first part
advertisement

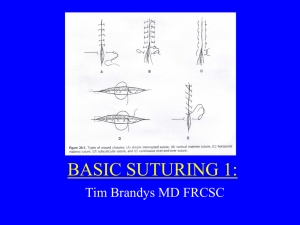
SUTURING TECHNIQUE BY Dr.zameer SUTURING TECHNIQUE INTRODUCTION: Closure of wound is one of the important aspects of any surgical procedure. It is also one aspect of surgery which is given least attention. The most common cause of post operative infection is poor surgical techniques usually related to devitalized tissue remaining in the wound or inadequate closure. Sutures and needles SUTURE: derived from sutura (Latin) means uniting edges of incision or wound by stitching. HISTORY: - oldest suture was placed by an embalmer on the belly of a mummy in Egypt in 1100 BC. - Hippocrates used the word suture ( meaning to ‘sew’ or ‘seam’ ) in 400 BC. - Galen in 2nd century : use of silk & hemp ligatures - Ambroise Pare’ ( 1510-1590 ) : substituted ligation of blood vessels to cauterization. - Physick ( 1806 ): developed absorbable ligatures using kid and buck skin. - Joseph Listen ( 1827-1921 ) : 1st to use disinfected suture material ( using carbolic acid ) . REQUISITES OF WOUND CLOSURE All osseous & soft tissue with severely compromised blood supply should be removed. Hemostasis should be obtained before each layer is closed & proper apposition should be ensured. Tension checked at each level. Subcutaneous layers adapted with absorbable sutures using interrupted sutures. Dead spaces should be obliterated. Loose ends of sutures trimmed to the knot to minimize amount of foreign material. INDICATIONS FOR SUTURING Sutures aid in healing. prevent contamination of wound. Prevent post operative bleeding. Prevent dislodgement of clot . Approximate tissues and facilitate primary healing. Prevent postoperative pain from exposed bone. Used to control or retract flaps. PRINCIPLES OF SUTURING Needle holder should grasp needle at 3/4 th of distance from cutting point. Needle should enter tissues perpendicularly. Needle should pass following curvature of the needle. Suture should pass at an equal distance of 2-3 mm from incision on both sides & at an equal depth. Distance between sutures should be 2-3 mm. Needle passed from free to fixed tissue. Needle passed from thinner to thicker tissue. Needle passed from deeper to superficial tissue. Distance the needle is passed into the tissue should be greater than the distance from tissue edge. Tissues should not be closed under tension. Knot should not be placed on the incision. Sutures should atleast be placed 2-3mm apart. MATERAILS USED IN SUTURING: 1. 2. 3. 4. 5. Needles. Suture material. Needle holder. Tissue holding forceps. Scissors. Proper suturing requires an understanding of the physical & biological properties of both needle & suture material. PLACEMENT OF NEEDLE IN TISSUE: 1. 2. 3. 4. 5. 6. 7. 8. 9. Ethicon(1985) gives following principles: Force should be applied in direction that follows curvature of needle. Pass from movable to non-movable tissue. Avoid excessive bites with small needles. Use sharp needles with minimal force. Grasp needle ¾ distance from the point. Never force needle through tissues. Avoid retrieving needle from tip, grasp the body. Sutures placed in keratinized tissues. Adequate tissue bite required to prevent tissue tearing. TISSUE ADHESIVES Based on epoxy resin: polyurethanes & cyanoacrylates. Epoxy resin gives high bond strength, but at low rate. Polyurethanes – good bond strength only in dry systems. Cyanoacrylates – moisture has minor effect on the reaction. - healing area indistinguishable from those of silk sutures. - margins may not merge properly. AUTOLOGOUS FIBRIN GLUE: Biological adhesive with fibrinogen, factor XIII , fibronectin , thrombin, apoprotein & CaCl2. Works as an adhesive by emulation of exudative phase of wound healing. Studies have demonstrated efficacy in stabilizing esophago-gastric, small intestinal & nerve anastomosis. Skin grafts also take up well ; sutures or pressure dressing - not required. Preparation of the glue – easy ; done with approx. 200ml of autologous blood from a single donor. FIBRIN SEAL ADHESIVE: 1. 2 component system ( Tissucol ) Derived from whole blood. Produces final pathway of coagulation. Still in experimental stage. Disadvantages: Possible transmission of AIDS & Hepatitis. CYANOACRYLATE: Used as tissue adhesive or hemostatic agent. Disadvantages: 1. Acts as barrier & prevents wound apposition. 