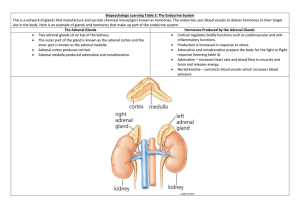
Adrenal cortex II
advertisement

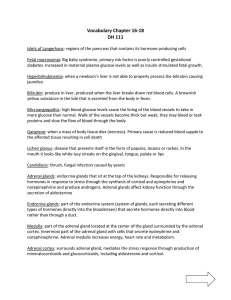
Pathology of Adrenal Cortex II Adrenal cortex Hyperadrenalism Excessive secretion of any one of the three basic types of corticosteroids gives rise to a distinct clinical syndrome: 1. Aldosterone – hyperaldosteronism (Conn’s syndrome) 2. Cortisol – Cushing’s syndrome 3. Androgens – adrenogenital syndromes Aldosterone is primarily involved with fluid and electrolyte balance. Aldosterone secretion causes sodium reabsorption in the distal renal tubule in exchange for potassium and hydrogen ions. The net effects are, fluid retention, decrease in plasma potassium and metabolic alkalosis. Hyperadrenalisms Adrenal cortex Primary Hyperaldosteronism Primary hyperaldosteronism – excess aldosterone secretion which is independent of the renin-angiotensin system (Conn’s syndrome) Causes: Aldosterone secreting adenoma Bilateral hyperplasia of the cortex Rarely carcinoma Clinical features: Hypertension, hypokalemia, sodium retention, muscle weakness, paraesthesia, ECG changes, cardiac decompensation Aldosterone, by inducing renal distal tubular reabsorption of sodium, enhances secretion of potassium and hydrogen ions, causing hypernatremia, hypokalemia, and metabolic alkalosis. Frequency: Prevalence for Conn syndrome; 0.05-2% of the population. Mortality/Morbidity: The morbidity and mortality associated with Conn syndrome, are primarily related to; 1- Hypertension, especially if left untreated for many years, can lead to many complications, including heart disease (eg, coronary artery disease, congestive heart failure), stroke, and intracerebral hemorrhage (with very high blood pressure). 2-Hypokalemia, especially if severe, causes cardiac arrhythmias, which can be fatal Age Peak incidence occurs in the third to sixth decades of life. Sex Primary hyperaldosteronism is twice as common in women as in men. II- 2ry hyperaldosteronism: There is increased renin-angiotensin with increased aldosterone secretion; -CHF -Liver cirrhosis and ascites -Nephrotic syndrome -Renal artery stenosis Clinical features Clinical suspicions should be raised when Hypertension occur with hypokalemia. Moderate to sever hypertension Hypokalemia Muscle weakness Malaise Polyuria polydipsia Investigations • Blood : Hypokalemia Plasma aldosterone • Urine : Increase urinary potassium • Imaging : U S CT MRI Iodocholesrerol isotope scan Adrenal vein sampling Treatment • Spironolactone • Adrenalectomy Congenital Adrenal Hyperplasia (CAH) By: Dr. Atif Ali Bashir Pathology Department Faculty of Medicine Majmaah University Congenital Adrenal Hyperplasia CAH refers to a group of disorders characterized by genital abornomalities due to deficiencies of the adrenal gland Causes Lack of an enzyme needed by the adrenal gland to make the hormones cortisol and aldosterone. Without these hormones, the body produces more androgen which is a type of male sex hormone. This causes male characteristics to appear early or inappropriately. Congenital Adrenal Hyperplasia The first case was described in 1865 Family of inherited disorders of adrenal steroidogenesis Each disorder results from a deficiency of one of several enzymes necessary for steroid synthesis Autosomal Recessive (M=F) 21-hydroxylase is the commonest form Location of Defective Gene CAH is caused by mutations of the CYP11B1 gene. The CYP11B1 gene is found on chromosomes 13 and 18 Congenital Adrenal Hyperplasia . Congenital Adrenal Hyperplasia CAH due to 21-Hydroxylase Deficiency 90–95% of CAH cases are caused by 21- OHD Females affected with severe, classic 21- OHD are exposed to excess androgens prenatally and are born with virilized external genitalia Symptoms Male Enlarged penis Failure to regain birth weight Weight loss Dehydration Vomiting Precocious puberty Rapid growth during childhood, but shorter than average final height. Female Ambiguous genitalia Failure to regain birth weight Weight loss Dehydration Vomiting Precocious puberty Rapid growth during childhood, but shorter than average final height. Infertility Irregular or absent menstruation Masculine characteristics Presentations of 21 HCAH Ambiguous genitalia in girls Dehydration Shock Salt-loss presentations with electrolytes imbalance Hyponatremia Hyperkalaemia Hypoglycemia Hyperpigementations . Symptoms Young woman with excess hair growth Baby girl with ambiguous genitalia. BOYS WITH CAH Are unrecognized at birth because their genitalia are normal. Present early with salt wasting crisis resulting in dehydration, hypotension, hyponatremia and hyperkalemia Or present later in childhood with early pubic hair, precocious puberty and accelerated growth Non classical CAH . Diagnosis Serum electrolytes & glucose Low Na & high K Fasting hypoglycemia Elevated serum urea due to associated dehydration Elevated plasma Renin & ACTH levels Low Cortisol High 17 – OHP High androgens especially testosterone level Low Aldosterone Urinary steroid profile Chromosomes Pelvic US Treatment To treat CAH, children are usually referred to a pediatric endocrinologist. Oral drugs are prescribed to boost the hormone levels Hydrocortisone and Dexamethasone are common meds to replace cortisol Fludrocortisone might be prescribed to replace aldosterone. Pedigree Chart CAH is autosomal recessive. This pedigree chart illustrates a child’s chances of inheriting the condition if both parents are carriers. Adrenal Neoplasms • Cortex: – Adenoma • Usually Non-Functioning – Carcinoma • Usually Functional • Medulla: – Pheochromocytoma – Neuroblastoma Adrenal Cortical Adenoma • F >> M 30-50 years of age • gross: well-circumscribed encapsulated nodule • solid yellow cut surface. Some have hemorrhage/cystic degeneration. Adrenal Cortical Adenoma Adrenal Adenoma Adrenal Cortical Carcinoma • wide age spectrum • often functional associated with hyperadrenalism • large, often >100 grams • gross: foci of hemorrhage, necrosis • micro: foci of necrosis, cytologic atypia, frequent mitoses, “solid” pattern Cortical Carcinoma Adrenal Carcinoma Pheochromocytoma • a tumor of adrenal medulla • 30-60 yrs.; F > M • rule of 10’s: 10% bilateral, malignant, occur in children, familial, extra-adrenal • Gross: solid, pale to light brown masses • clinical: hypertension, tachycardia, tremor, headache, sweating Pheochromocytoma Pheochromocytoma