infectious etiology have been unsuccessful. Genetic role. and environmental factors seem to play a As yet, no bacterial, fungal, or viral antigen has been consistently isolated from the sarcoidosis lesions. Sarcoidosis disease. is neither a malignant nor an autoimmune The following have been suggested as possible candidates that might play a role in causing sarcoidosis: Mycobacteria, such as Mycobacterium tuberculosis, and atypical pathogens have been suggested. Fungi and viruses, particularly Mycoplasma, Chlamydia, and EpsteinBarr virus, have been unconvincingly implicated. Environmental Causes Some of the earliest studies of sarcoidosis reported associations with exposures to irritants found in rural settings, such as emissions from wood-burning stoves and tree pollen. More recently, associations with sarcoidosis and exposure to inorganic particles ,insecticides ,and moldy environments have been reported. Occupational studies have shown positive associations with service in the U.S. Navy ,metalworking ,firefighting ,and the handling of building supplies. Genetic Features Familial sarcoidosis was first reported in 1923 in two affected sisters . No formal twin study has been reported, but the concordance appears to be higher in monozygotic twins than in dizygotic twins . In A Case-Control Study, patients with sarcoidosis stated 5 times as often as control subjects that they had siblings or parents with sarcoidosis. Common Clinical Features Presentation depends on the extent and severity of the organ involved. Approximately 5% of cases are asymptomatic and incidentally detected by CXR. Systemic symptoms occur in 45% of cases such as : Fever. anorexia Fatigue. Night sweats . Weight loss . Pulmonary, dyspnea on exertion, cough, chest pain, and hemoptysis (rare) occur in 50% of cases. Löfgren's syndrome, an acute presentation consisting of: Fever. Arthralgia. erythema nodosum. bilateral hilar adenopathy. occurs in 9 to 34% of patients . Heerford's syndrome : Anterior Uveitis Fever Parotid enlargment Facial palsy Physical finding Pulmonary findings. Dermatological manifestations. Ocular manifestations . Cardiac manifestations Neurologic manifestations (rare) Organ Involvement Sarcoidal granulomas can involve any organ, but in more than 90% of patients, clinical sarcoidosis is manifested as intrathoracic LN enlargement, pulmonary involvement, skin or ocular signs and symptoms, or some combination of these findings. Pulmonary Involvement dyspnea, cough, vague chest discomfort, and wheezing. Chest radiographs in patients with sarcoidosis have been classified into four stages: – – – – stage 1, bilateral hilar lymphadenopathy without infiltration. stage 2, bilateral hilar lymphadenopathy with infiltration. stage 3, infiltration alone. stage 4, fibrotic bands, bullae, hilar retraction, bronchiectasis, and diaphragmatic tenting. These so-called stages represent radiographic patterns and do not indicate disease chronicity or correlate with changes in pulmonary function. Stage 1 Stage II is BHL and infiltrates Stage III is infiltrates alone Cutaneous Involvement Although not life-threatening, but can be emotionally devastating. Erythema nodosum may occur. Lupus pernio is the most specific associated cutaneous lesion. Violaceous rash is often seen on the cheeks or nose. Osseous involvement may be present. Maculopapular plaques are possible. Lupus pernio is more common in women than in men and is associated with chronic disease and extrapulmonary involvement. Erythema nodosum occurs in about 10% of patients with sarcoidosis and usually lasts for about 3 weeks. Biopsy specimens of erythema nodosum lesions show nonspecific septal panniculitis, which neither confirms nor negates the diagnosis of sarcoidosis. Liver and Spleen Involvement 10% of all patients with sarcoidosis have elevated serum aminotransferase and alkaline phosphatase levels. A cholestatic syndrome characterized by pruritus and jaundice, hepatic failure, or portal hypertension can develop (liver involvement is usually clinically silent). Detection of hepatic and splenic lesions on CT is described in 5% and 15% of patients. 