motor functions of the stomach
advertisement

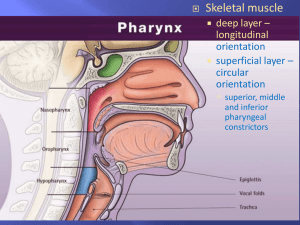
Motor functions of the stomach Dr. Khaled Ibrahim a. Enumerate the motor functions of the stomach. b. Describe the propulsive movements of the stomach and discuss their significance. c. Describe hunger pains and discuss their mechanism. d. Describe gastric emptying and discuss its physiological regulation and different factors affecting it. e. Describe vomiting and list its possible causes. • Text book of Medical Physiology by Guyton and Hall 12th Edition, PAGE 765 –768. • Ganong's review of Medical Physiology 24th edition, Page 502-504. Motor Functions of the Stomach 1) Storage Functions The volume of empty stomach is 50 ml but when food enters stomach fundus and upper portion of body relax (Receptive Relaxation) ing its volume up to 1.5 L without a marked in pressure. Mechanism: this relaxation is mediated by purinergic inhibitory vagal fibers and initiated by movements of pharynx and esophagus during swallowing. 2) Mixing Movements (Peristalsis): 2) Mixing Movements (Peristalsis): Definition: Weak peristaltic waves that move along gastric wall pylorus. Mechanism: These waves are controlled by basal electrical rhythm (BER). BER is a wave of depolarization & repolarization originating from pace-maker cell at a rate of one/ 20 sec. The wave can't produce contraction but needs neural or hormonal factors potential can reach threshold level contraction. The frequency of BER is : - ed by gastrin, vagal stimulation and gastric distension. - ed by symp. stimulation, duodenal distension, fats, and acids. Pyloric valve closed 1 Propulsion: Peristaltic waves move from the fundus toward the pylorus. Pyloric valve closed 2 Grinding: The most vigorous peristalsis and mixing action occur close to the pylorus. Pyloric valve slightly opened 3 Retropulsion: The pyloric end of the stomach acts as a pump that delivers small amounts of chyme into the duodenum, simultaneously forcing most of its contained material backward into the stomach. Description and Function: Filled stomach contraction wave that mix food with gastric secretion, and move mixed contents toward the antrum (i.e. Propulsion). When gastric contents reach to closed sphincter, the contents move back toward body of stomach (i.e. Retropulsion). After sometimes, pyloric sphincter open passing a small amount of most fluidly part of contents then the sphincter closes again. Repeated propulsion & retropulsion are called Pyloric Mill as they cause complete grinding & mixing of food e gastric juice forming "chyme". 3) Emptying of the Stomach Means emptying of gastric content into the duodenum. The Rate of gastric emptying is slow and small in volume. Significance of slow rate: prevents sudden stretch of duodenum (its capacity is low so, its sudden stretch abdominal discomfort, nausea & vomiting). Mechanism: The emptying depends on difference in pr. ( ) pyloric antrum & duodenal bulb. During peristalsis, pr. in pyloric antrum becomes > duodenum (pyloric pump). So, gastric contents passes to duodenum till the pylorus closes to prevent regurgitation of duodenal contents into the stomach. Regulation of Gastric Emptying: Regulated by signals both from the stomach & the duodenum. I. Gastric Factors: helps gastric emptying. 1) Nervous Signals: Gastric distension by food ++ mechanoreceptors in gastric wall Long vago-vagal and short reflexes (through ENS) Pyloric pump and inhibit pyloric sphincter. 2) Hormonal Signals: Stimulation of chemo- & mechano receptors gastrin release from antrum Pyloric pump and inhibit pyloric sphincter. 3) Consistency of Gastric Contents: Soft food emptied quicker than hard food. II. Duodenal Factors: inhibit gastric emptying 1) Nervous Signals: Distension & acidity of duodenum enterogastric reflex which inhibits gastric emptying. This reflex is mediated through: a) Extrinsic nerves Through inhibitory symp. nerve fiber to the stomach OR Transmitted by vagus n. to vagal nucl. and then efferent purinergic vagal fibers to the stomach. b) Local signals: Inhibitory impulses through ENS from upper part of duodenum reaching the stomach to inhibit its motility. Factors Initiating Enterogastric Reflex: 1) Duodenal distention. 