Introduction to CVS
advertisement
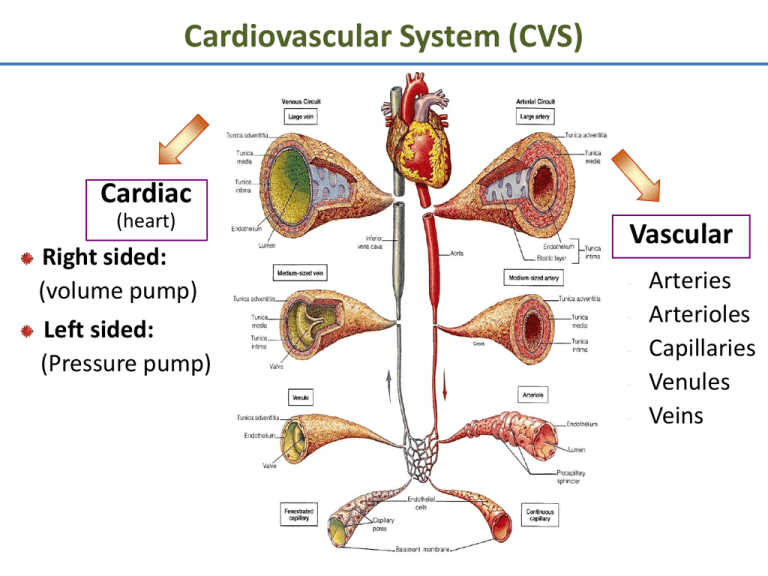
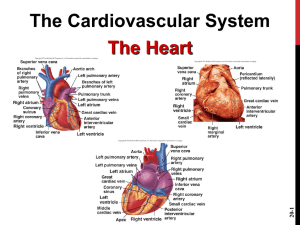
Cardiovascular System (CVS) Cardiac (heart) Right sided: (volume pump) Left sided: (Pressure pump) Vascular - Arteries Arterioles Capillaries Venules Veins Functions of Cardiovascular System I. Primary (main) Function of the Heart: ♥ Acts as a muscular pump: in order to maintain adequate level of blood flow throughout CVS by pumping blood under press into vascular system. ♥ Responsible for the mass movement of fluid in body. Functions of Cardiovascular System II. Secondary functions: 1. Transportation: • • • • Delivers O2 to tissues, & brings back CO2 to lungs. Carries absorbed digestion products to liver & tissues. Carries metabolic wastes to kidneys to be excreted. Distribution of body fluids. Functions of Cardiovascular System II. Secondary functions: 2. Regulation: • • • • Hormonal: carries hormones to target tissues to produce their effects. Immune: carries antibodies, leukocytes (WBCs), cytokines, & complement to aid body defense mechanism against pathogens. Protection: carries platelets, & clotting factors to aid protection of the body in blood clotting mechanism. Temperature: helps in regulation of body temperature, by diverting blood to cool or warm the body. Anatomy of the Heart Position: located behind sternum. Hollow, muscular organ. Anatomy of the Heart ♥ Consists of 2 separate pumps that maintain unidirectional flow of blood; the Lt & Rt hts. ♥ Left heart pumps oxygenated blood Systemic circulation. ♥ Right heart pumps deoxygenated blood Pulmonary circulation. ♥ Each pump contains 2 chambers: an atrium & a ventricle. ♥ 2 Atria: ■ ■ Chambers of the Heart ♥ 2 Ventricles: Thin-walled chambers. Receive blood returning to heart. ■ ■ ■ Thicker, muscular walls. Pump blood from heart. Each has same capacity & pumps same volume of bl in a given period of time. Chambers of the Heart ♥ Atria & ventricles are separated into 2 functional units by a sheet of fibrous connective tissue, which gives attachment to the valves. Valves of the Heart ♥ 2 Atrioventricular (AV) valves: ■ One way valves. ■ Allow bl to flow from atria into ventricles. ■ Tricuspid (Rt) & Mitral (Lt). ♥ 2 Semilunar valves : ■ One way valves. ■ At origin of pulmonary artery & aorta. ■ Pulmonary (Rt) & Aortic (Lt). ■ Open during ventricular contraction. Valves of the Heart: Remember ■ Vs are at entrance & exit of each ventricle. ■ Vs allow bl to flow in only ONE direction. ■ When AV-vs open, semilunar-vs close & vice versa. ■ Opening & closing of vs occur as a result of press differences. ■ AV cusps are held by chordae tendineae to papillary muscles. Atrioventricular & Semilunar Valves Types of Circulations Pulmonary and Systemic Circulations ■ Pulmonary circulation: – Bl pumped from RV through the lungs & back to the ht. ■ Systemic circulation: – Oxygen-rich bl pumped to all organ systems to supply nutrients from LV ■ Rate of bl flow through systemic circulation = flow rate through pulmonary circulation. Pulmonary Circulation • Moves blood to and from the lungs • Pulmonary trunk – Arises from right ventricle • Pulmonary arteries – Branches of pulmonary trunk which project to lungs • Pulmonary veins – Exit each lung and enter left atrium Systemic Circulation: Arteries • Aorta – From which all arteries are derived either directly or indirectly – Parts • Ascending, descending, thoracic, abdominal • Coronary arteries – Supply the heart Systemic Circulation: Veins • Return blood from body to right atrium • Major veins – Coronary sinus (heart) – Superior vena cava (head, neck, thorax, upper limbs) – Inferior vena cava (abdomen, pelvis, lower limbs) • Types of veins – Superficial, deep, sinuses Fetal Circulation Fetal Circulation •No circulation to lungs •Foramen ovale •Ductus arteriosum •Circulation must go to placenta •Umbilical aa., vv. Larry M. Frolich, Ph.D.,Human Anatomy Heart Walls: 3 Distinct Layers 1. Endocardium: the innermost layer of the ht. 2. Myocardium: the thickest main layer, consists of cardiac ms. 3. Pericardium (epicardium): the thin, outer covering or external membrane around the ht. Adult remnants of fetal circulation Adult Fetus Fossa ovale Foramen ovale Ligamentum arteriosum Ductus arteriosus Medial umbilical ligaments Umbilical aa.(within fetus) Round ligament (ligamentum teres) of liver Ligamentum venosum Umbilical v.(within fetus) Medial umbilical ligament Umbilical cord (leaving fetus) Ductus venosus Physiology of Cardiac Muscle ■ Cardiac muscle tissue forms 2 functional syncytia: atria, & ventricles. The heart is composed of 2 major types of cardiac muscle: 1: Contractile cells. 2: Autorhythmic (or automatic) cells. Contractile cells: Contract when stimulated, in same way as skeletal ms except for longer duration. Heart : Conducting Tissues 1. 2. 3. 4. 5. 6. Sinoatrial (SA) node. Internodal pathways. Atrioventricular (AV) node. Bundle of His. Rt & Lt bundle branches. Purkinje fibers. Heart : Conducting Tissues ♥ Conduction pathway: – – – – – – Sinoatrial (SA) node. Internodal pathways. Atrioventricular (AV) node. Bundle of His. Rt & Lt bundle branches. Purkinje fibers. ♥ Stimulation of Purkinje fibers cause both ventricles to contract simultaneously. Heart : Conducting Tissues ■ SA- node & to a lesser extent AVnode contain small round cells called ‘P cells’ which are probably the actual pacemaker cells. ■ At AV- node, very small no. of intercalated discs & gap junctions delay transmission of impulse. Cardiac Cycle • Heart is two pumps that work together, right and left half • Repetitive contraction (systole) and relaxation (diastole) of heart chambers • Blood moves through circulatory system from areas of higher to lower pressure. – Contraction of heart produces the pressure Regulation of the Heart • Intrinsic regulation: Results from normal functional characteristics, not on neural or hormonal regulation – Starling’s law of the heart • Extrinsic regulation: Involves neural and hormonal control – Parasympathetic stimulation • Supplied by vagus nerve, decreases heart rate, acetylcholine secreted – Sympathetic stimulation • Supplied by cardiac nerves, increases heart rate and force of contraction, epinephrine and norepinephrine released Cardiac Innervations ■ Autonomic Nervous System: I: Sympathetic Nervous System division. II: Parasympathetic Nervous System division. Cardiac Innervations I: Sympathetic Nervous System: ■ Sympathetic nerves that reaches heart originates from POSTGANGLIONIC FIBERS (upper thoracic, paravertebral, ganglia) releases NORADRENALINE. ■ Mainly supplies: – SA-node, – Atrial myocardium, – AV-node, – Ventricular myocardium. Cardiac Innervations II: Parasympathetic Nervous System: ■ Parasympathetic nerve (vagus) that reaches ht originates from PREGANGLIONIC FIBERS (T1 to T5) releases ACETYLCHOLINE. ■ Mainly supplies: – SA-node, – Atrial myocardium, – AV-node. Heart Sounds • First heart sound or “lubb” – Atrioventricular valves and surrounding fluid vibrations as valves close at beginning of ventricular systole • Second heart sound or “dupp” – Results from closure of aortic and pulmonary semilunar valves at beginning of ventricular diastole, lasts longer • Third heart sound (occasional) – Caused by turbulent blood flow into ventricles and detected near end of first one-third