2. Loosens over a period of time. MUSSEL ADHESIVE PROTEIN ( MAP ): Obatained from blue mussel “mytilus edulis”. Significant in attachment of tissue to metal. Disadvantage: 1. Causes artifacts on CAT images. 2. Possible Movement of metal sutures during MRI. SKIN TAPES: Introduced by Ambroise Pare’ Modern skin tapes are non occlusive & have excellent adhesive characteristics with viscous rayon fibres coated with adhesive copolymer. Advantages: 1. Puncture of skin surface is avoided. 2. Minimizes wound dehiscence. 3. May be reapplied to the wound. 1. 2. 1. 2. Uses: Used with sub cuticular sutures. Decreases tension on sutured skin in areas of motion Disadvantages: Does not evert wound edges. Loosened readily by blood or serum. METALLIC SUTURE MATERIALS: Stainless steel or tantalum wires used. Monofilament or braided. Strongest & most secure. Uses: 1. in scar revision in keloid forming patients 2. Suspension of splints or arch bars in maxillofacial surgeries. STAINLESS STEEL: 1. 2. 1. 2. 3. 1. 2. Advantages: One of the Strongest material. Least tissue reaction. Disadvantages: Very poor handling characteristics. Causes kinking & cutting through tissues. Fatigue & fracture occurs with time. Uses: Ligament, tendon & bone surgery. Circumzygomatic & circummandibular wiring. METALLIC STAPLES 1. 2. 3. 1908 – Humer Hultl Recent modification is introduction of absorbable staples ( Lactomer ) Examples of stapling instruments: TA instruments GIA instruments EEA instruments NEEDLE HOLDER Instrument with a locking handle & a short stout beak. Usually 6 inch needle holder recommended. Face of beak is cross hatched. Thumb & ring finger passed through the rings. Index finger held along length of needle holder & 2nd finger controls locking mechanism. TISSUE HOLDING FORCEPS . Used to stabilize soft tissue flaps during suturing. Adson forcep – most commonly used. Small delicate forceps with teeth are also used. SCISSORS Used in same way as needle holder. Have short cutting edges. Dean’s scissors – commonly used KNOT TYING 1. 2. 3. Holds the 2 ends of suture securely. Different suture materials require different knots. Usually placed on buccal side. 3 types of knots used in periodontal surgery : Square knot Surgeon’s knot Granny knot SQUARE KNOT: Done by placing 2 knots, each in opposite direction. 1st knot placed by passing the loop over the jaws of the needle holder & 2nd knot placed by passing loop under the needle holder. May loosen when synthetic or monofilament sutures are used. SURGEON’S KNOT: Modified square knot in which the 1st overhand knot is doubled. Last knot is placed in opposite direction. Used with synthetic or resorbable sutures. GRANNY(SLIP) KNOT: Similar to square knot but knots placed in same direction SUTURE METHOD 1. Interrupted suture : Most commonly used. Needle passed from one end of incised tissue margin & brought out from the other. This is then approximated & knot applied. Advantages: - strong & successive sutures may be placed to fit individual requirements. - each suture is independent of the next therefore loosening of one suture will not loosen other sutures. - eversion of tissue can be obtained by getting a deep bite. - preferred in areas of tension 2.Continuous suture: / RUNNING SIMPLE Provides rapid technique of closure. After passing through the tissue, suture is not cut but the needle is passed under the loop of the 1st suture in a continuous fashion. Advantages: - even distribution of tension. - provides more water tight closure. - Only 2 knots with associated tags Disadvantages If cut at one point, suture slackens along the whole length of the wound which will then gape open. 3.CONTINUOUS LOCKING/BLANKET Similar to continuous but locking provided by withdrawing the suture through its own loop. Indicated in long edentulous areas, tuberosities or retromolar area. Advantages -Will avoid multiple knots -Distributes tension uniformly -Water tight closure -Prevents excessive tightening. SUTURE REMOVAL When sutures are removed, the sutures should be grasped with an instrument & elevated above the tissue surface. Scissors used to cut one side of loop as close to the tissue as possible POSTOPERATIVE CARE Patient instructed to rinse frequently with saline. Wounds on lip & face should be cleansed with H 2 O 2