The importance of patient assessment cannot be overemphasized. EMTs must... Patient assessment
advertisement

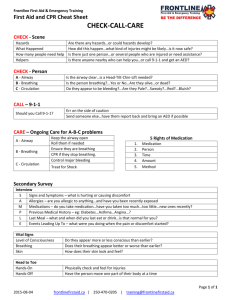
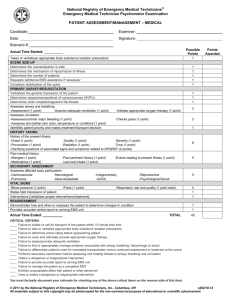
UNIT ONE: Assessment & Triage The importance of patient assessment cannot be overemphasized. EMTs must master and be comfortable with the patient assessment process. Patient assessment is used, to some degree, in every patient encounter. EMTs develop and perfect their own assessment techniques as they complete their education and gain experience in the field. The assessment process is divided into five main parts: l. Scene size-up 2. Primary assessment 3. History taking 4. Secondary assessment 5. Reassessment Although the steps of the l. Scene size-up When you are alerted for an emergency call, your dispatcher will provide you with some basic information about the situation that requires your assistance. Your scene size-up begins here. The scene size-up is how you prepare for a specific situation. From the moment you are called into action until you finally reach your patient, you must consider a variety of things that will have an impact on how you begin to care for your patient. The scene size-up includes dispatch information and must be combined with an inspection of the scene to help you ensure safety and identify hazards, safety concerns, and the number of patients you may have, as well as additional resources you might need to safely and effectively care for the patient. During your prehospital assessment you may be tempted to categorize your patient immediately as a trauma or medical patient. Remember, the fundamentals of a good patient assessment are the same despite the unique aspects of trauma and medical care. If an unconscious patient is found at the bottom of a ladder, did he fall off the ladder, strike his head, and become unconscious or did he experience a medical problem that caused him to fall off the ladder and then lose consciousness? Early in the assessment, it can be difficult to identify with absolute certainty whether the problem is of a traumatic or medical origin. Although further assessment is needed to come to a conclusion, considering 1 UNIT ONE: Assessment & Triage the mechanisrn of injury (MOI) or nature of illness (NOI) early will help you prepare for the rest of your assessment. II. Primary assessment The primary_ assessment has a single, critical, all-important goal to identify and initiate treatment of immediate or potential life threats. The patient's vital signs (level of consciousness; airway, breathing, and circulation [ABCs]) will determine the extent of your treatment at the scene. Vital signs are the key signs that are used to evaluate the patient's condition. Always give priority to the patient's level of consciousness and ABCs to ensure lifesaving treatment from here you will be able to determine the priority of patient care and transport. Form a General Impression: Anytime you meet someone new, you form an initial general impression about that person. Forming an Initial general impression of your patient is a similar process, but it helps to focus your attention toward life threatening problems. The initial general impression is formed to determine the priority of care and is based on your immediate assessment of the patient. This includes noting things such as the person's age, sex, race, level of distress, and overall appearance. You may anticipate different problems depending on the parent’s age, sex, and race. A woman reporting abdominal pain, for example, may have more serious implications than a man with the same complaint because of the complexity of the female reproductive system. Write any important information down because it will be difficult to remember minor details later. You should think of your initial general impression as a visual assessment, gathering information as you approach the patient. As you approach, make sure that * the patient sees you coming to avoid surprising the patient or causing the patient to turn to see you, possibly making any injuries worse. Note the patient’s position and whether the patient is moving or still. After you introduce yourself, you should ask the patient about the chief complaint. Assess the patient’s skin color and condition as you begin. For example, is the patients skin pink, pale, gray, or cyanotic? Is it dry clammy, or diaphoretic? The patient may direct you to a wound on his or her leg or demonstrate an airway problem by creating 2 UNIT ONE: Assessment & Triage abnormal sounds when breathing. If a life-threatening problem is found, it should be treated immediately Determine whether your patient's condition is stable, stable but potentially unstable, or unstable. Assess Level of Consciousness The patient's level of consciousness (LOC) is considered a vital sign because it can tell a great deal about the patient's neurologic and physiologic status. The brain requires a constant supply of oxygen and glucose to function properly in the primary assessment, you need to ascertain only the gross LOC by determining which of the following categories best fits your patient: 1-Conscious with an unaltered LOC 2-Conscious with an altered LOC 3-Unconscious When a patient is conscious with an altered LOC, it may indicate that inadequate perfusion and oxygenation or a chemical or neurologic problem is adversely affecting the brain and its ability to function. Your assessment of a patient who is unconscious should focus initially on problems with airway, breathing, and circulation, which are critical life threats, and then identify other emergency care that the patient may need. Sustained unconsciousness should warn you that a critical respiratory, circulatory, or central nervous system problem or deficit may exist, and you must assume that the patient has a potentially critical injury or potentially life-threatening condition. Therefore, after rapidly assessing the patient and providing