Systemic mycoses
advertisement

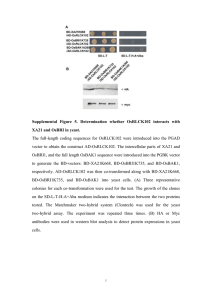
Systemic mycoses General characters 1) Fungi that cause systemic mycoses are: o Histoplasma capsulatum causing histoplasmosis. o Blastomyces dermatidis causing blastomycosis. o Paracoccidiodes brasiliensis causing paracoccidiodomycosis. o Coccidiodes immitis causing coccidiodomycosis. 2) All these fungi are DIMORPHIC: o In the soil or culture at 25 degree: hyphae with spores. o In the tissues or culture at 37 degree: yeast cells. 3) Infection by these fungi occurs as follows: o These fungi grow as hyphae in the soil. o They release spores into air. o These spores are inhaled by man. o Inside the human body: spores will grow as yeast cells. Epidemiology Infection by these fungi is restricted to certain areas in the world. So, SYSTEMIC mycoses is called ENDEMIC mycoses. Histoplasmosis and blastomycosis are endemic in vast areas that drain into Mississippi river. Paracoccidiodes brasiliensis is endemic in South America especially Brazil. Coccidiodes immitis is endemic in Southwestern USA (Arizona, New Mexico, South California) and North Mexico. Pathogenesis These fungi are acquired by inhalation of spores residing in the soil. (NO PERSON TO PERSON) Once inhaled, spores will grow as yeast cells that infect the lungs. Dissemination may occur. Histoplasma capsulatum (non capsulated ) grows in areas contaminated with birds & bats excreta. So, outbreaks of histoplasmosis occur during clearing chicken coops or spelunking. Blastomyces dermatidis is isolated from the soil and rotten wood. Clinical picture Asymptomatic: the majority of cases. Pneumonia: o Mild pneumonia with fever & coughing. Histoplasma lesions may heal with calcification of granuloma o A small percent will develop severe pneumonia. o A smaller percent will progress to chronic cavitary pneumonia. Disseminated lesion: occurs in immunodeficient patients. Spread occurs to: o o o o o Lung. CNS causing meningitis. Bone causing lytic lesions. Skin causing ulcers. Other organs. NOTE THAT Blastomycosis is the hardest to get & the hardest to have Blastomycosis is the rarest systemic infection. Mostly present as chronic disseminated disease. Blastomycosis Blastomycosis Skin lesions resulting from the dissemination of the fungus from the lungs Laboratory diagnosis Tissue is the issue Specimen: BIOPSY from the affected tissue. Direct microscopic examination of the tissue after staining with PAS (periodic Acid Schiff), silver to see the yeast phase. Culture on SDA at: At 25 degree: hyphae with characteristic spores. It converts to yeast after incubation at 37 degree. Serological diagnosis: detect the antibodies against fungi. The tests used are: o Complement fixation test. o Immunodiffusion test. Serological diagnosis of blastomycosis is not reliable because these antigens are: o Poorly defined. o Cross reactive with other fungi. PAS stain showing Histoplasma capsulatum yeast cells in liver specimen Histoplasma capsulatum Macroconidia and microconidia Rough-walled macroconidia Blastomycosis Tissue sections showing large, broad-base, unipolar budding yeast-like cells Blastomyces dermatitidis One-celled conidia formed on short conidiophores. Broad based budding and thickened cell walls and globose shape are characteristic of the yeast form of Blastomyces dermatitidis COCCIDIOIDOMYCOSIS Disease • Coccidioides immitis causes coccidioidomycosis. Properties • C. immitis is a dimorphic fungus that exists as a mold in soil and as a spherule in tissue Coccidioides immitis showing typical single-celled, hyaline, rectangular to barrel-shaped, alternate arthroconidia Transmission & Epidemiology Coccidioide The fungus is endemic in arid regions of the southwestern United States and Latin America. People who live in Central and Southern California, Arizona, New Mexico, Western Texas, and Northern Mexico. In soil, it forms hyphae with alternating arthrospores and empty cells. Arthrospores are very light and are carried by the wind. They can be inhaled and infect the lungs. Pathogenesis of Coccidioide In the lungs, arthrospores form spherules that are large, have a thick, doubly refractive wall, and are filled with endospores. Upon rupture of the wall, endospores are released and differentiate to form new spherules. The organism can spread within a person by direct extension or via the bloodstream. Granulomatous lesions can occur in virtually any organ but are found primarily in bones and the central nervous system (meningitis) Dissemination from the lungs to other organs occurs in people who have a defect in cell-mediated immunity. Pathogenesis of Coccidioide Most people who are infected by C. immitis develop a cell-mediated (delayed hypersensitivity) immune response that restricts the growth of the organism. One way to determine whether a person has produced adequate cell-mediated immunity to the organism is to do a skin test (see below). In general, a person who has a positive skin test reaction has developed sufficient immunity to prevent disseminated disease from occurring. If, at a later time, a person's cellular immunity is suppressed by drugs or disease, disseminated disease can occur. Clinical Findings of Coccidioide Infection of the lungs is often asymptomatic and is evident only by a positive skin test and the presence of antibodies. Some infected persons have an influenza like illness with fever and cough. About. 