2) Irritation to duodenal mucosa. 3) Degree of acidity: duodenal acidity inhibits gastric emptying until the acidity is neutralized by pancreatic secretion. 4) Products of protein digestion: to insure complete protein digestion in upper small intestine. 5) Degree of osmolality: hypo- or hypertonic fluids: to prevent electrolyte imbalance. 2) Hormonal Signals: Fat in duodenum release certain hormones (enterogastrone) from upper intestine, which inhibit gastric emptying. Enterogastrone include : Cholecystokinin (CCK), secretin and Gastric Inhibitory Peptide (GIP). - CCK acts as a competitive inhibitor for gastrin. - GIP and secretin act by inhibiting gastric motility. Motility of Fasted Stomach 1. Migrating Motor Complex (MMC): Def. Periodic phasic contraction occurring at regular and low frequency, once /6-20 min. Function of MMC : 1) It clears stomach and S.I from indigestible residues. So, called "the house-keeper of the gut". 2) It prevents duodenogastric reflux. Mechanism: unknown but its strength is increased by motilin hormone 2. Hunger contractions (Hunger Pangs): Definition: rhythmic peristaltic contraction that may fuse together forming continuous contractions lasting 2-3 min pain which is called hunger pangs. Occurs in empty stomach after long time of fasting (12-24 h). In starvation, hunger pangs reach maximum intensity in 3-4 days and then gradually and fasting can be continued without pain. Mechanism of Hunger Contraction: - Food regulating center in hypothalamus is consists of 2 parts: 1) Feeding center: when stimulated, it causes person to eat. 2) Satiety center: when stimulated, it causes complete satiety. Stomach -------> hunger painfeeding During normal Satiety Center conditions Vagus nerve Feeding Center ---- ------During fasting conditions Glucoreceptors in the hypothalamus Blood glucose level decreases +++ +++ Vomiting Definition: Outward expulsion of gastric contents through esophagus, pharynx & mouth. Mechanism of vomiting: Reflex in nature - Receptors & Afferent: vagal and sympathetic fibers from different parts of body. - Center: vomiting center in M.O. - Efferents from vomiting center pass through: 5th , 7th , 9th , 10th and 12th cranial nerves, go to the GIT. Spinal nerves to diaphragm and abdominal muscles. Response: Elevation of soft palate to close post. nasal cavity. Movement of larynx and hyoid bone ant. and upward pulling of UES Closure of the epiglottis. Strong downward contraction of diaphragm with simultaneous contraction of anterior abdominal muscle. The resulting in intra-abdominal pressure with relaxation of cardiac sphincter & strong contraction at pylorus stomach is squeezed (being passive and relaxed) expulsion of its contents through esophagus. Causes of Vomiting: 1) Reflex Vomiting: impulses from body ++ of vomiting center Mechanical ++ of posterior part of tongue. Irritation of mucosa of stomach and duodenum e.g. gastritis. Visceral pain e.g. acute pertionitis, appendicitis and intestinal obstruction. Myocardial infarction. Motion sickness: afferent sensory fibers from inner ear. 2) Psychic or Emotional Causes: Seeing or smelling certain substance vomiting (through conditioned reflex). 3) Chemical Causes: Vomiting can be caused by impulses arising in chemoreceptor trigger zone (an area of brain outside vomiting center) by: Certain drugs e.g. apomorphine, morphine and digitalis derivatives. Production of emetic substances (in pregnancy) or toxins (in uraemia). Massive doses of x-ray liberation of certain chemical substances (radiation sickness). Stimulation of chemoreceptor trigger zone -------> stimulation of vomiting center ---------> vomiting. 4) Nervous Causes: Mechanism: Intracranial tension (ICT) as in meningitis, migraine & brain tumors cerebral ischemia hypoxia +++ vomiting center. Characters: The central vomiting is: Projectile (strong and sudden) and not proceeded by nausea. Associated with blurring of vision & headache (due to ICT)