cvs 1st lecture

Physical Therapy For
Cardiovascular
Disorders
DR. Mohamed Seyam PhD. PT.
Assistant Professor Of Physical Therapy For
Cardiovascular /Respiratory Disorder
Course Code : RHPT 482 Credit hours ( 2+1+0)
Objectives
What is the main purpose for this course?
This course provides the student with the required information about the techniques of application to treat various acute & chronic cardiac conditions.
Planning and managing the appropriate way of application of treatment for various cardiovascular disorders.
This course also serves to integrate the knowledge gained by the students in clinical cardiac conditions with the skills gained in exercise therapy, electrotherapy and massage, thus enabling them to apply these in clinical situations-of dysfunction due to pathology.
Normal Cardiovascular Anatomy & Physiology
1. Myocardial Oxygen Supply / Demand
2. Contractility
3. Electrical Conduction
4. Blood flow through heart
5. Coronary arteries
6. Blood vessels
The cardiovascular system
It is consists of the heart , which pumps blood throughout the body and the blood vessels , which are a closed network of tubes that transport the blood.
There are three types of blood vessels :
Arteries , which transport blood away from the heart;
Veins , which transport blood toward the heart;
Capillaries , which connect the arteries and veins, are the smallest of the blood vessels, and are where oxygen, nutrients, and wastes are exchanged within the tissues.
BLOOD VESSELS WALLS
The walls of the blood vessels consist of three layers or tunics:
1) tunica externa (adventitia)the outer connective tissue layer.
2) tunica mediathe middle smooth muscle layer (may also contain varying amounts of elastic fibers in medium and large arteries).
3) tunica intimathe inner endothelial lining of the blood vessels.
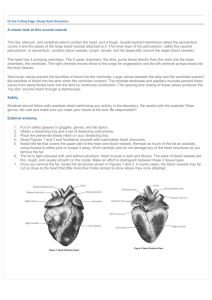
Heart
It is the pump which pushes blood into the circulation. It is formed of 2 sides, a. Right side: Right atrium and right ventricle.
b. Left side: Left atrium and left ventricle.
The tricuspid valve: It connects between the right atrium and right ventricle.
The mitral valve: It connects between the left atrium and left ventricle.
Shape of the heart: It is pyramidal shaped resting on one of its sides.
- The apex: It projects downward, forward and to the left.
- It is formed by the left ventricles.
- The base (posterior surface) of the heart:
- It is quadrilateral and directed posteriorly.
- It consists of the left atrium and small portion of the right atrium
♥
■
■
2 Atria:
Chambers of the Heart
♥
2 Ventricles:
Thin-walled chambers.
■ Thicker, muscular walls.
Receive blood returning to
Pump blood from heart.
heart.
■ Each has same capacity
& pumps same volume of blood in same time.
Valves of the Heart
♥
2 Atrioventricular (AV) valves:
■ One way valves.
■ Allow bl to flow from atria into ventricles.
■ Tricuspid (Rt) & Mitral (Lt).
♥
2 Semilunar valves :
■ One way valves.
■ At origin of pulmonary artery
& aorta.
■ Pulmonary (Rt) & Aortic (Lt).
■ Open during ventricular contraction.
Heart Walls: 3 Distinct Layers
1. Endocardium: the innermost layer of the heart.
2. Myocardium: the thickest main layer, consists of cardiac muscle.
3. Pericardium (epicardium): it is a fibroserous sac surrounding the heart and the roots of the great vessels.
And outer covering or external membrane around the heart.
Pericardium
It is a fibroserous sac surrounding the heart and the roots of the great vessels.
It consists of two components:
1. Fibrous pericardium: It is a tough connective tissue outer layer.
2. Serous pericardium: It is thin and consists of two layers:
Parietal layer: It lines the inner surface of the fibrous pericardium
Visceral layer: It form the layer covering the heart and greet vessels.
Pericardial cavity: It is narrow space created between the two layers of serous pericardium containing a small amount of fluid.
Types of circulation
1. Pulmonary circulation
2. Systemic circulation
Fetal Circulation
Fetal Circulation
•No circulation to lungs
•Foramen ovale
•Ductus arteriosum
•Circulation must go to placenta
•Umbilical aa., vv.