60% of patients with hepatic manifestations of sarcoidosis have constitutional symptoms such as fever, night sweats, anorexia, and weight loss. Portal hypertension with variceal bleeding, a hepatopulmonary syndrome with refractory hypoxemia, and cirrhosis leading to liver failure occur in only 1% of patients with sarcoidosis. Neurologic Involvement CNS is involved in up to 25% of patients with sarcoidosis who undergo autopsy, but only 10% of all patients with sarcoidosis present with neurologic symptoms. The most common problems: – – – – – – cranial-nerve palsies. Headache. Ataxia. cognitive dysfunction. Weakness. seizures. CSF Analysis : – nonspecific lymphocytic inflammation. – measuring ACE levels . – oligoclonal immunoglobulin bands in the CSF are elevated, making it difficult to differentiate sarcoidosis from multiple sclerosis. Magnetic resonance imaging (MRI) Ophthalmologic Complications The eye and adnexa are involved in 25 -80% of patients with sarcoidosis,this necessitating routine slit-lamp and funduscopic examination. Anterior or posterior granulomatous uveitis . Conjunctival lesions and scleral plaques may also be noted. Ocular involvement may lead to blindness if untreated. Anterior uveitis (is the most common manifestation) chronic anterior uveitis, with insidious symptoms leading to glaucoma and vision loss, is more common than acute anterior uveitis. Cardiac manifestations Heart failure from cardiomyopathy rarely occurs. Heart block and sudden death may occur. Approximately 25% of patients may have NCGs at autopsy, but fewer than 5% have clinical cardiac disease. Okada et al reported on cardiac infiltration associated with a novel heterogenous mutation (G481D in CARD15) in early-onset sarcoidosis. Differential Diagnosis Hilar infiltrates: Tuberculosis. Lymphoma Eosinophilic granuloma Fungal infection Lung cancer NCG on a biopsy : Berylliosis Catscratch disease Fungal infection Hypersensitivity pneumonitis Leprosy Primary biliary cirrhosis Tuberculosis. Diagnosis The diagnosis is established on the basis of : Clinical finding. Radiologic findings. Supported by histologic evidence in one or more organs of noncaseating epithelioid-cell granulomas in the absence of organisms or particles. A diagnosis of sarcoidosis is reasonably certain without biopsy in patients who present with Löfgren's syndrome. Laboratory Studies Routine lab evaluation often is unrevealing. Hypercalcemia or hypercalciuria may occur (NCGs secrete 1,25 vitamin D). Hypercalcemia is seen in about 10-13% of patients, whereas hypercalciuria is 3 times more common. An elevated alkaline phosphatase level suggests hepatic involvement. Angiotensin converting enzyme (ACE) levels may be elevated. NCGs secrete ACE, which may function as a cytokine. Serum ACE levels are elevated in 60% of patients at the time of diagnosis. Levels may be increased in fluid from bronchoalveolar lavage or in CSF. Sensitivity and specificity as a diagnostic test is limited (60 and 70%, respectively). There is no clear prognostic value. Serum ACE levels may decline in response to therapy. Decisions on treatment should not be based on the ACE level alone. Imaging Studies A chest radiograph is central to evaluation. Routine chest CT scan adds little. HRCT of the chest may be helpful. Biopsy specimen A biopsy specimen should be obtained from the involved organ that is most easily accessed, such as the skin, peripheral LN, lacrimal glands, or conjunctiva. If diagnosis requires pulmonary tissue, transbronchial biopsy by means of bronchoscopy has a diagnostic yield of at least 85% when multiple lung segments are sampled . The central histologic finding is the presence of NCGs with special stains negative for fungus and mycobacteria. Sarcoidal granulomas have no unique histologic features to differentiate them from other granulomas. Special stains for acid-fast bacilli and fungi, as well as cultures of such organisms, are essential. If the results of lung biopsy with bronchoscopy are negative and other organs are not obviously involved, biopsy of intrathoracic lymph nodes, which are often enlarged in patients with sarcoidosis ,may be necessary to confirm the diagnosis. Treatment Most patients (>75%) require only symptomatic therapy NSAID. Approximately 10% of patients need treatment for extrapulmonary disease. 