Skeletal Muscle Diseases Lecture 49 Dr zeenat
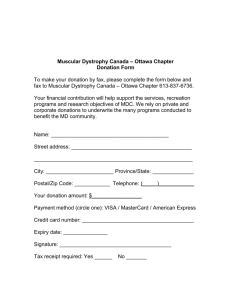
advertisement

Lecture 49 Skeletal Muscle Diseases Dr zeenat DR ZEENAT NASEER • HISTOPATHOLOGIST • College of Medicine • Majmaah Lecture Objectives • Enlist and classify muscular dystrophies. – Describe their pathogenesis – Describe their morphology – Discuss their clinical features and management. • Enlist common diseases of neuromuscular junctions. – Describe their pathogenesis. – Describe their morphology. – Describe their clinical features, diagnosis and complications. Classification • X-linked: • Duchenne muscular dystrophy (DMD) Most • Becker muscular dystrophy (BMD) Common • Emery-Dreifuss muscular dystrophy (EDMD) • Autosomal recessive: • Limb-girdle muscular dystrophy (LGMD) • Autosomal dominant: • • • • Less Facioscapulohumeral muscular dystrophy (FSHD) Common Distal muscular dystrophy Ocular muscular dystrophy Oculopharyngeal muscular dystrophy Reference: UpToDate, 2014 Pathogenesis Reference: UpToDate, 2014 Duchenne Muscular Dystrophy (DMD) Becker Muscular Dystrophy (BMD) Role of Dystrophin α2- chain Cytoplasmic actin Reference: Robbins Basic Pathology. 8th Ed. The relationship between the cell membrane (sarcolemma) and the sarcolemmal associated proteins. Dystrophin, an intracellular protein, forms an interface between the cytoskeletal proteins and a group of transmembrane proteins, the dystroglycans and the sarcoglycans. These transmembrane proteins interact with the ECM, including the laminin proteins. Mutations in dystrophin are associated with the X-linked muscular dystrophies, mutations in caveolin and the sarcoglycan proteins with the autosomal limb girdle muscular dystrophies, and mutations in the α2-laminin (merosin) with a form of congenital muscular dystrophy. • Histology is similar in DMD & BMD • Marked variation in muscle fiber size • Residual muscle fibers show a range of degenerative changes • Other fibers show regeneration • Connective tissue is increased throughout the muscle • Definitive diagnosis – abnormal immunohistochemical staining for dystrophin or by western blot of skeletal muscle Clinical Features References: -Robbins Basic Pathology. 8th Ed. -UpToDate, 2014 • Death due to: - Respiratory insufficiency - Pulmonary infection - Cardiac decompensation Management • Steroids – main treatment option • Vaccination to prevent Pneumonia & Influenza • Screening (by Echo/MRI) at around 6 years age, and treatment of Cardiomyopathy • Lung function testing at around 9-10 years age and assisted ventilation if needed • Periodic monitoring of Vitamin D levels & diet rich in Calcium & Vit D • Physical therapy, leg braces • Surgery for correction of contractures & scoliotic deformities Reference: UpToDate, 2014 Diseases of the Neuromuscular junction Myasthenia gravis • Pathogenesis Autoantibodies to AChRs (Acetylcholine Receptors) • Associated conditions Thymic hyperplasia (65%) Thymoma (15%) • Electrophysiologic studies decreased motor responses after repeated stimulation • Morphology Electron Microscopyloss of AChRs from region of synapse • Clinical features weakness starts in extraocular muscles or generalized clinical improvement with anticholinesterase drugs • Complication Respiratory compromise, no autonomic dysfunction Lambert-Eaton Myasthenic Syndrome • • • • • • Reference: Robbins & Cotran Pathologic Basis of Disease. 8th Ed. Pathogenesis Autoantibodies to presynaptic Calcium channels Associated conditions paraneoplastic process with Small cell lung carcinoma60% Electrophysiologic studies increased motor responses after repeated stimulation Morphology Electron Microscopynormal AChRs in region of synapse Clinical features weakness starts in proximal muscles no clinical improvement with anticholinesterase drugs Complication Autonomic dysfunction present Summary • Duchenne & Becker are the most common Muscular Dystrophies • Inheritance is X-linked recessive • Dystrophin, an important skeletal muscle intracellular protein, is either absent (DMD) or decreased (BMD) • Progressive weakness of the pelvic girdle followed by the shoulder girdle occurs; symptoms being less severe in BMD • Management mainly involves use of steroids along with good supportive course Summary • Myasthenia gravis & Lambert-Eaton Myasthenic Syndrome are the two main diseases of the Neuromuscular Junction; the former being differentiated from the latter by: – Presence of Autoantibodies to AChRs – No autonomic dysfunction – Decreased motor responses after repeated stimulation in Electrophysiologic studies – Clinical improvement with use of Anticholinesterase drugs Thank you