Arterial Supply Of The Heart
A. Right coronary artery : It originates from the right aortic sinus of the ascending aorta
It gives the following branches:
1) Atrial branch.
2) Sinu-atrial nodal branch.
3) Right marginal branch.
4) Right posterior descending artery branch (RPDA).
B. Left coronary artery: It originates from the left aortic sinus of the ascending aorta.
It gives the following branches:
1) Left anterior descending artery branch (LADA).
2) Circumflex branch.
3) Left marginal artery.
Heart Venous return
a. Coronary sinus: It receives the following tributaries:
1. Great cardiac vein :
It ascends in the anterior interventricular sulcus.
2. Middle cardiac vein :
It ascends in the posterior interventricular sulcus.
3. Small cardiac vein :
It begins in the coronary sulcus between the right atrium and right ventricle.
4. Posterior cardiac vein :
It lies on the posterior surface of the left ventricle just to the left of the middle cardiac vein.
b. Anterior cardiac veins:
They are small veins that arise on the anterior surface of the right ventricle.
c. Venae cordis minimae:
They are small veins draining directly into the cardiac chambers.
Regulation of the Heart
• Intrinsic regulation : Results from normal functional characteristics, not on neural or hormonal regulation
– Starling’s law of the heart
• Extrinsic regulation : Involves neural and hormonal control
– Parasympathetic stimulation
• Supplied by vagus nerve, decreases heart rate, acetylcholine secreted
– Sympathetic stimulation
• Supplied by cardiac nerves, increases heart rate and force of contraction, epinephrine and norepinephrine released
Nerve Supply Of The Heart
It is in medulla oblongata and it is supplied by sympathetic (cardiac nerves) and parasympathetic nerves (vagus nerve).
- Stimulation of the sympathetic system:
1. Increases heart rate.
2. Increases the force of contraction.
- Stimulation of the parasympathetic system:
1. Decreases heart rate.
2. Reduces force of contraction.
3. Constricts the coronary arteries
Heart Surface Anatomy
Surface anatomy of the heart is presented by
4 points.
A.
Point at the lower border of the left 2 nd costal cartilage.
B. Point at the upper border of the right 3 rd costal cartilage.
C. Point at the 5 th intercostal space near the midclavicular line represents the apex.
D. Point at the right 6 th costal cartilage.
- The upper border: It extends from A-B.
- The right border: It extends from B-D.
- The left border: It extends from A-C.
- The lower border: It extends from C-D.
B
D
A
C
Heart : Conducting Tissues
1. Sinoatrial (SA) node.
2. Internodal pathways.
3. Atrioventricular (AV) node.
4. Bundle of His.
5. Rt & Lt bundle branches.
6. Purkinje fibers.
7. This rhythmic sequence of events occurs an average of
72 times per minutes
Heart : Conducting Tissues
■ SA- node and to a lesser extent
AV- node contain small round cells called ‘ P cells ’ which are probably the actual pacemaker cells.
■ At AV- node, very small no. of intercalated discs & gap junctions
delay transmission of impulse.
SA node located in the right atrial wall, just inferior to the entrance of the superior vena cava.
The electrical impulses from SA node spread through the entire right and left atrial muscle mass, triggering contraction of the right and left atrium.
The impulses from S-A node travel to atrioventricular (A-V) node.
A-V node is located in lower end of the interatrial septum near the tricuspid valve.
Delay at A-V Node
Conduction speed in A-V node is slow (delay).
- This delay allows time for the atria to finish contraction and empty their contents into the ventricles before ventricles start to contract.
-
A-V node is the only normal route that impulses from SA node are transmitted into ventricles
.
Heart Sounds
• First heart sound or “lubb”
– Atrioventricular valves and surrounding fluid vibrations as valves close at beginning of ventricular systole
• Second heart sound or “dupp”
– Results from closure of aortic and pulmonary semilunar valves at beginning of ventricular diastole, lasts longer
• Third heart sound (occasional)
– Caused by turbulent blood flow into ventricles and detected near end of first one-third of diastole