Document 15352335
advertisement

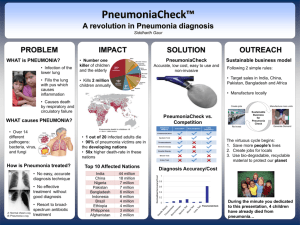
Introduction 0 Pneumonia is an inflammation of the lung parenchyma (i.e. alveoli rather than the bronchi) of infective origin. 12/12/2011 Pneumonia 2 0 It is the most common infectious cause of death. 0 It is usually characterized by consolidation. 0 Consolidation is a pathological process in which the alveoli are filled with a mixture of inflammatory exudate, bacteria & WBC 12/12/2011 Pneumonia 3 EPIDEMIOLOGY 0 Occurs throughout the year 0 Results from different etiological agents varying with the seasons 0 Occurs in persons of all ages 0 Clinical manifestations severe in very young, elderly & in chronically ill patients 12/12/2011 Pneumonia 4 CLASSIFICATION Classified based on two types 1. Type 1 0 Lobar pneumonia 0 Bronchopneumonia 2. Type 2 0 Community- acquired pneumonia (CAP) 0 Hospital-acquired pneumonia (HAP) 12/12/2011 Pneumonia 5 Lobar pneumonia 0 Lobar pneumonia is acute bacterial infection of a part of lobe the entire lobe, or even two lobes of one or both the lungs. 12/12/2011 Pneumonia 6 Bronchopneumonia 0 Bronchopneumonia is infection of the terminal bronchioles that extends into the surrounding alveoli resulting in patchy consolidation of the lung. 12/12/2011 Pneumonia 7 Community Acquired Pneumonia (CAP) Pneumonia which develops in an otherwise healthy person outside of hospital or have been in hospital for less than 48hrs 12/12/2011 Pneumonia 8 Nosocomial pneumonia (HAP) Pneumonia that was not incubating upon admission developing in a patient hospitalized for greater than 48 hrs. 12/12/2011 Pneumonia 9 PATHOPHYSIOLOGY Microbial invasion of the normally sterile lower respiratory tract Three routes0 Inhaled as aerosolized particles 0 Haematogenous spread from an extrapulmonary site of infection 0 Aspiration of oropharyngeal contents 12/12/2011 Pneumonia 10 Various defence mechanisms that protects lung from infection 0 Anatomic barriers –epiglottis, larynx 0 Cough reflexes 0 Tracheobronchial secretions 0 Mucocilliary lining 0 Cell & humoral mediated immunity 0 Dual phagocytic system-alveolar macrophages & neutrophils 12/12/2011 Pneumonia 11 Invasion occurs as a result of 0 Defect in host defence mechanism 0 Overwhelming inocculum 0 Lung infection with viruses suppress the antibacterial activity of the lung by impairing alveolar macrophage function & mucocilliary clearance thus setting the stage for secondary bacterial pneumonia. 12/12/2011 Pneumonia 12 Clinical Manifestations 0 0 0 • • • • • • • 0 0 Indolent to fulminant in presentation Mild to fatal in severity Typical symptoms – Fever Chills Cough Rust coloured sputum Mucopurulent sputum Dyspnea ( shortness of breath) Pleuritic chest pain Elevated WBC Bacteraemic 12/12/2011 Pneumonia 13 Chest X-ray For Lobar Pneumonia Consolidation confined to one or more lobes (or segments of lobes) of lungs. Lobarpneumonia 12/12/2011 Pneumonia 14 Chest X-ray For Bronchopneumonia •Patchy consolidation usually in the bases of both lungs. Bronchopneumonia 12/12/2011 Pneumonia 15 Diagnosis Clinical diagnosis 0 History 0 Signs & symptoms 0 Chest x-ray 0 CT 12/12/2011 Pneumonia 16 Diagnosis Etiological diagnosis 0 Gram's Stain and Culture of Sputum 0 Blood Cultures 0 Antigen Tests 0 Polymerase Chain Reaction 0 Serology 0 Bronchoalveolar lavage 0 Bronchoscopy 12/12/2011 Pneumonia 17 Complications Possible complications include: 0 Acute respiratory distress syndrome (ARDS) 0 Fluid around the lung (pleural effusion) 0 Lung abscesses 0 Respiratory failure (which requires a breathing machine or ventilator) 0 Sepsis, which may lead to organ failure 12/12/2011 Pneumonia 18 COMMUNITY ACQUIRED PNEUMONIA Pneumonia is most common in winter because of seasonal increase in viral infections Mortality 1%- Non hospitalized patients 13.7%-Hospiatalized patients 19.6%-Bacteremic patients <36.5%- Intensive care unit 12/12/2011 Pneumonia 19 Risk factors 1. 2. 3. 4. 5. 12/12/2011 Comorbidity- Neoplastic disease, neurological problem Alcoholism Advanced age Asthma Immunosuppression Pneumonia 20 Etiology Potential etiologic agents in CAP - Bacteria Viruses Fungi Protozoa Potential bacteriologic causes can be divided into two types 0 Typical bacterial pathogens 0 Atypical bacterial pathogens 12/12/2011 Pneumonia 21 Typical bacterial pathogens 0 Streptococcus pneumoniae – 30% to 60% ,Severe illness, death 0 Haemophilus influenzae - 10% 0 S. aureus (in selected patients) 0 gram-negative bacilli – Klebsiella pneumoniae Pseudomonas aeruginosa 12/12/2011 Pneumonia 22 Atypical bacterial pathogens 0 Mycoplasma pneumoniae 0 Chlamydophila pneumoniae 0 Legionella pneumophillia 0 These organisms are intrinsically resistant to all - B lactam agents macrolide, a fluoroquinolone, or a tetracycline. 