15% of patients require treatment for persistent pulmonary disease. Corticosteroids are the mainstay of therapy prednisone given daily and then tapered over a 6-month course is adequate for pulmonary disease. Earlier recommendations suggested an initial dose of 1 mg/kg/d of prednisone; however, more recent expert opinions endorse a lower dose (eg, 40 mg/d), which is tapered to every other day long-term therapy over several weeks. Most patients who require long-term steroids can be treated using 10-15 mg of prednisone every other day. High-dose inhaled corticosteroids may be an option, but conclusive data are lacking. Data suggest that corticosteroid use may be associated with increased relapse rates. Occasionally, certain patients cannot tolerate or do not respond to corticosteroids. Noncorticosteroid agents Used more frequently. Common indications : Steroid-resistant disease. Intolerable adverse effects. patient desire not to take corticosteroids. Methotrexate (MTX) has been a successful alternative to prednisone and is a steroid-sparing agent. Chloroquine and hydroxychloroquine are antimalarial drugs with immunomodulating properties, which have been used for cutaneous lesions, hypercalcemia, neurological sarcoidosis, and bone lesions. Chloroquine has also been shown to be efficacious for the treatment and maintenance of chronic pulmonary sarcoidosis. Cyclophosphamide has been rarely used with modest success as a Azathioprine is another second-line therapy, which is best used as a Chlorambucil is an alkylating agent that may be beneficial in Cyclosporine is a fungal cyclic polypeptide with lymphocyte- steroid-sparing treatment in patients with refractory sarcoidosis. steroid-sparing agent rather than as a single-drug treatment for sarcoidosis. patients with progressive disease unresponsive to corticosteroids or when corticosteroids are contraindicated. suppressive properties that may be of limited benefit in skin sarcoidosis or in progressive sarcoid resistant to conventional therapy. Infliximab and thalidomide have been used for refractory sarcoidosis, particularly for cutaneous disease. Infliximab appears to be an effective treatment for patients with systemic manifestations such as lupus pernio, uveitis, hepatic sarcoidosis, and neurosarcoidosis. Tetracyclines have shown promise for the treatment of cutaneous sarcoidosis. For pulmonary disease Asymptomatic PFT and/or CXR abnormalities are not an indication for treatment. In patients with minimal symptoms, serial reevaluation is prudent. Significant respiratory symptoms associated with PFT and CXR abnormalities likely require therapy. For such patients, treatment is indicated if objective evidence of recent deterioration in lung function exists. Corticosteroids can result in small improvements in the functional vital capacity and in the radiographic appearance in patients with more severe stage II and III disease. One recent study demonstrated an approach that may minimize the use of corticosteroids without harming the patient. This is accomplished by Withholding therapy unless the patient shows at least a 15% decline in one spirometric measure associated with increasing symptoms or, if asymptomatic, withholding therapy unless the patient shows worsening PFTs and a change in CXR. For extrapulmonary sarcoidosis involving such critical organs as the heart, liver, eyes, kidneys, or central nervous system, corticosteroid therapy is indicated. Topical corticosteroids are effective for ocular disease. Inhaled corticosteroids are occasionally used, in particular in patients with endobronchial disease. NSAIDs are indicated for the treatment of arthralgias and other rheumatic complaints. Patients with stage I sarcoidosis often require only occasional treatment with NSAIDs. Follow-up Further Inpatient Care – Monitor pulmonary function and CXR every 6-12 months. – Assess for progression or resolution. – Determine if previously uninvolved organs have become affected. Further Outpatient Care – Annual slit lamp eye examination and ECG are recommended. Prognosis Many patients do not require therapy, and their conditions will spontaneously improve. Markers for a poor prognosis include : Advanced CXR stage. Extrapulmonary disease (predominantly cardiac and neurologic) Evidence of pulmonary hypertension. Multiple studies have demonstrated that the most important marker for prognosis is the initial CXR stage. Remission 2/3 of patients with sarcoidosis generally have a remission within a decade after diagnosis, with few or no consequences ;remission occurs for more than half of patients within 3 years . Unfortunately, up to 1/3 of patients have progressive disease, leading to clinically significant organ impairment. A recurrence after 1 or more years of remission is uncommon (affecting <5% of patients), but recurrent disease may develop at any age and in any organ. Death Less death than 5% of patients die from sarcoidosis. is usually the result of pulmonary fibrosis with respiratory failure or of cardiac or neurologic involvement .