Complications of Dibetes
advertisement
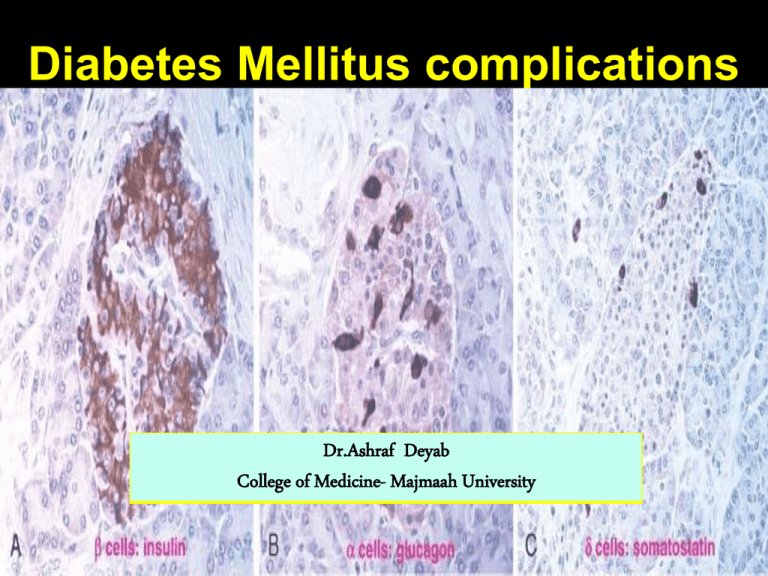
Diabetes Mellitus complications Dr.Ashraf Deyab College of Medicine- Majmaah University Pathology of diabetes complication • By the end of this session, the student should: • Discuss the pathogenesis of diabetes complications. • Describe the morphology of diabetes complication. • Discuss epidemiology, public health importance, prevention and screening (where applicable) of diabetic complications. Acute and chronic DM complications Acute complication 1. Diabetic ketaoacidosis= DKA. 2. Hyperglycemia hyperosmolar state = (HHS), ‘nonketaotic” 3. Hypoglycemia 4. Diabetic coma 5. Respiratory infections 6. Periodontal disease 7. Impaired wound healing Chronic complications Macrovascular disease Microvascular disease 1. 2. 3. 4. 5. 6. Diabetic nephropathy Diabetic neuropathy Diabetic retinopathy Cataract Diabetic cardiomyopathy Diabetic embryopathy Pathogenesis of DM complications • Pathologic sequelae caused by persistent hyperglycemia (“glucotoxicity”) , lead to metabolic dys-regulation, considered as responsible for the short& long-term complications. • Hyperglycemia- basically lead to damage of blood vessels (angiopathy) grouped under two types: 1) Microvascular angiopathy: capillaries dysfunction in target organs -e.g. diabetic neuropathy, nephropathy, and retinopathy. 2) Macrovascular angiopathy: Both large& Medium-sized muscular arteries (Myocardial infarction, stroke, and peripheral vascular insufficiencyaccelerated atherosclerosis, peripheral LL amputation) • Three distinct metabolic pathways have been implicated in this serious effects of persistent hyperglycemia on peripheral tissue: • (1) Formation of Advanced (Protein) Glycation End product (AGE) • (2) Activation of Protein Kinase C (PKC) • (3) Intracellular Hyperglycemia and Disturbances in Polyol Pathways Pathogenesis of DM complications • I) Formation of Advanced Glycation End Products-(AGE). (1) Hyperglycemia increase protein glycation gradual build-up of (AGEs) (a) Release pro-inflammatory markers (b) Free radical activity ↓↓↓ Cells& vessels injury Microangiopathy (2) AGEs Cross-linking with collagen (type I in- BV. +type IV in- BM) Decreases their elasticity+ Increases extravasation of fluid + Decreases protein removal while + Enhancing protein& LDL deposition. • II) Activation of Protein Kinase C (PKC): The activation of PKC initiates a complex Intracellular signals 1- Increases in vascular permeability, 2- BM thickening with ECM deposition flexibility affected 3- Angiogenesis- proliferation tendency 4- Apoptosis, 5-Vascular occlusion + decrease fibrinolysis Vasoconstriction • Pathogenesis of DM complication • III) Intracellular Hyperglycemia &Disturbances in Polyol Pathways: polyol pathway= sorbitol aldose reductase pathway. • Insulin-independent tissue: like in BV, retina, kidney and nerves, any Unused\excess glucose enter polyol pathways. 1) Unused\excess glucose enter polyol pathways formation of Sorbitol , mediated by Aldose reductase (using much more NADPH) (a) Sorbitol-accumulation cannot cross cell membranes (osmotic influx of water) CATRACT. (b) NADPH deficiency 2) NADPH deficiency lead to glutathione deficiency induce cells Oxidative stress Release& accumulation of reactive oxygen species\ free radicals: (a) Decreased concentrations of nitric oxide, inositol (b) Cell injury (c ) Hemolysis (d ) Vasoconstriction, etc…. DM morphology: Principal organs affected in diabetes mellitus (not related to pancreas only” depend on the late complications: Eyes • Retinopathy • Cataract • Glaucoma Pancreas • Islet cells: - Insulitis (type I). Amyloid deposition (type II) Blood vesselsAngiopathy • Macrovascular • Microvascular. Kidney Atherosclerosis Nephropathy: Foot Gangrene . Nephroscerlosis\ MI. Glomeruloscelrosis. • Arterioscelrosis CVA • pyelonephritis HTN Nerves: - Peripheral +Autonomic Neuropathy 1)Pancreas : pancreatic lesions are neither constant nor necessarily pathognomonic. They are more likely to be distinctive in type I >> in type II. One or more of the following alterations may be present:-1. Reduction in the size& number of islets (DM-1), ↓islet mass (DM-2). 2. Increase in the size & number of islets (nondiabetic newborns of diabetic mothers). 