50% have changes in the lungs (infiltrates, adenopathy, or effusions) as seen on chest x-ray. 10% develop erythema nodosum (see below) or arthralgias. This syndrome is called "valley fever" or "desert rheumatism"; it tends to subside spontaneously. Disseminated disease can occur in almost any organ; the meninges, bone, and skin are important sites. Clinical Findings of Coccidioide The overall incidence of dissemination in persons infected with C. imrnitis is 1%, although the incidence in Filipinos and African Americans is 10 times higher. Women in the third trimester of pregnancy also have a markedly increased incidence of dissemination. Erythema nodosum (EN) manifests as red, tender nodules ("desert bumps") on extensor surfaces such as the shins. It is a delayed (cell-mediated) hypersensitivity response to fungal antigens and thus is an indicator of a good prognosis. Clinical Findings of Coccidioide There are no organisms in these lesions; they are not a sign of disseminated disease. EN is not specific for coccidioidomycosis; it occurs in other granulomatous diseases, eg, histoplasmosis, tuberculosis, and leprosy. In infected persons, skin tests with fungal extracts cause at least a 5mm induration 48 hours after injection (delayed hypersensitivity reaction). Skin tests become positive within 2-4 weeks of infection and remain so for years but are often negative in patients with disseminated disease. Coccidioidomycosis Tissue section showing typical endosporulating spherules of C. immitis Coccidioidomycosis Chronic cutaneous granulomatous lesions of the face, neck and chin Extension of pulmonary coccidioidomycosis showing a large superficial ulcerated lesion Laboratory Diagnosis of Coccidioide In tissue specimens, spherules are seen microscopically. Cultures on Sabouraud's agar incubated at 25 °C show hyphae with arthrospores (Caution: Cultures are highly infectious; precautions against inhaling arthrospores must be taken.) Laboratory Diagnosis of Coccidioide In serologic tests, [gM and IgG precipitins appear within 2-4 weeks of infection and then decline in subsequent months. Complement-fixing antibodies occur at low titer initially, but the titer rises greatly if dissemination occurs PARACOCCIDIOIDOMYCOSIS Paracoccidioides brasiliensis causes paracoccidioidomycosis, also known as South American blastomycosis. Properties of Paracoccidioides P. brasiliensis is a dimorphic fungus that exists as a mold in soil and as a yeast in tissue. The yeast is thick walled with multiple buds, in contrast to B. dermatidis, which has a single bud . Transmission & Epidemiology of Paracoccidioides The spores are inhaled, and early lesions occur in the lungs. Asymptomatic infection is common. Alternatively oral mucous membrane lesions, lymph node enlargement, and sometimes dissemination to many organs develop. Paracoccidioidomycosis Extensive destruction of facial features Ulcerated lesion on the pharyngeal mucosa Ulcerated lesion on the nasal mucosa Laboratory Diagnosis of Paracoccidioides In pus or tissues, yeast cells with multiple buds are seen microscopically. A specimen cultured for 2-4 weeks may grow typical organisms. Skin tests are rarely helpful. Serologic testing shows that when significant antibody titers (by immunodiffusion or complement fixation) are found, active disease is present. Paracoccidioidoes brasiliensis Multiple, narrow base, budding yeast cells "steering wheels" of P. brasiliensis Paracoccidioidoes brasiliensis Multiple, narrow base, budding yeast cells "steering wheels" of P. brasiliensis Summary Agent infection Dissemination Drug of choice Blastomyces dermatitidis Blastomycosis Skin and bone Later nervous system and visceral organs Amphotericin B itraconazole Coccidioides immitis Coccidioidomycosis Skin, bones, joints, subcutaneous tissues, and visceral organs Amphotericin B Paracoccidioidoes brasiliensis Paracoccidioidomycosis Oro-nasal mucosa latter spleen, liver, intestine and skin Amphotericin B + sulfas or azoles Histoplasma capsulatum Histoplasmosis Acute pneumonia (cave disease) Amphotericin B Chronic pneumonia (smoker) Disseminated (immunocompromised) Primary cutaneous (lab accidents) Systemic Mycoses PARACOCCIDIOIDES BLASTOMYCES HISTOPLASMA COCCIDIOIDE