of diastole Heart Chambers and Valves Larry M. Frolich, Ph.D.,Human Anatomy Heart Valves: Lub*-Dub** • *Tricuspid Valve: Right AV valve – – – – – – • 3 Cusps (flaps) made of endocardium and CT Cusps anchored in Rt. Ventricle by Chordae Tendinae Chordae Tendinae prevent inversion of cusps into atrium Flow of blood pushes cusps open When ventricle in diastole (relaxed), cusps hang limp in ventricle Ventricular contraction increases pressure and forces cusps closed *Bicuspid (Mitral) Valve: Left AV valve – 2 cusps anchored in Lft. Ventricle by chordae tendinae – Functions same as Rt. AV valve • **Semilunar valves: prevents backflow in large arteries – Pulmonary Semilunar Valve: Rt Ventricle and Pulmonary Trunk – Aortic Semilunar Valve: Left Ventricle and Aorta – 3 cusps: blood rushes past they’re flattened, as it settles they’re pushed down (valve closed) Larry M. Frolich, Ph.D.,Human Anatomy Location of Heart in Thorax pg 523 Larry M. Frolich, Ph.D.,Human Anatomy Location of Heart in Chest • • • • • • • Oblique Position Apex = Left of Midline (5th ICS), Anterior to rest of heart Base (posterior surface) sits on vertebral column Superior Right = 3rd Costal Cartilage, 1” right midsternum Superior Left = 2nd Costal Cartilage, 1” left midsternum Inferior Right = 6th Costal Cartilage, 1” right midsternum Inferior Left = 5th Intercostal Space at Midclavicular line Larry M. Frolich, Ph.D.,Human Anatomy Heart Innervation • Heart receives visceral motor innervation – Sympathetic (speeds up) – Parasympathetic (slows down) p. 534 Larry M. Frolich, Ph.D.,Human Anatomy Fetal Circulation •No circulation to lungs •Foramen ovale •Ductus arteriosum •Circulation must go to placenta •Umbilical aa., vv. Larry M. Frolich, Ph.D.,Human Anatomy Adult remnants of fetal circulation Adult Fetus Fossa ovale Foramen ovale Ligamentum arteriosum Ductus arteriosus Medial umbilical ligaments Umbilical aa.(within fetus) Round ligament (ligamentum teres) of liver Ligamentum venosum Umbilical v.(within fetus) Medial umbilical ligament Umbilical cord (leaving fetus) Ductus venosus Coronary Arteries The heart muscle, like every other organ or tissue in your body, needs oxygenrich blood to survive. Blood is supplied to the heart by its own vascular system, called coronary circulation. The aorta (the main blood supplier to the body) branches off into two main coronary blood vessels (also called arteries). These coronary arteries branch off into smaller arteries, which supply oxygen-rich blood to the entire heart muscle. The right coronary artery supplies blood mainly to the right side of the heart. The right side of the heart is smaller because it pumps blood only to the lungs. The left coronary artery, which branches into the left anterior descending artery and the circumflex artery, supplies blood to the left side of the heart. The left side of the heart is larger and more muscular because it pumps blood to the rest of the body. Conductive system of the heart Electrical impulses from your heart muscle (the myocardium) cause your heart to beat (contract). This electrical signal begins in the sinoatrial (SA) node, located at the top of the right atrium. The SA node is sometimes called the heart's "natural pacemaker." When an electrical impulse is released from this natural pacemaker, it causes the atria to contract. The signal then passes through the atrioventricular (AV) node. The AV node checks the signal and sends it through the muscle fibers of the ventricles, causing them to contract. The SA node sends electrical impulses at a certain rate, but your heart rate may still change depending on physical demands, stress, or hormonal factors.