1. . DM-1: Leukocytic infiltration (insulitis)- mostly T- cells, Eosinophilic infiltrates (Autoimmune diseases) DM-2: Amyloid replacement of islets and around capillaries & b\w islet cells obliteration & fibrosis. DM-1 DM-2 Blood vessels. Small vessels (Diabetes microangiopathy) . Morphologic features Diffuse Thickening& widening of basement membrane by a homogeneous , sometimes multilayered hyaline substance= PAS stain positive. Capillaries are more leaky than normal to plasma proteins. EXAMPLES: kidenys (glomeruli, tubules, renal medulla) , skin, muscle, eye-retina/ etc……. Diabetic Macrovascular Disease Atherosclerosis (AT): Endothelial dysfunction- predisposes (LDL deposition). Hyaline arteriolosclerosisAmorphous, hyaline thickening wall of the arterioles, which causes narrowing of the lumen. Complications: AT MI, CVA, Gangrene of the lower extremities etc.. Kidneys. (Diabetic Nephropathy ). The kidneys are second target for DM after the heart . • The second leading cause of death after MI from DM. • Three lesions are encountered: Morphology ( after> 20 yrs of diabetes) Glomerular and tubular lesions: Most specific for DM is Nodular Glomerulosclerosis: = (KimmelstielWilson lesion), chr. Nodular intercapillary lesion - Capillary and Tubular BM thickening. - Mesangial matrix widening, ↑↑↑cellularity. - Diffuse mesangial sclerosis. Renal vascular lesions:Arteriosclerosis - Thickeneing of basement membrane. - Severe hyaline changes Interstitial lesion: - Interstitial inflammation. - Pyelonephritis, including necrotizing papillitis Severe renal hyaline (afferent art.) arteriolosclerosis Nephrosclerosis long-standing DM thickening of tubular BM Nodular “intercapillary” glomerulosclerosis Eyes( diabetic Retinopathy) Morphology- divided into 2 groups I. Diabetes microangiopathy (non proliferative) a) Macular edema (visual loss): Thickening of the Basement membrane Breakdown of the blood-retinal barrier lead to leakage with micro-occlusion b) Pericyte degeneration+ arteriolar hyalinzation c) Microaneurysms d) Retinal micro-hemorrhages- cotton-wool spots II. Intraretinal angiogenesis (proliferative phase) a) Retinal neovascularization . b) Posterior vitreous detachment Massive hemorrhage. c) Organization d) Retinal traction- detachment visual disturbance Eyes. ( Anterior chamber complications) . Cataract due accumulation of sorbitol 1 - Opacification of the lens nucleus (Osomotic effect of polyol pathway) 2 - Enhance of lens epithelial apoptosis Development of Neovascular membrane on iris surface: (a) Development of iris neovascular membrane. 1. (b) Increased levels of VEGF in the aqueous humor. 3. Neovascular glaucoma: (a) Proliferation of fibrovascular tissue in anterior chamber Contraction of neovascular membrane (b) Lead to adhesions. (c) Occluding a major pathway for aqueous outflow. (d) Elevation of the intra-ocular pressure IOP Nerves ( Diabetic Neuropathy ). • • 80% of DM> more than 15 years. • Site: Peripheral nerves , brain, and spinal cord. Site Autonomic neuropathy, e.g. genito-urinary & sexual, CVS symptoms and signs Peripheral neuropathy – sensorimotor neuropathy morphologic features- most common 1- Endoneurial arterioles show thickening, of BM with hyalinization,. 2- Demyelination resulting from Schwann cell dysfunction. 3- Axonal degeneration, with relative loss of small myelinated and unmyelinated fibers. Epidemiology, public health importance, prevention and screening (where applicable) of DM complications. • How Frequent? – – – – – – This disorder consider as very important public health problem 151 - 171 million of people worldwide. The overall prevalence of DM in adults in KSA is 23.7%. Male > female. 7% of the population, 1.5 million new cases\ year-USA. The prevalence is increasingly in the developing world as people adopt more sedentary life styles. • How to screen for diabetes, what the effectiveness of this screening and who to screen (all people or high risk group)? – 1- Meeting diagnostic criteria. (type 1,II, gestational, secondary, etc..) – 2- Screening test: OGTT=FBG >126mg\dl + (2-h OGTT) < 140mg/dl (normal), 140-199gm/dl (impaired), >200mg\dl (provisional diagnosis of DM). • Prevention: • Type II diabetes: – Exercise. – Loosing weight. – Diet control (high fiber, free of refined carbohydrates, based around vegetables). – Stopping smoking and alcohol intake. – Start medication early, stop some medications. • Type I diabetes: – Is an autoimmune condition. For this reason, it is not directly preventable. • _______________________________________________________ • Assessment of glycemic control regularly: • Measure Glycosylated hemoglobin% =HbA1C, which is formed by nonenzymatic covalent addition of glucose to hemoglobin in red cells. • The American Diabetic Association recommends that HbA1C be maintained below 6.5% in diabetic patients