emergency treatment, you should package the patient and provide rapid transport to the hospital. The AVPU scale is a rapid method of assessing the patient's level of consciousness using one of the following four terms: A ...Awake and Alert V... Responsive to Verbal stimuli P... Responsive to Pain U.. Unresponsive Assess the Airway As you move through the steps of the primary assessment, you must always be alert for signs of airway obstruction. Regardless of the cause, a mild or severe airway obstruction will result in inadequate or absent air flow into and out of the lungs. To prevent permanent damage to the 3 UNIT ONE: Assessment & Triage brain, heart, and lungs, or even death, you must determine if the airway is open (patent) and adequate. Assess Breathing A patients breathing status is directly related to the adequacy of his or her airway. Once you have made sure the patient's airway is open, make sure the patient's breathing is present and adequate. A patient who is breathing without assistance is said to have spontaneous respirations or spontaneous breathing. When assessing breathing, you must obtain the following information: Respiratory rate Rhythm, regular or irregular Quality/character of breathing Depth of breathing Oxygen should always be administered to patients who are having difficulty breathing, but it may also be provided to patients who are breathing adequately. Positive-pressure ventilations should be performed for patients who are apneic or whose breathing is too slow or too shallow. lf a patient seems to develop difficulty breathing after your primary assessment, you should immediately reevaluate the airway. lf the airway is open and breathing is present and adequate, you should consider Administering supplemental oxygen. If breathing is present and inadequate (the normal rate is 12 to 20 breaths/min in adults) because respirations are too fast (generally more than 20 breaths/min), too shallow, or too slow (generally fewer than 12 breaths/min), you should administer supplemental oxygen. When respirations exceed 24 breaths/min or are fewer than 8 breaths/min, you should consider providing positive pressure ventilations with an airway adjunct. Remember that air exchange is the critical issue, not the number of breaths. .Assess Circulation: Assessing circulation helps you to evaluate how well blood is circulating to the major organs, including the brain, lungs, heart, kidneys, and the rest of the body A variety of problems can impair circulation, including blood loss, shock, and conditions that affect the heart and major blood vessels. Circulation is evaluated by assessing the pulse rate, pulse quality, and pulse rhythm. You will also need to identify external bleeding and evaluate the skin. 4 UNIT ONE: Assessment & Triage Assess and Control External Bleeding: Perform a rapid scan of the patient to identify any major external bleeding. in some cases, blood loss can be very rapid and can quickly result in shock or even death. Therefore, this step demands your immediate attention. Signs of blood Loss include active bleeding from wounds and./or evidence of bleeding such as blood on the clothes or near the patient. Serious bleeding from a large vein may be characterized by steady blood flow. Bleeding from an artery is characterized by a spurting flow of blood. When you evaluate an unconscious patient, do a sweep for blood quickly and lightly by running your gloved hands from head to toe, pausing periodically to see if your gloves are bloody. Controlling external bleeding is often very simple. Initially, direct pressure with your gloved hand and soon thereafter a sterile bandage over the wound will control bleeding in most cases. This direct pressure stops the bleeding and helps the blood to coagulate, or clot naturally Most often, bleeding can be adequately controlled by using direct pressure, along with elevating the extremity if bleeding is from the arms or legs. When direct pressure and elevation are not successful, you should apply a tourniquet. Identify and Treat Life Threats: Many conditions present an immediate threat to life, and key to your role as an EMT is to determine if a life threat is present and, if so, to quickly address it. In many situations, there is a process the body takes when reacting to a life threat. Lifesaving interventions begin with you opening the airway. Airway patency is your number one priority Assess the patients breathing, and initiate ventilations in patients who have inadequate respirations or a respiratory rate greater rhan24 or less than 8 breaths/min. Perform a Rapid Scan You will need to take 60 to 90 seconds and perform a rapid scan of the patient's body to identify injuries that must be managed and\or protected immediately this is not a systematic or focused physical examination. Perform a Rapid Scan You will need to take 60 to 90 seconds and perform a rapid scan of the patient's body to identify injuries that must be managed and\or protected immediately This is not a systematic or focused physical examination. Determine Priority of Patient care and Transport As you complete your primary assessment, you have to make some decisions about patient care and transport. The rapid scan will assist you in determining transport priority. Would you consider your patient a high, medium, or low priority for transport? Priority designation is used 5 UNIT ONE: Assessment & Triage to determine if your patient needs immediate transport will tolerate a few more minutes on scene. Patients with any of the following conditions are examples of high priority Patients and should be transported immediately: . Difficulty breathing Poor general impression Unresponsive with no gag or cough reflex Severe chest pain Pale skin or other signs of poor perfusion Complicated childbirth Uncontrolled bleeding Responsive but unable to follow commands Severe pain in any area of the body In ability to move any part of the body Protecting the