0 Poor dental hygiene-anaerobes 0 HIV- p.carnii 0 Birds- Chlamydia psittaci 0 Cattle or parturient cat-Coxiella burnetti 12/12/2011 Pneumonia 23 HOSPITAL ACQUIRED PNEUMONIA 0 Pneumonia that was not incubating upon admission developing in a patient hospitalized for greater than 48 hrs 0 10-15% of all hospital acquired pneumonia, usually presenting with sepsis or&/or respiratory failure 0 50% acquired on ICU 12/12/2011 Pneumonia 24 Predisposing features Reduced host defence against bacteria 0 Reduced immune defences (Corticosteroid treatment, diabetes, malignancy) 0 Reduced cough reflux (Post operative) 0 Disordered mucocilliary clearance (Anaesthetic agents) Aspiration of nasopharyngeal or gastric secretions 0 Immobility or reduced conscious level 0 Vomiting, Dysphagia, 0 12/12/2011 Nasogastric intubation Pneumonia 25 0 Most bacterial nosocomial infection occur by microaspiration of bacteria colonizing the patients oropharynx or upper GI tract 0 Most common pathogen – Aerobic gram negative bacilli 0 Most commonly exposed to multiresistant hospital pathogen 0 86% nosocomial infection-mechanical ventilation 0 Mortality-0 to 50% 12/12/2011 Pneumonia 26 Bacterial introduction into LRT Endotracheal intubation Infected ventillatiors / nebuliser /bronchoscopy Dental or sinus infection Bacteraemia Abdominal sepsis Intravenous canula 12/12/2011 Pneumonia 27 Causative organisms Common organisms Gram negative bacteria0 Escherichia coli 0 Klebsiella sp. 0 Pseudomonas aeruginosa Gram positive bacteria0 Streptococcus pneumoniae 0 Staphylococcus aureus 12/12/2011 Pneumonia 28 Less common organisms 1. 0 0 0 0 0 2. 3. 4. 12/12/2011 Gram negative bacilli other coliforms:Enterobacter sp. Proteus sp. Seratia marcescens Citrobacter sp. Acinobacter sp. Legionella pneumophillia Anaerobic bacteria Fungi- Candida albicans Aspergillus fumigatus Viruses- Cytomegalovirus (CMV), Herpes simplex Pneumonia 29 Treatment Goals of therapy- 0 Eradication of the offending organism. 0 Selection of an appropriate antibiotic. 0 To minimize associated morbidity. 12/12/2011 Pneumonia 30 General approach to treatment 0 Adequacy of respiratory function 0 Humidified oxygen for hypoxemia 0 Bronchodilators (albuterol) 0 Chest physiotherapy with postural drainage 0 Adequate hydration if necessary 0 Expectorants such as guaifenesin 0 Chest pain- analgesics 12/12/2011 Pneumonia 31 Selection of an antimicrobial agent 0 Empirical use of relatively broad spectrum antibiotic 0 Narrow spectrum antibiotics to cover specific pathogen 0 Potential pathogens involved 0 Age 0 Previous &current medication history 0 Underlying disease 0 Present clinical status 12/12/2011 Pneumonia 32 Antibiotic doses for treating pneumonia 12/12/2011 Pneumonia 33 Treatment for special cases 1. Patient less than 60 years & without comorbidities:Azithromycine ( 500mg OD) *1day ( 250mg OD) *4days Norfloxacin/Levofloxacin (400mg OD) *7days 2. Outpatient greater than 65 years:Norfloxacin (400mg OD) *7days or Ceftriaxon (1-2 g/day) / Cifixim (2-4 g/day) 3rd gen cefalosporins + 12/12/2011 Pneumonia 34 Macrolides like Azithromycin ( 500mg OD) *1day ( 250mg OD) *4days 3. Patient is hospitalised but not severely ill:Combination of 3rd gen cefalosporins + Macrolides Ceftriaxone + Azithromycin OR Norfloxacin/Levofloxacin (400mg OD) 4. If the patient is hospitalised but not severely ill:Combination of 3rd gen cefalosporins + Macrolides Ceftriaxone + Azithromycin and newer fluroquinolones (Gatifloxacin) 12/12/2011 Pneumonia 35 5. Patient hospitalised & severely ill:- Combination of 3rd gen cefalosporins + Macrolides Ceftriaxone + Azithromycin and newer fluroquinolones (Gatifloxacin) We can add Vancomycin. 6. Patient with icu admission:3rd gen cefalosporins + Fluroquinolones (Gatifloxacin) + Nutritional supplements + Saline Vancomycin/Meropenam 12/12/2011 Pneumonia 36 7. For HAP:- Cephalosporins + Aminoglycocides 8. For antipseudomons cephalosporins:- Ceftazidime + Cefexime 12/12/2011 Pneumonia 37 Drugs with usual doses 12/12/2011 Pneumonia 38 12/12/2011 Pneumonia 39 12/12/2011 Pneumonia 40 12/12/2011 Pneumonia 41