patients spine and identifying fractured extremities are integral parts of packaging for transport. lf a spinal injury is suspected or the MOI is significant enough to cause a possible injury consider spinal immobilization early. If you are unsure if spinal immobilization is necessary always err on the side of caution and immobilize the patient. These injuries can be made worse if you neglect to assess and treat them before moving the patient. Recognizing the need to transport serious trauma patients is of such importance that you may hear colleagues refer to the Golden Period. This refers to the time from injury to definitive care, during which treatment of shock and traumatic injuries should occur because survival potential is best. After the first 60 minutes, the body has increasing difficulty in compensating for shock and traumatic injuries For this reason, you should spend as little time as possible on scene with patients who have sustained significant or severe trauma. Aim to assess, stabilize, package, and begin transport to the appropriate facility within 10 minutes (often referred to as the "Platinum I0") III-History taking History taking provides detail about the patient’s chief complaint and an account of the patients signs and symptoms. It is important to document all of the information. on gathered during this phase of the assessment process. This includes demographic information, past medical history, and current health status of the patient. Be sure to document the following information: Date of the incident All times of assessments and interventions Patient's age Patient's sex 6 UNIT ONE: Assessment & Triage Patient's race Past medical history including any pertinent information about the patient’s condition, such as medical problems, traumatic injuries, and surgeries Patient's current health status, including diet, medications, drug use ,Living environment and hazards, physician visits for immunizations or testing, and family history. IV-secondary assessment: The purpose of the secondary assessment is to perform a systematic physical examination of the patient. The physical examination may be a systematic head-to toe, full-body scan or a systematic assessment that focuses on a certain area or region of the body, often determined through the chief complaint. Circumstances will dictate which aspects of the physical examination will be used. The following are guidelines on how and what to assess during a physical examination: Inspection. Inspection is simply looking at your patient for abnormalities. This is done by looking for anything that may indicate a problem. For example, swelling in a lower extremity may indicate an acute injury or a chronic illness. Palpation. Palpation describes the process of touching or feeling the patient for abnormalities. At times palpation is gentle, and at other times it is firmer and will help you to identify where the patient has pain. Your fingertips are best suited for detecting texture and consistency, while the back of your hand is best suited for noting temperature. Auscultation. Auscultation is the process of listening to sounds the body makes by using a stethoscope. For example, when measuring a patient's blood pressure, you listen to the flow of blood against the brachial artery with the head of the stethoscope.This is auscultation of a blood pressure. The mnemonic DCAP-BTLS will help remind you what to look for when inspecting and palpating various body regions. Each area of the body is evaluated for the following: Deformities Contusions Abrasions 7 UNIT ONE: Assessment & Triage Punctures/penetrations Burns Tenderness Lacerations Swelling Assess Vital Signs Using the Appropriate Monitoring Device Pulse Oximetry :Pulse oximetry is a newer assessment tool that is used to evaluate the effectiveness of oxygenation. The pulse oximeter is a photoelectric device that monitors the Oxygen saturation of hemoglobin. Noninvasive Blood Pressure Measurement : The sphygmomanometer, or blood pressure cuff, is used in the measurement of the patient's blood pressure. electronic measurement,is another method of obtaining blood pressure readings on patients. End-Tidal Carbon Dioxide: Capnography is a noninvasive method that can quickly and Efficiently provide information on a patient's ventilator status. Circulation. and metabolism. It can be used as a secondary tool during the confirmation of endotracheal intubation or the effectiveness of ongoing CPR. End-tidal co, is the partial pressure or maximal concentration of CO2, at the end of an exhaled breath, which is expressed as a percentage of co2, or millimeters of mercury The normal range is 35 to 45 mm Hg, or 5 % to 6 % co2. When co, is absent when measured by capnography, it may indicate the endotracheal tube is in the wrong position or there is an absence or decrease in the level of co, in the lungs, possibly from cardiac arrest, ineffective CPR, or shock. When cardiac output increases, the end-tidal co2, measurement will provide information on the adequacy of ventilations and circulation. Systematically Assess the Patient- Full-Body Scan: The full-body scan is a systematic head-to-toe examination. The goal of this process is to identify hidden injuries or identify causes that may not have been found during the 60- to 9Osecond rapid scan that took place during the primary assessment. Any patient who has sustained a significant MOl, is unconscious, or is in critical condition should receive this type of examination. An unconscious patient is unable to tell you what is wrong; therefore, this type of examination may give you clues to identify the problem. 8 UNIT ONE: Assessment & Triage V-Reassessment: Is performed at regular intervals during the assessment process, and its purpose is to identify and treat changes in a patient's condition. Reassessment should take Place: every 5 minutes for patients in unstable condition every 15 minutes for patients in stable condition 9